HEMOBLASTOSES
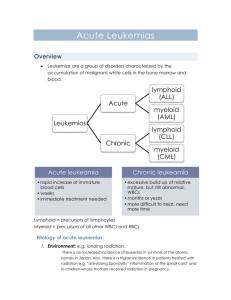
advertisement

STATE ESTABLISHMENT «DNEPROPETROVSK MEDICAL ACADEMY OF MINISTRY OF HEALTH UKRAINE » “Сonfirmed;” at methodical meeting of hospital pediatrics №1 department Сhief of department professor _____________V. A. Kondratyev “______” _________________ 2013 y. METHODICAL INSTRUCTIONS FOR STUDENTS` SELF-WORK WHILE PREPARING FOR PRACTICAL LESSONS Educational discipline module № Substantial module № Theme of the lesson Course Faculty pediatrics 2 10 HEMOBLASTOSES AT CHILDREN 5 medical Dnepropetrovsk, 2013. 1. Theme urgency: Hemoblastoses and leukemias for instance remain one of the most important problems of contemporary hematology. Childhood hemoblastosis has been diagnosed more often then other malignant diseases. Each tenth person, having hemoblastosis, is a child. Peak of disease incidence is mostly observed at age period of 2-5 years (80%). Prevalenceof hemoblastoses on the average makes 6-8 cases on 100.000 children's population per year. Hemoblastoses are a huge group of blood diseases of malignant origin, which is interpreted as malignant neoplasms of lymphatic and blood tissues. Hemoblastoses are divided into 2 main groups: leukemias and malignant lymphomas depending upon systemic or regional affectionof blood tissue. Acute lymphoblastic leukemia (ALL) is the most prevalent form of childhood hemoblastosis; it is registered with frequency of 3-5 children on 100 000 children's population per year. ALL represents about 30% of all oncology diseases. More often this disease is observed at 3-5 years of age. ALL morbidity in this age group is 10 times more often registered than morbidity in other age groups. Acute myeloid leukemias are less prevalent childhood malignancies: its prevalence is 0,7 cases per 100.000 children population per year on average. Chronic myeloleukemia – is malignant disease of blood system, which is originated from myeloid sprout of blood production. Granulocytes, predominantly mature forms, are main tumor pathological components. In childhood chronic myeloleukemia is observed at 25% cases of leukemia and is the only malignant process, which has precise chromosome disorders. Hodgkin`s disease is malignant neoplastic disease of lymphatic system. Childhood Hodgkin`s disease takes second place in prevalence after acute leukemia among hemoblastosis and first place among malignant lymphomas. In childhood and youth age periods lethality among hemoblastoses achieves 50% of all amount of lethal cases in oncology. So all this statements proves urgency of learning current theme. 2. Specific purposes А. Student has to know: 1. Definition of term «hemoblastosis». 2. Classification of childhood hemoblastosis. 3. Definition of terms “leukemia”, " myeloleukemia ", “ myeloleukemia ” 4. Contemporary classifications of leukemia, myeloleukemia, myeloleukemia at children. 5. Etiopathogenetical features of the development of leukemia, myeloleukemia and Hodgkin`s disease at children. 6. Clinical findings consistent with different variants of hemoblastosis course at children. 7. Cytomorphological forms of hemoblastosis at children - Acute lymphoblastic leukemia - Acute mieloblastic leukemia - Acute monoblastic leukemia. - Acute mielomonoblastic leukemia - Acute erithroleukemia. - Chronic leukemia - Hodgkin`s disease 8. Clinical and laboratory diagnostic criteria of hemoblastosis at children. 9. Principles of management of different forms of childhood hemoblastoses. 10. Outcomes of different forms of hemoblastoses at children. 2 В. Student should be able: 1. To develop the scheme of diagnostic search at blood disease. 2. To take history of patient, having blood disease.. 3. To carry out objective investigation of the patient. 4. To evaluate the laboratory data. To choose from analyses the data, which confirm hemoblastosis. 5. To be able to reveal clinical criteria of the diagnosis at different clinical forms of hemoblastoses. 6. To formulate the developed clinical diagnosis according to classification 7. To make differential diagnostics with other blood diseases at children. 8. To appoint treatment, taking into account the clinical form of disease.. 9. Principles of prophylaxis of disease recurrence. 10. To use deontological principles during collecting of the anamnesis, objective investigation of the sick child. 3. Tasks for students` self-dependent work during preparation for the classes. 3.1. List of main terms, parameters, characteristics, which students has to master preparing for the classes. Term 1. Hemoblastoses 2. Leukemias 3. Malignant lymphomas (hematosarcomas) 4. Acute leukemia 5. Chronic leukemia Definition The big group of blood diseases of tumorous origin, or a neoplasm of lymphatic and hematopoietic tissue. Malignant tumorous diseases of hematopoietic system with primary localisation in a marrow. Group of diseases which belongs to primary localised tumours of lymphatic system. Disease at which there is a tumorous transformation and impetuous growth of young blast cells. Disease at which development of tumorous cells reaches to differentiated mature (or ripened) forms: plasmocytes, red (blood) cells, lymphocytes. Leukemia with tumorous transformation and impetuous growth of young blast cells. Leukemia, with insufficiency of marrowy hematopoiesis caused by replacement of normal hematopoietic cells by malignant cells. Malignant lymphoma which affects not only lymphatic system, but also can affect nonlymphatic organs and tissues. Not specific for lymphogranulomatosis tumorous cells. 6. Acute lymphoblastic leukemia 7. Acute mieloblastic leukemia 8.Lymphogranulomatosis, Hodgkin`s disease 9.Uninuclear Hodgkin`s cells 10.Polynuclear Sternberg- Specific for lymphogranulomatosis tumorous cells. Reeds cells 3.2. Theoretical questions for the classes 1. Definition of terms «hemoblastosis», “leukemia”, " myeloleukemia ", “ Hodgkin`s disease” 2. Contemporary classifications of hemoblastosis, leukemia, myeloleukemia, Hodgkin`s disease at children. 