The immune system may be viewed as one aspect of the lymphatic
advertisement

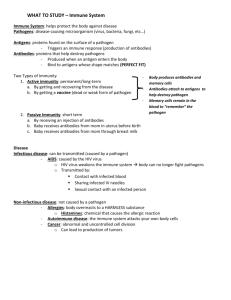
Immunity: innate versus adaptive Innate immunity: is non-specific (generalized response to threats) and short-term. 1. Skin and mucous membranes (airways, GI tract, e.g.) are barriers to entry by microbes. Low pH of gastric fluid destroys some microbes. The slight rise in body temperature (fever) that accompanies some illness may be enough to retard microbial reproduction. 2. Some cells may secrete chemicals that damage microbes: e.g. neutrophils, basophils, mast cells. 3. Activation of complement, which is a group of blood proteins that can damage microbes. See text for more information. 4. Inflammation, which involves #2, #3 above. This includes localized heat, swelling, redness; damaged tissue releases chemicals that recruit leukocytes to the site of injury to destroy microbes (formation of pus). Adaptive immunity: is specific (against a particular type of bacterium, virus, etc.) and long-lasting. The following is a greatly simplified summary of major points. This immune system may be viewed as one aspect of the lymphatic system. In text Figure 42.1, pg. 875, note the human body's extensive network of lymphatic ducts (vessels) and lymph nodes. Lymph, a fluid tissue containing leukocytes (WBC, white blood cells), moves in the ducts. WBC are also found in the bloodstream. WBC are the major players in immunity; they are constantly "on patrol," some even able to slip out of the bloodstream into surrounding tissues. 3 major functions of lymphatic system: A. Recovery of tissue water. With each heart contraction, some water is forced out of the bloodstream, through blood capillary walls, into surrounding tissues. That water returns to the bloodstream slowly via the lymphatic ducts; failure to recover that tissue water would lead to swelling of tissues, called edema. B. Dietary fat absorption. Whereas dietary carbohydrates, amino acids, minerals, and most vitamins are absorbed from the small intestine directly into the bloodstream, dietary fats pass first into the lymphatic ducts, and then into the bloodstream. See text Figure 51.15, pg. 1082. C. Immunity. Text Figure 42.1 also shows the thymus, spleen, and bone marrow as components of the immune system. Origin and variety of WBC: Text Figure 42.2 shows the many WBC types, each of which has a role in immunity, i.e. the body's immune response. Figure 42.2 also shows that stem cells in bone marrow give rise to WBC as well as platelets (= thrombocytes, required for blood clot formation) and erythrocytes (= RBC). Stem cells divide mitotically to produce (1) more stem cells, which remain in the marrow and (2) progenitor WBC, which are partially differentiated, not yet able to function in immunity. Contact with an infectious agent will stimulate these progenitor cells to complete their differentiation/maturation, to become functional, in various parts of the body such as thymus and spleen. In Figure 42.2 focus on macrophages and lymphocytes. These cells secrete (i.e. produce and release) cytokines, which serve as chemical signals (molecular communication) among the cells to coordinate the activities of WBC in the immune response. Macrophages have 2 roles: (1) to consume and destroy viruses and bacteria and (2) to act as antigen presenting cells. Lymphocytes are subdivided into B cells and T cells. Those are further subdivided by function, each playing a role in an immune response: B cells types: (1) Plasma cells secrete proteins called antibodies into blood, lymph; note that antibodies are not considered cytokines. (2) Memory B cells remain in blood/lymph after the current episode (threat/response) to provide quick response in case of subsequent exposure to the same infectious agent. T cell types: (1) Cytotoxic T cells release substances called reactive oxygen species (ROS,) that destroy virus-infected cells, tumor cells, foreign cells. These ROS are free radicals such as H2O2 and superoxide O2-. (2) Helper T cells release cytokines to organize activities of other lymphocytes. Helper T cells are the primary target of HIV; their destruction renders the immune system ineffective. (3) Suppressor T cells reduce the vigor of the immune response to return to "normal" after the infection. (4) Memory T cells remain in blood/lymph after the current episode (threat/response) to provide quick response in case of subsequent exposure to the same infectious agent. Depending on the type of threat (virus, bacterium, tumor cells, e.g.) the immune response will be primarily a B cell response (called humoral response, humoral immunity) or primarily a T cell response (called cellular response, cellular immunity). Aside from the obvious difference in the number of different