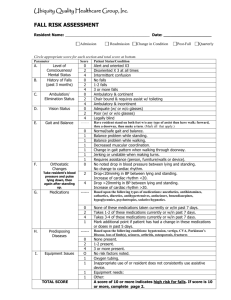
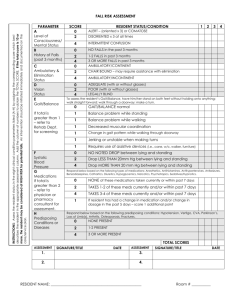
RESIDENT ASSESSMENT
advertisement
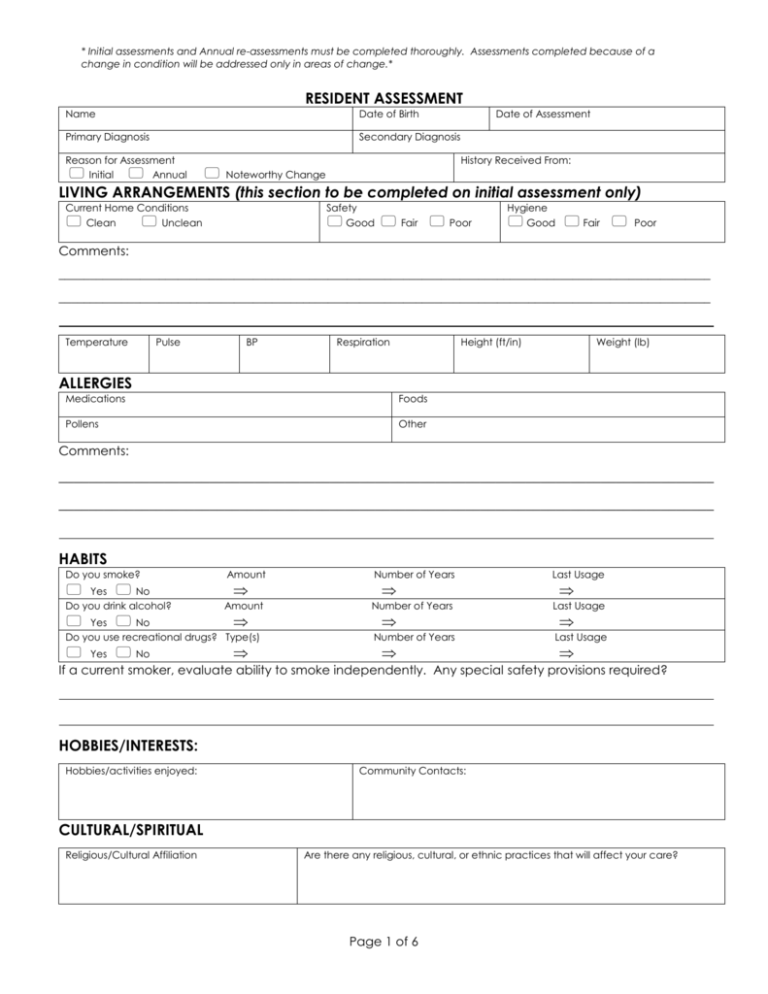
* Initial assessments and Annual re-assessments must be completed thoroughly. Assessments completed because of a change in condition will be addressed only in areas of change.* RESIDENT ASSESSMENT Name Date of Birth Primary Diagnosis Secondary Diagnosis Reason for Assessment Initial Annual Date of Assessment History Received From: Noteworthy Change LIVING ARRANGEMENTS (this section to be completed on initial assessment only) Current Home Conditions Clean Unclean Safety Good Fair Poor Hygiene Good Fair Poor Comments: ________________________________________________________________________________________________________ ________________________________________________________________________________________________________ Temperature Pulse BP Respiration Height (ft/in) Weight (lb) ALLERGIES Medications Foods Pollens Other Comments: _______________________________________________________________________________________ _______________________________________________________________________________________ HABITS Do you smoke? Yes No Do you drink alcohol? Amount Amount Yes No Do you use recreational drugs? Type(s) Yes No Number of Years Number of Years Number of Years Last Usage Last Usage Last Usage If a current smoker, evaluate ability to smoke independently. Any special safety provisions required? HOBBIES/INTERESTS: Hobbies/activities enjoyed: Community Contacts: CULTURAL/SPIRITUAL Religious/Cultural Affiliation Are there any religious, cultural, or ethnic practices that will affect your care? Page 1 of 6 Resident Assessment MEDICAL HISTORY: SURGICAL HISTORY SURGERY DATE SURGERY 1. 6. 2. 7. 3. 8. 4. 9. 5. 10. DATE MEDICATIONS Who is responsible to purchase medications? Who is responsible to store medications? Who is responsible to administer medications? Primary Pharmacy: MEDICATION Phone Number: DOSAGE ROUTE FREQUENCY DATE OF RX PHYSICIAN Any over-the-counter medications commonly used, and reasons for use: Have there been any recent changes in medications? . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . If yes, explain: COMFORT Pain/Discomfort Intensity (1-10) Location Yes No How do others recognize that you are in pain? What relieves your pain? SLEEPING PATTERNS: Page 2 of 6 Yes No Resident Assessment COMMUNICATION Speech Education Level Primary Language Hearing Vision Modes of expression: Able to make self understood? Yes No Explain: Able to understand others? Yes No Explain: Comments: ABILITIES: Activities of Daily Living ACTIVITY Independent Needs Assistance Dependent RECOMMENDATIONS Eating Ambulation Transfer Grooming Oral Hygiene Toileting Dressing Bathing Food Preparation Medications Manage Finances Healthcare Visits DAILY ROUTINES: typical 6 AM 6 PM 7 AM 7 PM 8 AM 8 PM 9 AM 9 PM 10 AM 10 PM 11 AM 11 PM 12PM 12 AM 1 PM 1 AM 2 PM 2 AM 3 PM 3 AM 4 PM 4 AM 5 PM 5 AM ORTHOPEDIC Equipment