3 3. Etiopathogenetical features of the development of leukemia, myeloleukemia and Hodgkin`s disease in childhood. 4. Clinical manifestations of different variants of outcomes of childhood hemoblastoses. 5. Clinical, laboratory and diagnostic criteria of hemoblastosis at children. 6. Principles of management of different forms of hemoblastoses at children. 7. Outcomes of different forms of hemoblastoses at children. 3.3. Practical skills (tasks) mastering during practical lesson: 1. To collect complaints, case history and personal (life) history 2. To inspect the child consistently 3. To reveal early symptoms of the disease 4. To reveal the signs of complications of the disease 5. To evaluate the condition of the child and available clinical symptoms. 6. To evaluate the results of the additional methods of investigation 7. To make the clinical diagnosis according to classification. 8. To make the treatment plan according to the protocol. 9. To make recommendations of dispensary supervision. 3. Maintenance of the subject: 5.1 . Hemoblastoses at children. 1 . Definition: Hemoblastoses – is the term for definition of the tumors originating from the hematopoietic cells. In clinical concept hemoblastoses are a big group of blood malignant diseases. 2 . Classification of hemoblastoses at children. Depending on the systemic or regional disorder of the hematopoietic tissue hemoblastoses are subdivided into such main groups: Leukemias - malignant diseases of the hematopoietic system with primary localization in marrow and spreading into organs and systems: - acute leukemia - a disease at which there is a tumoral transformation and impetuous growth of young blast cells. The substratum of the tumor represents hematopoietic cells of the first four rows of the modern scheme of hematopoiesis, mature cells ripen also. - chronic leukemia is the disease at which there is development of tumoral cells reaches differentiated mature (or that ripen) forms: plasmocites, erythrocytes, lymphocytes. Malignant lymphomas (non Hodgkin lymphoma, hematosarcomas) are the group of diseases which belong to initially localized tumors of lymphatic system Lymphogranulomatosis (or Hodgkin's desease) – a malignant lymphoma which affects lymphatic system with the following tumoral changes of not lymphatic tissues and organs. Specific to the Hodgkin's disease one-nuclear tumoral Hodgkin cells and multinuclear cells of Berezovsky-Rid-Shternberg are considered. 3 . Classification of acute leukemias. Cytochemical features of the blast cellsare put in the basis of classification of acute leukemias I. Clinical-morphological variants of acute leukemia at children: - lymphoblastic - myeloblastic - monoblastic - mieelomonoblastic 4 - promielocytic - erythromielosis - undifferentiated form ІІ. Periods of the diseasae: - initial stage - period of the full development of the disease - remission period - period of recurrence of the disease - terminal period III. Forms depending on quantity of leukocytes in peripheral blood: - leukemic form (L >50x109/l); - subleukemic form (L = 10-50x109/l); - leukopenic form (L <5x109/l); - aleukemic form (L>1x109/l); . 5.2 . Acute lymphoblastic leukemia at children. Code ICD-X C 91.0 1 . Definition: Acute lymphoblastic leukemia (lymphoid form of acute leukemia) - a disease at which there is a tumoral transformation and impetuous growth of young blast cells. The substratum of the tumor represents hematopoietic cells of the first four rows of the modern scheme of hematopoiesis, mature cells ripen also. Acute lymphoblastic leukemia is the most widespread tumor of children's age; it is registered with a frequency of 3-5 per 100 000 and represents about 30% of all oncologic diseases, the lymphoid variant of acute leukemia is prevalent at 82,3% cases, (myeloid variants - 17,7% of cases). Most often this disease develops at children of 3-5 years old. Incidence on ALL in this age group is seen by 10 times more often than in other age groups. 2. Classification of lymphoid form of acute leukemia: Cytological types: 1 . L1 - small lymphoblasts with small amount of cytoplasm; 2 . L2 - big lymphoblasts with the large amount of cytoplasm, changed nuclear membrane; 3 . L3 - lymphoblasts with characteristic cytoplasmic vacuolisation . Immunological subtypes: 1. T-ALL (13%) T - cellular acute lymphoblastic leukemia; 2. B-ALL (3%) B - cellular acute lymphoblastic leukemia; 3. Pre-B-ALL (16%) Pre-B-cellular acute lymphoblastic leukemia; 4. Pre-Pre-B-ALL (5%) Pre-Pre-B-cellular acute lymphoblastic leukemia; 5. "common" ALL (52%) - on the blast surface markers of both B- and T-cells 3. Etiopathogenetic theories of the development of a leukemia at children: - Endogenous (exchange) chemical theory of leukemia. - Role of ionizing radiation. - Virus theory. - Genetic theory. - Tumoral theory. 4 . Etiopathogenetic mechanisms: 1 . The clonal origin of leukemia, i.e. develops from one pathological cell owing to tumoral progression: - monoclonal benign tumor transforms into polyclonal malignant tumor; - polyclonal malignant tumor quickly metastasizes; 2 . Disorders of cellular differentiation (maturing): 5 - uncontrollable reproduction of malignant (leukemic) cells-precursors of lymphoid cells in marrow; - its subsequent distribution by blood and by lymphatic vessels - deppression of marrow hematopoiesis with the development of anemia, thrombocytopenia and a neutropenia; 3 . Disorders of cellular proliferation - development of proliferative syndrome, manifested by generalized enlargement of lymph nodes and hepatosplenomegaly. 