Diabetes and Renal Disease
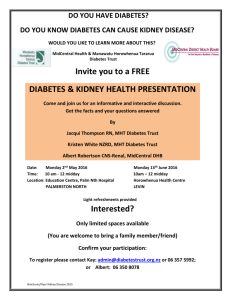
advertisement

Diabetes and Renal Disease Definition Diabetes is a disease that occurs when the body is not able to use sugar, as it should. The body needs sugar for growth and energy for daily activities. It gets sugar when it changes food into glucose (a form of sugar). Glucose is carried through the bloodstream to provide energy to cells. A hormone called insulin is needed for the glucose to be taken up and used by the body. Diabetes occurs when the pancreas is not able to make enough insulin or the insulin that is available is not effective. Statistics Prevalence of diabetes: Age 20 years or older: 16.9 million. 8.6 % of all people in this age group have diabetes. Age 65 years or older: 7 million. 20.1% of all people in this age group have diabetes. Men: 7.8 million. 8.3% of all men have diabetes. Women: 9.1 million. 8.9% of all women have diabetes. Approximately 17 million people in the U.S., or 6.2 % of the population, have diabetes. While an estimated 11.1 million have been diagnosed, unfortunately, 5.9 million people (or 1/3) are unaware that they have the disease. Deaths among people with diabetes: In 1999, approximately 450,000 deaths occurred among people with diabetes aged 25 years and older. This figure represents about 19% of all deaths in the United States in people aged 25 years and older. Overall, the risk for death among people with diabetes is about 2 times that of people without diabetes. Diabetes was the sixth leading cause of death listed on U.S. death certificates in 1999. Causes The cause of diabetes is unknown, although both genetics and environmental factors such as obesity and lack of exercise appear to play roles. Symptoms Some symptoms may include: Sudden vision changes Excessive thirst Extreme hunger Frequent urination Nausea, vomiting, or stomach pains Unexplained weight loss Tingling or numbness in hands or feet Fatigue Very dry skin Sores that are slow to heal More infections than usual Types of Diabetes Noninsulin-Dependent or Type 2 Most common type of diabetes This type usually develops gradually, most often in people over age 40 Type 2 diabetes occurs when the body does not make enough insulin or the body makes insulin but cannot properly use it Insulin-Dependent or Type 1 Appears suddenly and most commonly in younger people under age 30 (sometimes referred to as juvenile diabetes) Type 1 diabetes occurs when the body destroys the cells in the pancreas that produce insulin, usually leading to a total failure to produce insulin Gestational Diabetes Mellitus (GDM) Occurs in some women during pregnancy This condition may occur in the second half of pregnancy where the woman may have high blood glucose levels As the pregnancy ends, the blood glucose levels will return to normal Related Terms Hypoglycemia Condition that occurs when blood glucose levels are too low. Symptoms may include: cranky, tired, sweaty, hungry, confused, and shaky and is some instances can lose consciousness or experience a seizure Eating sugar may treat hypoglycemia Hyperglycemia Occurs when blood sugar is too high Symptoms may include: extreme thirst, frequent urination, fatigue, blurred vision, vomiting and weight loss Diabetic Nephropathy Kidney disease occurs when there is damage to the kidney Treatments The key is keeping a balance of the following: Taking insulin as prescribed by a physician Having a healthy diet Regular exercise Losing weight Testing blood sugar levels regularly No smoking Insulin There are different types of insulin based on how soon the insulin starts working (onset), when it works the hardest (peak time), and how long it lasts in your body (duration) Many people who take insulin use a syringe, but other methods of delivery include a pen and an insulin pump A common side effect from insulin is a hypoglycemic attack resulting from low blood glucose levels Oral Medications There are five different classes of diabetes medications that work in the body to improve blood glucose levels: Sulfonylureas This class of drugs works by stimulating the pancreas to release more insulin and is often one of the first oral therapies given to people with type 2 diabetes. Common side effects include weight gain, mild gastrointestinal disturbances, alcohol intolerance, mild skin irritations and hypoglycemia or low blood glucose levels. Biguanides (Metformin) This drug is often prescribed in combination therapy with other diabetes medications or insulin, and can be used as a first line of treatment. This class works by keeping the liver from releasing too much glucose and helping the body better respond to its own insulin. Metformin, on its own, can minimize the risk of hypoglycemic attacks. Common side effects may include nausea, diarrhea or mild gastrointestinal disturbances and loss of appetite. Alpha-Glucosidase Inhibitors This class of drugs helps delay the digestion of sugars and carbohydrates by releasing them slowly into the system, avoiding high blood glucose levels after meals. Common side effects include nausea, diarrhea, mild gastrointestinal disturbances, bloating and gas. Thiazolidinediones (TZD) This class helps sensitize the muscle cells to insulin and reduce the amount of glucose released by the