Used/Comments: Page 3 of 6 COMMENTS Resident Assessment NEUROLOGICAL Mental Status Oriented Alert Confused/Disoriented To: Motor Movement Right Arm: Paralysis Cooperative Agitated Anxious Confused Level of Consciousness: Left Arm: Right Leg: Syncope Yes No Location Yes No Restless Left Leg: Vertigo Yes Tremors Yes No Seizures Type Duration Last Seizure Yes No No Comments: RESPIRATORY Airway Breathing Oxygen Therapy Type Yes No Sounds Right: Liters per Minute: Left: Assistance Required: Yes No Comments: CARDIOVASCULAR Dizziness Yes Shortness of Breath Yes No No Edema Yes Cyanosis Yes No No Comments: GASTROINTESTINAL Diet Appetite Mouth Problems # Meals/day # Snacks/day Dietary Supplements Recent Wt loss/gain If yes, explain: Yes No Swallowing Difficulties: If yes, explain: Yes No Dentures Upper Lower Teeth Problems None Bowel Schedule/Patterns Yes If yes, explain: No Bowel Management Program Check all that apply: Incontinent Laxative use Yes Constipation Diarrhea No Use of Incontinence Products? Comments/preferences: Page 4 of 6 Yes No Specify: Specify Resident Assessment GENITOURINARY Bladder Dribbling Incontinent Stoma Stones Frequency Difficulty Burning Retention Nocturia Distention UTI Hematuria Starting Stream Onset of Symptoms Catheter Type Yes Dialysis Yes Size No No Last Changed Frequency Location of Dialysis Service/Phone contact Comments: SKIN Color Temperature PROBLEMS Turgor LOCATION(S) PROBLEMS Edema Dry Skin Flaky Skin Rash Lesion Scars Burns Ecchymosis Abrasion Laceration Pressure Ulcer Wound Dressings Stoma Colostomy Bag LOCATION(S) Wounds/ Location Decubitus Length Width Depth Frequency Dressing: List any previous or potential skin conditions: Comments: SAFETY ISSUES Does the participant have the ability (physical, cognitive, etc) to leave the boarding home without supervision? . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . Yes No Yes No Yes No Explain: Can participant access emergency response without assistance? . . . . . . . . . . . . . . . . . . . Explain: Can participant access emergency exits independently? . . . . . . . . . . . . . . . . . . . . . . . . . . Explain: Page 5 of 6 Resident Assessment List any additional safety needs: DECISION-MAKING CAPABILITIES Can make own decisions: Yes Alternate Decision Maker/Contact #: Advance Directives in place, if any: No Scope of decision-making abilities: ADDITIONAL ASSESSMENT TOOLS USED (please see attached forms, as necessary) Mental Health Yes Dementia No Yes Other Yes No No NURSING NEEDS/DELEGATION ISSUES: RECOMMENDATIONS: COMMENTS: ___________________________________ Signature of prospective resident/resident ___________________________________ Signature of Person Completing Assessment ___________________________________ Signature of Registered Nurse, if applicable (Only if different from person completing Assessment) ________________________________________ Signature of responsible party/family ________________ Credentials ________________ Date Page 6 of 6 _____________________ Date