kinds of cells involved, just listed), for our purposes the major difference is a matter of how cytotoxic T cells remove the threat versus how plasma cells (a type of B lymphocyte) remove the threat. Plasma cells do so by secreting antibodies, whereas cytotoxic T cells do so by secreting other types of toxic substances. Therefore, in the following story the role of antibodies is very important. Self versus nonself: The purpose of the immune system is to recognize, and protect against, agents that "don't belong" inside the body. Usually that means infectious agents such as bacteria and viruses. "Self" refers to the body's own cells; then "nonself" is everything else. A person's own cells have proteins on their surface that identify the cells as "self," that person's own cells. These are called MHC proteins, Major Histocompatibility Complex proteins. Their presence signals to WBC that the body's own cells are not a threat, not to be attacked. Sequence of events in immune response: The immune response is provoked by the entry of a foreign antigen into the body (into the bloodstream, e.g.). An antigen (adjective antigenic) is a protein that provokes an immune response. Even the body's own proteins on cell surfaces might do so were it not for the presence of the MHC proteins to signal otherwise. Thus, a foreign antigen would be a protein on the surface of a virus particle or on the surface of a bacterial cell or on the surface of cells of a transplanted organ. [Cells from another person would be recognized by your WBC as nonself and would be attacked, hence the failure of organ transplants if the recipient's immune system is not suppressed.] For illustration now, in the following sequence we'll suppose that the threat is a virus, with its capsid protein serving as the foreign (nonself) antigen. 1. Antigen challenge: An antigen presenting cell (APC) such as a macrophage bumps into the virus, recognizes its antigenic surface as alien, and consumes the virus by phagocytosis. It then displays fragments of the virus on its own surface. 2. These APCs bump into progenitor WBC, triggering them to divide mitotically to produce large numbers of fully differentiated lymphocytes; these are the B cell and T cell types listed above. 3a. Cytotoxic T cells destroy virus infected host cells. (Some cells will be infected before the WBC are marshaled in defense.) 3b. Plasma cells secrete antibodies, which bind to the virus particles outside cells. 4. As antibodies stick to (and cover) the virions' surface, that prevents virions from binding to host cells, thus no further infection of host cells. 5. As the masses of viruses bound to antibodies enlarge, the masses are engulfed and eliminated by macrophages. 6. These ongoing WBC activities are "coordinated" by cytokines released from helper T cells. As the viruses and virus-infected cells are eliminated, the suppressor T cells release cytokines that slow down the vigor of these activities, which includes stopping the cell division by progenitor WBC. 7. After this episode is done and the virus threat has been eliminated, memory B cells, memory T cells, and antibodies will remain resident in the bloodstream indefinitely as rapid protection against that same virus (foreign antigen) if it enters the body again. Specificity of response. Each foreign agent (virus, bacterium, etc.) has different surface antigens (proteins having different structure/shape). The immune response is specific for each type of antigen challenge. The antibody proteins that are produced and released by plasma cells are structured to recognize and bind to the specific antigen that provoked the immune response. So, for example, antibodies produced in response to one strain of flu virus will not recognize/bind to a different strain of flu virus. Since an antibody molecule is Y-shaped (see text Figure 42.9), with 2 antigen binding sites, each antibody molecule can bind 2 virions; and since each virion can bind many antibodies on its surface, the two bind in a "chain reaction," producing an enlarging mass. The specific binding of antigen to antibody is called agglutination. Memory cells also are specific for subsequently recognizing and responding to the antigen that provoked their production. Primary immunity versus secondary immunity. Primary immune response is the sequence of events described above. It takes some time for all of the WBC types to be generated in sufficient numbers and for enough antibodies to be secreted to effectively destroy the threat. For a bout of flu or common cold, e.g., this entire response may take 2 weeks. The early symptoms show that cells are being infected and killed as the virus reproduces and spreads within the tissues. The return of good health shows that the immune response has