liver, resulting in increased glucose uptake. Side effects may include nausea, vomiting, abdominal pain, fatigue, loss of appetite and dark urine. Meglitinides This class of drug also stimulates the pancreas to release more insulin. As with many diabetic drugs, however, hypoglycemia is a potential side effect. Accommodations Hypo/Hyperglycemia: Allow for storage of medications such as insulin, and/or food Supply an area to test blood sugar levels Supply an area to administer medications (insulin) Provide appropriate containers for needles/syringe disposal Provide a rest area for reorientation after hypo/hyperglycemic episode Frequent breaks for food as needed Fatigue or Weakness: Frequent rest breaks Reduce or eliminate strenuous activities Anti-fatigue mats or padded carpeting Provide rest area with cot Flexibility to sit or stand Job sharing Shorten work day and extend work week Vision Impairment: (e.g.-sudden vision changes) If benefit from magnification, consider options to enlarge with magnification devices or computer screen magnification software If does not benefit from magnification, consider options for accessing information through Braille, tactile graphics, or voice output technology Provide a tape recorder Provide a reader Flexible schedule to use public transportation to and from work Use of service animal for assistance with mobility Nephropathy: (e.g.-Kidney Disease) Provide easy access to restroom facilities Allow a flexible schedule or time off for treatment (dialysis) Neuropathy: (e.g.-Nerve damage) Modify job tasks requiring fine finger dexterity Provide protective clothing and equipment Eliminate or reduce the need to use sharp objects Cognitive Complications: Provide written job instructions and prioritize assignments Use of day planner or electronic organizer Provide flexible work hours Minimize distractions Recommended Readings Job Accommodations Network (JAN) The Job Accommodation Network (JAN) is a free consulting service that provides information about job accommodations, the Americans with Disabilities Act (ADA), and the employability of people with disabilities. http://www.jan.wvu.edu/links/ American Diabetes Association The American Diabetes Association is the nation's leading nonprofit health organization providing diabetes research, information and advocacy. The mission of the organization is to prevent and cure diabetes and to improve the lives of all people affected by diabetes. To fulfill this mission, the American Diabetes Association funds research, publishes scientific findings, provides information and other services to people with diabetes, their families, health care professionals and the public. The Association is also actively involved in advocating for scientific research and for the rights of people with diabetes. http://www.diabetes.org/ Research Article Martz, E., Roessler, R., & Livneh, H. (2002). Responses to insulin reactions and long-term adaptation to diabetes. Journal of Rehabilitation, 68 (2), 14-21. Renal Disease Function of the kidney: The kidney has three basic functions: Filter: The kidney acts as a filter to remove waste products and fluids. Blood pressure control: The kidney acts with a substance, renin, to control blood pressure from becoming high. If the kidneys are not removing enough fluid, urine, blood pressure can rise. The heart works harder pumping blood to the body when there is extra fluid to be pump blood through. Hormone production: The kidney produces a hormone, erythropoietin. This hormone is responsible for red blood cell production in your bone marrow. The kidney also produces the active form of Vitamin D so a person is able to absorb calcium. Statistics: In the United States, 15%-20% of kidney failure cases are due to hypertension. Hypertension is second only to diabetes as the leading cause of kidney failure. It is estimated that hypertension affects 20% of the adult population in most countries. Types of Renal Failure: Acute Renal Failure: Kidneys could be damaged suddenly. This could be due to injury, disease or toxins. When remedies for these are sought, kidney functions could be restored. Chronic Renal Failure: If you have chronic renal disease, you are slowly losing kidney functions. Over a period of time this could lead to kidney failure and serious health complications. You may not even be aware of this in the beginning. It is not possible to restore the functions you have already lost. But it is possible to control or retard the process of deterioration. End Stage Renal Disease (ESRD): Chronic Renal failure progresses to a point when kidneys work less than 10% capacity. At this point, the kidneys are no longer fulfilling their role of removing waste and excess fluids from the body. So, toxins begin to build up in the blood causing a person to become ill. There is currently no cure for End-Stage Renal Disease. This condition is fatal unless dialysis on a regular basis or kidney transplant is performed, to restore kidney functions. Causes: Diabetes Diabetes is the most common cause of kidney disease. Diabetes is a metabolic disorder caused by the insufficient insulin secretion or inefficient usage of the insulin secreted by the body. Hypertension Hypertension or high blood pressure is defined as a blood pressure reading