5 . Periods of the disease: initial period, complete development of the disease, remission period, period of recurrence of the disease and terminal. Initial period of acute leukemia - can begin with the signs resembling acute respiratory viral infections, tonsilitis, rheumatic fever, anemia and others; - small symptoms: quick fatigue, weakness, deterioration of the appetite, high fever, a general malaise, muscular pain, catarrhal phenomena in the form of hyperemia of the pharynx, rhinitis or conjunctivitis. - necrotic form of tonsilitis, ulcer necrotic stomatitis, its recurrence and resistance to antibiotics. - muscle, bone and joint pain, can be intensive, enhancing at night - increasing paleness and enlargement of peripheral lymph nodes: cervical, submaxillary lymph nodes; they are mobile, painless at palpation, skin over them isn't changed. - affection of salivary glands (Mikulich's symptom) that is characterized by bilateral swelling of the parotid glands; salivary glands can also be involved. - hemorrhagic syndrome which is caused by thrombocytopenia: single hemorrhages of different form and size, rarely – profound bleedings, blood in the stool. - some children have neurologic symptoms: fatigue, weakness, drowsiness, headache, emotional lability, disorders of memory and attention; paresis of facial nerve, nistagmus, positive meningeal symptoms. - leucopenia or leucocytosis with lymphocytosis, a tendency to the thrombocytopenia, accelerated ESR; - further - emergence in peripheral blood of young, blast cells. - in marrow - blast cells more than 30%. Period of complete development of acute leukemia. - characterized by progressing of symptoms of an initial stage of the disease, and also occurrence of new symptoms; - symptoms of leukemic intoxication progress: weakness, apathy, decreased appetite, vomiting. The most constant symptoms of this period: - febrile fever of the wrong type. - paleness of skin; leucemides at skin - dense hemorrhagic infiltrates, eczema-like rash, exudative erythema, urticaria, pemphigus; - considerable necrotic changes of the mucous membranes; - hyperplasia of peripheral lymph nodes, spleen and liver (less often). - progressing hemorrhagic syndrome: hemorrhages into skin, mucous membranes, nasal, intestinal bleedings, hemorrhages into conjunctiva, fundus of eye. - bone system: pain in bones and joints (50%); osteoporosis, osteosclerosis, osteolysis, periostal reactions. - cardiovascular disorders: tachycardia, expansion of the heart borders, systolic murmur, ECG changes. - respiratory tract: focal pneumonic infiltrates, cavities, pleuritis. - complete blood count: progressing hypochtomic anemia, thrombocytopenia, accelerated ESR. 6 - leukocyte formula - leukocytosis, blast cells (lymphoblasts, myeloblasts, reticulocytes); "leukemic hole" - lack of intermediate forms of the myeloid cells; - 80-100% of immature, blast forms in liquor. Period of remission of acute leukemia. Remission is the absence of clinical-hematologic signs of acute leukemia. Existence of prolong remission (more than 5 years) that can be achieved at 50% of patients allows to establish the recovery of the disease. Staging of marrow hematopoietic disorders 1. For the first 10 days of treatment develops moderate cytopenia with disappearance of blast cells from peripheral blood. 2. Further there is appears hypoplasia of marrow hematopoiesis. 3. In 3-4 weeks there are noted the signs of its regeneration with increase of quantity of platelets, leukocytes, reticulocytes. 4. In 6 weeks from the initiation of treatment the normal hematopoiesis is restored that confirms the occurrence of remission. Criteria of clinical-hematologic remission of acute leukemia: - absence of clinical symptoms of acute leukemia not less than 1 month; - in mielogramme no more than 5% of blasts and lymphocytes no more than 30%; - restoration of a ratio of an erythrocyte-granulocyte cells 1:3 and of megakaryocytic cells; - normalization of complete blood count (Hb >120g/l, leukocytes >4x109/l, platelets >100x109/l; - absence of blast cells in peripheral blood. Recurrence of clinical-hematological manifestations of the disease is defined as the recurrence of acute leukemia which can turn into terminal stage. 6 . Diagnostics (obligatory diagnostic investigations): - marrow puncture with cytologic, cytochemical, imunocytological and moleculargenetic investigation of leukemic (blast) cells; - morphological investigation of peripheral blood for the presence of blast cells; - lumbar puncture for the counting of quantity of cells in liquor; - presence of 25% and more blast cells in marrow is confirmatory sign of acute lymphoblastic lyukemia.. 7 . Treatment of acure leukemia. The purpose of therapy is the maximum destruction of tumoral cells by eradicating polychemotherapy. Therapy stages irrespective of the variant of the disease: therapy of an induction and remission consolidation, prevention of neuroleukemia and treatment in the remission period, at least 2-3 years. The first stage - an induction of remission, Drug therapy is depending upon the lymphoid or myeloid form of a acute leukemia, aggressiveness of the process. In the period of an induction of remission neuroleukemia prevention is carried out. The second stage - consolidation (strengthening) of remission or consolidating therapy - the additional course of chemotherapy directed on destruction of leukemic infiltrates, of neuroleukemia, with endolumbal introduction of cytostatics and radial therapy at skull area. The third stage - maintenance therapy with the courses of reinduction - Maintenance therapy keeps under control pathological tumoral substratum, 107-109 tumoral cells which are in the rest phase which decreases due to death of cells. - At decrease in leukemic population of cells to 105-106 pathological process can be controlled by the organism independently, there could be reached recovery. - Depending on the remission term each 1-3 months reinduction courses are performed. 7 Therapeutic schemes of a sharp leukosis. The BFM program – the most effective program of cytostatic therapy of acute limphoblastic leukemia which is directed on destruction of the tumoral clone, duration - 6 months of intensive protocols; then maintenance therapy for 2 years. Low risk patients are treated according to the protocol N 1. Protocol No. 1. First phase. 