succeeded. If the same virus enters the body again later, as a rule no illness occurs because the memory cells and antibodies remaining from the first exposure respond immediately to destroy the threat; this is the secondary immune response that provides long term protection. Transplant rejection. Since immune system cells distinguish self from nonself and mount a defense against any nonself entity, that includes transplanted tissues. The cells of tissues transplanted from one person into another will lack the MHC surface proteins of the recipient. The recipient's immune system will recognize the transplanted cells (kidney, liver, etc.) as a threat and destroy them, causing "rejection" of the transplanted organ. Thus, after transplant surgery, the recipient must take drugs (cyclosporine, e.g.) that partially suppress his immune system: enough to prevent rejection of the organ while maintaining enough capacity to protect against infectious agents. That balance can be hard to maintain. This therapy is called immunosuppression and is life-long. If the drugs are discontinued, the immune system resumes full vigor and will attack the transplanted organ. Blood transfusion. (There is a separate assigned reading for this.) Autoimmune diseases ("immune to self"). For unknown reasons, sometimes the immune system loses the ability to recognize one's own tissues as "self." Perhaps the MHC surface proteins are lost or damaged. The result is an attack on one's own tissues. Lupus (affecting various organs), rheumatoid arthritis (affecting connective tissues), insulin-dependent diabetes (affecting the pancreas) are examples. Vaccination. Vaccination (synonym: immunization) is the act of treating with a vaccine. A vaccine is a preparation (usually a solution, to be injected or swallowed) that contains an attenuated (= weakened) form of an infectious agent. Under laboratory conditions, a purified preparation of a virus, e.g., can be treated by various chemical or physical means so as to render it harmless (unable to cause infection) but still sufficiently intact to provoke an immune response. Recall that WBC of the immune system recognize the surface proteins of a virus. If a lab treatment damages the viral nucleic acid but leaves the viral surface intact, WBC would still recognize the virus as a threat, even though it isn't a threat. And the WBC would respond as expected when the attenuated virus is injected into the body. So, vaccination provokes an immune response, without illness, leaving secondary immune protection against that infectious agent. When the actual infectious agent does enter the body later, memory cells and antibodies are already present to provide immediate response. Vaccination is prophylaxis, i.e. protection against disease. **Note that a major reason for the lack of a vaccine against HIV is the fact that HIV mutates often, such that its surface proteins change; a vaccine against one form of HIV may not work against other forms of HIV.** Vaccines are specific; each vaccine protects against a particular infectious agent, as a rule. Allergy. Antibodies are also called immunoglobulins, "Ig" for short, and are divided into 5 major groups: IgM, IgA, IgD, IgG, IgE (the acronym MADGE may help to remember them). Further, antigens that provoke an allergic response are called allergens. For unknown reasons, in some people IgE antibodies (produced in response to past exposure to allergens on pollen, mold spores, animal dander, etc.) bind their allergens, and then the two together provoke mast cells (found throughout the body) to secrete excessive quantities of irritant molecules such as histamine. Those substances then cause the familiar allergic symptoms. Antihistamines act by preventing/reducing production of histamine or by counteracting its effects. Active immunity versus passive immunity. The immune response described above is an active response of the immune system to foreign antigens; whether primary or secondary, it is still an active response of the body's immune system. Passive immunity refers to immunity that is acquired without the body's active participation. For example, a newborn baby gets some protection from (1) maternal antibodies in breastmilk and (2) maternal antibodies that previously passed through the placenta to the fetus. The newborn's own immune system is not yet functional. As another example, an adult may get some protection by receiving an injection of purified preformed antibodies. The disadvantage is that passive immunity is temporary; in time these "doses" of antibodies will be lost since the recipient's immune system hasn't been provoked to produce them.

![Immune Sys Quiz[1] - kyoussef-mci](http://s3.studylib.net/store/data/006621981_1-02033c62cab9330a6e1312a8f53a74c4-300x300.png)