of greater than 140/90* in adults over 18 years of age. *Measured in mm Hg (millimeters of mercury) Other Causes include: Chronic Glomerulonephritis Polycystic Kidney Disease Kidney infections Lupus Kidney Stones Some congenital defects like pylonephritis Symptoms: Early stages of kidney disease are asymptomatic. As the disease progresses the following symptoms are experienced: Burning or difficulty during urination More frequent urination, especially during the night Blood in the urine Puffiness around the eyes or swelling of hands and feet Pain in the back or side, below the ribs Diagnosis: Blood Tests Creatinine Any form of activity leads to the breakdown of muscle. This is then replaced by body building foods. When the muscle breaks down, a waste product called creatinine is produced. This is moved from the blood to the urine by the kidneys. When kidneys are not working well, creatinine builds up in the blood. The normal (serum) creatinine range is 0.6 to 1.2 mg/dl. However, some labs may define the normal range a little differently. Besides, your diet may also have an impact on the creatinine level. However, if your creatinine level is consistently beyond the normal range, there is reason to believe that your kidneys have a problem. Blood Urea Nitrogen (BUN) Urea is a waste product in the blood. This is produced when the cells take protein from the blood. Urea contains nitrogen. It is the work of the kidneys to expel urea from the blood into the urine. If your kidney functions are affected, more urea than is normal is found in the blood. Normal blood contains 7 to 20 milligrams of urea per deciliter of blood. If your BUN is more than 20 mg/dl, your kidneys may not be working at full strength. An increase in BUN could also suggest other health problems. Urine Tests Creatinine Clearance Another way to measure kidney function is the Creatinine Clearance test. This test shows how fast your kidneys remove creatinine from the blood. Clearance is measured in milliliters per minute (ml/min). Creatinine Clearance is arrived at by comparing the amount of creatinine in your urine to the amount of creatinine in your blood. Proteinuria Normally, kidneys filter out wastes from blood. They also reabsorb any nutrients that may have gone out with the wastes. When the kidneys are affected proteins, so valuable to the body, begin to slip out with the wastes. This leads to a condition called proteinuria. Ultra sonogram When there is enough evidence in your blood and urine tests to suggest a problem, the first test you will be asked to take an ultra sonogram of the abdominal area. These help to detect if there are growths or obstructions in your kidney. Computer Aided Tomography (CAT) scan Magnetic resonance Imaging (MRI). Biopsy A renal biopsy involves snipping off of a tiny bit of kidney tissue for study under a microscope. This study helps to know if there is any problem at the cellular level in the kidneys. http://www.webhealthcentre.com/general/rd_diag.asp - TOP#TOP Treatment: Dialysis-The process of removing waste matter and maintaining electrolyte balance through diffusion is called dialysis. Usually performed by the kidneys, this is performed by artificial means in kidney patients. The two main types of dialysis are: Peritoneal Dialysis Peritoneal dialysis occurs inside the body. It uses your peritoneal membrane (the lining of you abdomen) as the filter. For this treatment, a tube called a catheter is surgically placed through the wall of your abdomen. o Continuous Ambulatory Peritoneal Dialysis (CAPD) Allows gravity to draw dialysis solution into and out of the peritoneal cavity, using a system of tubing and bags. Usually, CAPD is performed four times a day. Each solution exchanges lasts about half an hour. Assist devices help people with problems seeing or with problems using their hands to do CAPD. o Automated Peritoneal Dialysis (APD) The second type of peritoneal dialysis, automated peritoneal dialysis (APD) involves a machine. You attach the tubing and solution bags to the machine. Before going to sleep, you connect the tubing to the peritoneal catheter. During the night the machine performs the dialysis. Haemodialysis Blood is pumped outside the body to an artificial kidney machine. The machine cleanses the blood and returns it to the body. Only a small amount of blood is out of the body at any time. The average person receives three treatments per week. Each treatment lasts three to four hours. There are two options for haemodialysis: (1) home haemodialysis, and (2) in-centre or clinic haemodialysis. http://www.webhealthcentre.com/general/rd_treat.asp TOP#TOPTransplantation During a transplant, a healthy donated kidney is placed deep under your skin near your hip bone. In some cases, the non working kidneys may be removed to control infection or high blood pressure. Research Article: Symister, Petra; Friend, Ronald. (1996). Quality of life and adjustment in renal disease: A health psychology perspective. [References]. [Chapter] Resnick, Robert J (Ed); Rozensky, Ronald H (Ed). Health psychology through the life span: Practice and research opportunities. (pp. 265-287). Washington, DC, US: American Psychological Association. xvii, 464 pp. **Please refer to the Diabetes Module for more information.