1 . Prednisone - 60 mg/sq.m per os 2 . Vincristin - 1,5 mg/sq.m intravenously and rubomycin - 30 mg/sq.m intravenously for 1 hour at 8, 15, 22, 29th day of treatment; 3 . L-asparginaze - 10 000 U/sq.m intravenously for 1 hour 1 time in 3 days, since 12th day of therapy; 4 . The methotrexate is entered intrathecally for the prevention of neuroleukemia 1 time in 2 weeks in age dose - till 1 year - 6 mg, - 1-2 years - 8 mg, - 2-3 years - 10 mg, - > 3 years - 12 mg. ; 5 . At neuroleukemia - the methotrexate is entered intrathecally 5 times at a week. Second phase. 1 . Cyclofosfan 1g/sq.m intravenously at 36 and 64 days of treatment with uroprotector uromithexan in the total dose of 1000 mg/sq.m 0,4 and 8 hours after administration of cyclofosfan; 2 . Cytozar – 75 mg/sq.m; 3 . 6-merkaptopurin - 60 mg/sq.m per os from 36 to 64 days of therapy. 4 . Accompanying therapy: a) Decontamination of intestines (polimixin, nystatin). b) Oral cavity sanation. 5 . Prevention of hyperuricemia a) Allopurinol - 10 mg/kg for 3 - 8 days. b) Infusional therapy with urine alkalization. c) Biseptol - 3-5 mg/kg of 1 times in 2 days from 36 to 64 day. 6 . Control of efficiency of therapy is performed by continuous control of temperature, diuresis, stool, weight, blood analyses, electrolytes and hepatic enzymes, Creactive protein, coagulogram, electrocardiogram. Marrow puncture should be carry out at the 8th and 33rd day. Therapy of the patients of moderate risk by the protocol No. 1 Prednisolonum is administered according to the scheme: - 1st day - Prednisolonum is entered at 1/3 of full dose, - 2nd day - Prednisolonum are entered at 1/2 of full dose, - 3rd day - the full dose - 60 mg/sq.m is given. Replacement therapy: 1 . Erythrocytes - 10-15 mg/kg if Hb is less than 90 g/l. 2 . Thrombocytes - 1 dose / 10 kg if platelets are less than 20x109/l. After the termination of the protocol, in case of achievement of remission the child is discharged. Protocol M. 1.6-merkaptopurin is entered per os in a dose of 25 mg/sq.m per day. 2 . Methotrexate – 1g/sq.m in 36 hours intravenously with 5% glucose solution 3 . Cyclofosfan - 15 mg/sq.m intravenously 4 . If pH decreases sodium bicarbonatis is administered for the decrease in methotrexate toxicity. 8 5 . In 2 hours - methotrexate intrathecally (for the prevention of neuroleukemia). 6 . After administration of the listed preparations antidotes (uromithexan and leukoverin - 15 mg/sq.m) and massive antibacterial therapy are prescribed. Therapy of patients of high risk group. Survival in this group of patients is about 30-40%. For this group of patients transplantation of marrow which increases quality of treatment is supposed. Allogenic transplantation of marrow. At patients with the extremely unfavorable prognosis (the presence of adverse chromosomal anomalies, prognostic unfavorable factors and the poor answer to the standard chemotherapy) allogenic transplantation should be carried out in the remission stage: - allogenic transplantation of marrow should be performed at patients with adverse chromosomal anomalies of t (9; 22) and t (4; 11) -other indications for allogenic transplantation are combination of several adverse factors, including the T-cellular phenotype, bad answer to an initial prednisone phase of treatment, and the absence of full hematologic remission after end of the I phase of the Protocol I. 5.3 . Acute myeloid leukemia at children. ICD-X C 92.0 - 94.0 1 . Definition: Acute myeloid leukosis (myeloid form of acute leukemia) - a leukemia which characteristic sign of insufficiency of marrow hematopoiesis owing to the replacement of normal hematopoietic cells by malignant cells with uncontrollable reproduction of leukemic cells precursors of a myeloid line in marrow with the following their distribution by a hematogenous way. Acute myeloid leukemias belong to the widespread oncologic diseases at children with average prevalence 0,7 cases per 100 000 children's population in a year. Myeloid variants acute leukemia are about 17,7%, (lymphoid - 82,3%). 2 . Classification of myeloid form of acute leukemia: The definition "acute mieloleukemias" unites the group of diseases which (according to modern modernized FAB-classification system) are divided on 8 clinical variants (subtypes): Cytologic subtype: 1 . M0 - acute undifferentiated myeloid leukemia (2%) 2 . M1 - acute myeloblastic leukemia with differentiation (25%) 4 . M3 - acute promyelocytic leukemia (10%) 5 . M4 - acute myelomonocytic leukemia (30%) 6 . M5 - acute monocytic leukemia (10%): - М5а - monoblasts, - М5b - promonocytes. 7 . M6 - acute erythromyelosis (4%) 8 . M7 - acute megakarioblastic leukemia (1%) 3 . Etiopathological mechanisms: - Mechanism of these diseases - uncontrollable reproduction of malignant (leukemic) cells precursors of a myeloid line in marrow with the following their distribution by a hematogenous way. - The most characteristic sign of acute myeloleukemia is marrow insufficiency owing to replacement of normal hematopoietic cells by malignant cells which manifests wirh anemia, thrombocytopenia and neutropenia with the corresponding clinical manifestations. - Proliferative syndrome is specific only for several variants of the disease (monoblastic leukemia, myelomonoblastic leukemia) and is manifested by hepatosplenomegaly because leukemic cells have tropism to the reticuloendotelial system. 9 4 . Clinical diagnostics of acute myeloid leukemia. 4.1 . Very severe course, full and permanent remissions are rarely observed. 4.2 . Specific syndromes: intoxicational, anemic, hemorrhagic, rare - hepatoliyenal. 4.3 . Specific signs: infiltration of kidneys, skin, gingiva, etc. 4.4 . Peripheral blood: severe anemia and thrombocytopenia, eosinophilia, leucositosis. Leukogram – a left shift to the myeloblasts. 4.5 . Marrow aspirate - a total infiltration by myeloblasts. 4.6 . Urgent conditions: - uncontrollable bleedings, - and/or with hemorrhages into internal organs, - with severe infections, sepsis with septic shock. Obligatory diagnostic actions are the marrow puncture with the following cytological, cytochemical, imunocytological and molecular and genetic investigations of the leukemic (blast) cells. The definition in marrow aspirate more than 20% of leukemic cells is confirmatory feature for the establishment of the diagnosis of acute myeloid leukemia. 5 . Treatment. - treatment of acute myeloid leukemia. The BFM protocol of treatment of acute myeloid leukemia at children: 1 . Induction phase - 8 days: - Cytozar in standard dose - 8 days; - Rubomycin 30 mg/sq.m twice a day at the 3, 4, 5 days; - Etopozid - 150 mg/sq.m once a day at the 6, 7, 8 days. 2 . Phase remission consolidation: - begins after the break in 2-4 weeks and lasts for 6 weeks preparations: cyclophosphan, cytozar, vincristin, adriamycin, 6-merkaptopurin, prednisone; - after termination of the intensive phase of treatment patients receive cranial radiation in a dose 18 Gr. 3 . Supported therapy - lasts about 1,5 years: - 6-merkaptopurin once a day - 40¼ú/sq.m; - cytozar every month - 40 mg/sq.m in/in for 4 days. 4 . Maintenance therapy - Total decontamination of intestines, constant transfusions thromboconcentrate and erythrocytes, preventive and medical applications of wide spectrum antibiotics, antimycotic preparations, antiviral drugs, hepatoprotectors, kardiotrophic drugs and enzymes, if necessary –partial or total parenteral nutrition. - Allogenic (if HLA-matched donor is present) or autological transplantation of stem cells should be performed in the first remission of the disease at patients of high risk group. - Lethality level during chemotherapy of acute myeloid leukemia can achieve up to 10%, level of a survival achieve up to 50%. -Treatment of a chronic myeloid leukemia. The main drugs for the treatment of chronic myeloid leukemia are myelosan or myelobromol. Doses of preparations depend upon clinical-hematologic parameters at the initiation of treatment. Prevention of blast crisis can be achieved by the appointment of 6-MP (50mg/sq.m) 2-3 times a week. In acute phase of CML the combined polychemotherapy is appointed, similar to the therapy of acute leukemia. Marrow transplantation and immunotherapy should be administered at appropriate indications. 10 Interferon is appointed during remission. Introduction of human interferon and reaferon (1-3 million IU in/m for 1-2 weeks) increases duration of remission and survival of patients. 5.4 . Lymphogranulomatosis at children. ICD-X C 81 1 . Definition: Lymphogranulomatosis (or Hodgkin's disease) belongs to the group of malignant lymphomas and affects mainly lymphatic system, but can affect nonlymphatic organs and tissues also. Hodgkin's one-nuclear tumoral cells and Berezovsky-Shternberg multinuclear cells which are specific for the disease are found in histological preparations of the affected tissues. 2 . Classification Histological classification. According to the histological classification there are four main types of lymphogranulomatosis according to the content of different cells in the specific granuloma: - lymphocyte-rich (lymphocytic predominant) – nodular or diffuse - nodular sclerosing HL (1 and 2 types by degree of malignancy); - mixed-cellularity subtype; - lymphocyte depleted. Clinical classification of lymphogranulomatosis. 1 stage (localized) - the disease is limited to one group of lymph nodes or two adjacent, located at one party of a diaphragm; 2 stage (regional) - involvement of 2 or more lymph node areas on the same side of the diaphragm 3 stage (generalized) - a disease extends on both sides of the diaphragm, but within lymphatic system with affection of lymph nodes, thymic gland, lymphatic pharyngeal ring, spleen (designated "by S +"). 4 stage (disseminated) - is characterized by involvement of extranodal organs (+): lungs - L, liver - H, kidneys, gastrointestinal tract, pleura - P, skin - D, bones - B, marrow M, lymph nodes - N. A or B designations denote the absence or presence of B symptoms. A "B" designation includes the presence of 1 or more of the following: - Fever (temperature >38°C) more than 5 days or prolong subfebrile fever ; - Drenching night sweats - generalized itching; Unexplained loss of more than 10% of body weight within the preceding 6 months An "A" designation is the absence of the above. Signs of biological activity of process a) - absence of signs of biological activity of process; b) - presence of signs of biological activity: - ESR more than 30-40 mm/hour; - leucocytosis more than 12-15х109; - serum iron less than 12 µmol/l; - fibrinogen more than 5 g/l; - albumine less than 35%; - 2-a globulines more than 12%. Example of the diagnosis: Lymphogranulomatosis. IV N + S+ M+ L+ P-D-O. 3 . Clinical diagnostics of lymphogranulomatosis - According to the Ann Arbor classification (see above) there are four stages of the disease which subdivided into categories A and B depending on absence (A) or existence (B) the 11 symptoms of the general intoxication: loss of weight ≥10% for the last 6 months and/or constant or persistent fever >380C and/or is increased sweating at night. - Leading symptoms are painless enlargement of lymph nodes, most often, of cervical (7080%) and mediastinal groups (15-20%), which are formed into conglomerates packages, with following possible compression of adjacent organs (trachea, bronchus or vessels). Liver and spleen can increase in size also. - Involvement of extranodal structures can manifest in the form of tumor, exudate, pain, and disorders of functions of internal organs. 4 . Paraclinical diagnostics of lymphogranulomatosis: - biopsi of the affected lymph node (advantage is provided to the excisional biopsy of the lymph node which gives opportunity to study its architectonics) - studying of the cytological preparations received during a marrow or other nonlymphatic organs puncture aren't sufficient for the definition of their affection - trepatobiopcy is essential for the for establishment of the IV stage of the disease owing to marrow affection Affected tissues are investigated cytologically (prints), histologically, immunohistochemically and also in doubtful cases (for differential diagnostics with non Hodgkin lymphomas), by molecular and genetic methods. - In cases of massive mediastinal tumor and in the case of possible life-threatening breathing disturbances biopsy is carried out under local anesthesia or after the previous treatment with corticosteroids. 5 . Treatment of lymphogranulomatosis - Polychemotherapy in combination with irradiation of initially affected regions. - The most effective for children and the least dangerous from the point of view of the remote consequences are schemes OEPA/OPPA and COPP (DAL-HD-90 and GPOH-HD-95 protocols). Necessary quantity of cycles depend upon the stage of the disease and the presence of involvement of not lymphoid bodies. - Depending on the quantity of polychemotherapy cycles the cumulative dose of irradiation of the affected are planned. Irradiation of the initially affected lungs and liver isn't carried out. - The decision on the volume of irradiation therapy (zones and a irradiation dose) has to be accepted right after establishment of the diagnosis and definition of the stage of the disease together with the hematologist (children oncologist) and the doctor-radiotherapist. Accompanying treatment: - Provides minimization of the possible infectious complications caused both by development of clinically significant neutropenia, and considerable degree of the immunosupression which remains for 6 months after termination of the treatment, at spleen irradiation - more than 1-1,5 years after its carrying out. - Administration of oral cotrimoxazol, antifungal preparations, bacterial decontamination (is neutropenia is possible), preventive use of acyclovir at decrease in absolute level of lymphocytes (<300/mcl), careful hygienic recommendations for the oral cavity and others mucous membranes cleaning are obligatory therapeutic measures for such patients. Remission is defined after normalization of the size of initially increased groups of lymph nodes, liver, spleen. Monitoring of initially affected zones is carried out each three months for the first two years after termination of treatment, every 6 months on the 3rd and 4th year, and then – at suspicion for the disease recurrence. 12 Additional materials for the self-control А. Clinical cases Case 1 A2 year old girl presented to her general practitioner after several weeks of being, in her mother’s words, "tired and just not herself," preceded by several months of recurrent upper respiratory tract infections. After positive urinalysis, the general practitioner diagnosed a urinary tract infection. Despite repeated treatment with oral antibiotics, she developed four further urinary tract infections over the next two months. At this time—four months after the initial onset of symptoms—the mother noticed her daughter was pale and lethargic. Over the coming few weeks, she also observed the child’s skin become yellow in colour. Eventually, when her daughter rapidly developed fever, night sweats, and joint pain severe enough to prevent walking, the mother made an emergency appointment at her general practice. The toddler was sent urgently to hospital, where examination elicited hepatosplenomegaly and cervical lymphadenopathy. On admission, she was pancytopenic (haemoglobin 28 g/l, white blood cell count 0.89x109/l, platelets 120x109/l). The blood film confirmed pancytopenia, with occasional teardrop cells but no immature lymphoid cells. Questions 1. What is the most possible diagnosis? 2. What other conditions would you include in your differential and why? 2 What are the potential life threatening complications in patients presenting with acute leukaemia? 3 How would you make a definitive diagnosis? 4 How might acute leukaemia lead to jaundice? 5 What is the likely prognosis for this child? Case 2 A 17-year-old boy presents on a winter day for "ED follow-up" and anemia. He reports 3 days of fever, nasal congestion, weakness, and cough. He had been seen in the ED the previous night and had a viral infection diagnosed. A history of anemia led the ED physician to measure Hgb, which was 9 g/dL (90 g/L). The clinic chart reveals a 3-kg weight loss over the past 12 months. An office Hgb assessment was 12.3 g/dL (123 g/L) 1 year ago, and he was started on iron tablets, which he takes inconsistently. Earlier in the winter, he felt that his lungs had decreased capacity during band practice. These symptoms lasted 1 month, then resolved. He has felt well for 2 weeks prior to his current illness. Physical examination reveals a thin, friendly boy. His weight is 60.5 kg, temperature is 37.4°C, and blood pressure is 108/66 mm Hg. His ears and throat are clear. Lungs are clear to auscultation. Heart rate is elevated at 123 beats/min, but results of the cardiac examination are otherwise normal. His abdomen is soft, nontender, and free of hepatosplenomegaly or masses. There is no lymphadenopathy in the cervical, supraclavicular, axillary, or inguinal areas. His Hgb is 9 g/dL (90 g/L), WBC count is 3.7x103/mcL (3.7x109/L), platelet count is 3 474x10 /mcL (474x109/L), mean corpuscular volume is low at 65 fL, and reticulocyte count is 1.5%. His serum iron value is low at 24 mcg/dL (4.3 mcmol/L) (normal, 40 to 170 mcg/dL [7.2 to 30.4 mcmol/L]) and ferritin concentration is high at 569 ng/mL (1,278.5 pmol/L) (normal, 7 to 282 ng/mL [15.7 to 633.7 pmol/L]). His ESR is elevated at 80 mm/hr. Findings on urinalysis are normal, and stool is negative for occult blood. The history of respiratory symptoms and weight loss warranted a chest radiograph, which revealed a large right-sided anterior mediastinal mass. CT scan of the chest showed a homogenous soft-tissue mass, which displaced the superior vena cava and heart to the left. Positron emission tomography scan demonstrated no sites of metastases outside the mediastinum. 13 Questions 1. What is the most possible diagnosis? 2. What other conditions would you include in your differential and why? 3 How would you make a definitive diagnosis? 4. How to treat this disorder? Case 3 A 6-year-old boy who has Down syndrome presents with a 2-day history of fever (temperature to 39.0°C) and a painful limp and favoring of his right leg. During the past 2 weeks, he has had decreased appetite, increased pallor, and increased bruises on his upper and lower extremities. Physical examination reveals pallor and multiple ecchymoses on his arms, legs, and trunk. Bilateral cervical and supraclavicular lymph nodes are palpable; the nodes are firm, nontender, and 1 to 2 cm in size. The liver is palpable 3 cm below the right costal margin, and the spleen is palpable 2 cm below the left costal margin. Tenderness is elicited over the right distal femur. Radiographs of the right distal femur reveal osteopenia plus a small lytic lesion. A chest radiograph shows normal results with no mediastinal mass or pulmonary infiltrate. His white blood cell count is 2.8_103/mcL (2.8_109/L) with 10% neutrophils, 5% monocytes, 85% lymphocytes, and no blasts. His hemoglobin measures 8.2 g/dL (82 g/L) and platelet count is 38_103/mcL (38_109/L). Due to the presence of severe neutropenia with fever, intravenous broad-spectrum antibiotics are administered after blood cultures are obtained. The child is referred to a pediatric hematologist/oncologist, and a bone marrow aspirate and biopsy demonstrate more than 90% lymphoblasts. Questions 1. What is the definitive diagnosis? 2. What are the principles of treatment? 3. What are the possible adverse effects of the chemotherapy? 4. What is the likely prognosis for this child? B. Tests Question 1. A 14-yr-old girl presents with bilateral cervical lymphadenopathy that has progressed over the last 4 wk. It is slowly worsening despite antibiotic therapy with cephalexin, which was prescribed 2 wk ago. On physical examination, the lymph nodes are enlarged, matted, and nontender. There is mild splenomegaly. The most likely diagnosis is: A. Human immunodeficiency virus infection B. Infectious mononucleosis (Epstein-Barr virus infection) C. Tuberculosis D. Methicillin-resistant Staphylococcus aureus infection E. Acute lymphocytic leukemia Answer E. Explanation: Leukemias and lymphomas are the most common malignant neoplasms among young children. Question 2. The definitive diagnostic procedure for the child described in Question 8 is: A. Urinalysis B. Lymph node biopsy and culture C. Plain x-ray film D. Ultrasound study of the neck E. Complete blood count and differential 14 Answer B. Explanation: A lymph node biopsy and culture is the definitive means of diagnosing lymphoma. Question 3. Metabolic complications of anticancer therapy include: A. Hyperuricemia B. Hyperkalemia C. Hyperphosphatemia D. Hypocalcemia E. All of the above Answer E. Explanation: Anticancer therapy can result in substantial breakdown of tumor cells (tumor lysis syndrome) with release of large quantities of phosphates and potassium into the circulation. Hypocalcemia can result in the setting of inadequate renal function. Question 4. A 12-yr-old girl receives cranial, neck, and spinal irradiation for cancer. All of the following are likely long-term sequelae of the radiotherapy Except: A. Interstitial fibrosis B. Scoliosis C. Impaired cognition and intelligence D. Pituitary dysfunction Answer D. Explanation: Many sequelae of radiation do not become apparent until the child is fully grown. Irradiation can result in infertility, second cancers, scoliosis, pulmonary dysfunction (interstitial fibrosis), leukoencephalopathy, impaired cognition and intelligence, hypothyroidism, isolated growth hormone deficiency, and panhypopituitarism. Cardiomyopathy is classically associated with the anthracyclines (doxorubicin and daunomycin) but can also occur with irradiation. Question 5. All of the following statements concerning childhood lymphocytic and myelogenous leukemias are Except: A. Leukemias as a group are the most common childhood cancer B. Acute lymphocytic leukemia accounts for approximately 75% of cases C. The incidence is higher in white children than in black children D. The clinical features at presentation are similar E. The responses to therapy and prognoses are similar Answer D. Explanation: The clinical features of the childhood leukemias are similar, because all involve severe disruption of bone marrow function. There is marked variability in response to therapy and in the prognosis. Question 6. All of the following statements concerning acute lymphocytic leukemia (ALL) are true Except: A. Most cases (about 85%) are derived from T-cell progenitors B. Staging of ALL is based on bone marrow biopsy and cerebrospinal fluid examination C. Chromosomal abnormalities are identified in most cases of ALL D. Exposure to medical radiation is associated with an increased incidence of ALL E. Childhood ALL was the first form of cancer shown to be curable with chemotherapy and irradiation Answer D. Explanation: About 85% of cases of ALL are derived from progenitors of B cells, about 15% are derived from T cells, and about 1% are derived from mature B cells. Question 7. BCharacteristic presenting symptoms and signs of childhood leukemia include: A. Pallor 15 B. Petechiae C. Lymphadenopathy D. Bone or joint pain E. All of the above Answer E. Explanation: Most children with leukemia present with symptoms of less than 4 weeks' duration. Most children with ALL have pallor, 50% have petechiae or mucous membrane bleeding, 60% have lymphadenopathy, 25% have fever, and about 25% have bone pain and arthralgias caused by leukemic infiltration of the perichondral bone or joint or by leukemic expansion of the marrow cavity. Question 8. Which of the following factors indicates an increased risk of relapse for childhood ALL? A. Age greater than 1 yr B. Age younger than 10 yr C. Presenting white blood cell count under 100,000/mm3 D. Any chromosomal abnormality Answer D. Explanation: Chromosomal abnormalities are found in most cases of ALL; some indicate a favorable prognosis, some unfavorable, and some have no apparent influence. E. Rapid response to therapy Question 9. A 4-yr-old boy has a bone marrow biopsy that shows 4% blasts. No blasts are seen on peripheral blood smear. Findings on physical examination and other laboratory studies are normal. The most likely diagnosis is: A. Acute lymphoblastic leukemia B. Acute myelogenous leukemia C. Chronic myelogenous leukemia D. Preleukemia syndrome E. None of the above. this is a normal bone marrow biopsy Answer E. Explanation: ALL is diagnosed by a bone marrow evaluation that demonstrates more than 25% of the bone marrow cells as a homogeneous population of lymphoblasts. Question 10. All of the following statements about leukemia in children with Down syndrome are true Except: A. Leukemia occurs more frequently among children with Down syndrome B. Acute lymphoblastic leukemia is the most common type of leukemia that occurs in these children C. Acute myeloid leukemia has a better outcome in children with Down syndrome than in children without Down syndrome D. Chemotherapy is easier to administer because of decreased toxicity compared with the general population E. Almost all neonates with Down syndrome and transient myeloproliferative syndrome eventually develop leukemia Answer E. Explanation: About 20-30% of neonates with Down syndrome who develop a transient leukemia or myeloproliferative syndrome will develop typical leukemia within the first few years of life Question 11. 3-year-old child has arrived to the pediatric department with complaints of ossalgia, increased temperature to 39ºС. During inspection – the condition of the child is severe, can't stand because of the severe bone pain, intoxication, lymph nodes are enlarged about 1,5 cm. Liver is on 3 cm, the spleen is on 2 cm under edge of a costal arch. Complete 16 blood count: Er-.3.0 Т / l, Hb-87g/l, СI-0,9, platelets-190 G/l, leukocytes–3,2 G/l, eosiniphils-1 %, band forms-1 %, segmented 9 %, lymphocytes-87 %, мonocytes-2 %, ESR 36 mm/h. What investigation should be done for confirmation of the diagnosis? A Sternal puncture B Ultrasonic investigation C lymph node puncture D lymph node biopsy E Computer tomography Question 12. 9-year-old girl has complaints on prolong subfebrile fever, loosing weight, drowsiness pallor. Buises on the trunk and extremities, generalised lymphe node enlargement, hepatosplenomegaly are evident. Complete blood count - anemia, leucopenia, thrombocytopenia. Marrow punctate - total blasttransformation. What is the preliminary diagnosis? A Acute leucemia B Eritromielosis C Infectious mononucleosis D Fankoni anemia E Blekfana-Dajmond anemia Question 13. 10-year-old child has weakness, increaseing pallor, fever, Hemorrhages into skin and mucous membranes. Bone marrow – depression of all hematopoetic lines. Aplastic anemia, subacute couse was diagnosed What is the leading method of therapy is indicated at this disorder? A Corticosteroids +bone marrow transplantation B Cytostatics + bone marrow transplantation C Antibiotics + haemotransfusions D Corticosteroids + cytostatics E Splenectomy + haemotransfusions Question 14. 9-year-old child is in severe condition: temperature 38-39°С, nasal bleedings, bone pain. Objectively: extreme pallor, hemorrhagic rash, a ulcerous-necrotic stomatitis. All groups of lymph nodes are enlarged, liver of +5 cm, spleen +4 cm. What investigation is the most useful for confirmation of the diagnosis? A Mielogramme B Complete blood count C complex of immunological investigations D Abdominal ultrasonic E Mediastinum X-ray investigation Question 15. 11-year-old child has arrived at hospital with complaints to the weakness, disordered consciousness, fever about 39°С, nasal bleeding. Objectively: pale, hemorrhagic rash, lymphadenopathy, liver of +4 cm, spleen +2 cm. Blood analysis: red cells-2,1x10T/l, Hb 60 g/l, colour index -0,75, white cells-2,0 G/l, s-30 %, band forms-5 %, eosinofils-5 %, lymphocytes-55 %, мonocytes-5 %, ESR - 60 mm/h. What is the most possible diagnosis? A Acute leucemia B Thrombocytopenia C Aplastic anemia D Haemolytic anemia E Hodgkin`s disease 17 Question 16. 7-year-old infant has weakness, decreased appetite, frequent nasal bleedings and pain in legs. For last 3 months pneumonia, bronchitis and acute tonsilitis. have accured Objectively: the skin is pale, small petechial rash at the trunk and extremities, single bruises. All groups of peripheral lymph nodes are palpated. The liver is +5 cm, the spleen is + 4 cm. Haemogram: red cells - 2,3x10*12/l, Нb-69 g/l, white cells - 3,0x10*9/l, platelets – 41x10*9/l, reticulocytes - 0,2 %, eosinophils-1 %, segmented neutrophils - 25 %, lymphocytes.-71 %, monocytes- 3 %, ESR- 65 mm/hour. What is the most probable diagnosis at the patient? A Mieloproliferave disorder B Systemic lupus erythematosus C Acute rheumatic fever D Trombocytopenic purple E Hodgkin`s disease Literature 1. Nelson Textbook of Pediatrics. - 18th ed. / Ed. by R. Kliegman et al.-Philadelphia: Saunders Co, 2007.- 3146 p. 2. Pediatry. Guidance Aid / За ред. О.В. Тяжка; О.П. Вінницька, Т.І. Лутай – К. : Медицина, 2007 . – 158 с. 3. Current Pediatric Diagnosis & Treatment (CPDT). - 18th ed./ Ed. By W.W.Hay et al. - The McGraw-Hill Companies. – 2006. 4. Current pediatric therapy -18th ed. / Ed. by F.D.Burg et al. - Elsevier Inc. – 2007. 5. Nelson Essentials of Pediatrics -5th ed. / Ed. by B.S.Siegel, J.J.Siegel. - Elsevier Inc. – 2007. 6. ABC of Clinical Haematology - 2nd ed. D. Provan. - BMJ Books. – 2003. 7. Hematology. Basic Principles and Practice - 4th ed. / Edited by R.Hoffman et al. Elsevier Inc. – 2005. 8. Practical Algorithms in Pediatric Hematology and Oncology / Edited by R. H. Sills.- S. Karger AG, P.O. - 2003. Performed by ass. Linnik V.A., ass. Tkachenko N.P. Approved “_____”____________20____y. Сhief of the department, professor Protocol №_____ V. A. Kondratyev Reconsidered Approved “_____”____________20____р. Сhief of the department, professor Protocol №_____ V. A. Kondratyev Reconsidered Approved ““_____”____________20____р. Сhief of the department, professor Protocol №_____ V. A. Kondratyev 18