Chapter 18 - Moorpark College
advertisement

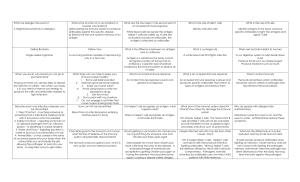
Chapter 18 - Defense Mechanisms of the Body - pages 695-738 SECTION A - IMMUNOLOGY: DEFENSES AGAINST FOREIGN MATTER I. Chapter 18 - Introduction A. Basic concept is "self, not-self" 1. Immunity - any mechanism that maintains the "self, not-self" distinction (very broad definition) 2. Not-self a) b) c) Bacteria, virus, funguses, protozoa, parasites read brief description page 696 Non-microbial foreign substances Destroy cancerous cells in body immune surveillance B. II. Categories 1. Nonspecific immune defenses - does not require prior exposure and is nonselective in protection; it is inherited 2. Specific immune defenses - depends on prior exposure to a specific foreign material, recognition of it upon subsequent exposure and reaction to it; it is ACQUIRED and not inherited (one exception explained later) Cells mediating immune responses A. Introduction, overview 1. Leukocytes - white blood cells (WBC) a) Neutrophils b) Eosinophils c) Basophils d) Monocytes e) Lymphocytes (1) B cells (2) T cells (a) Cytotoxic T cells (b) Helper T cells (3) NK cells 2. Plasma cells a) Derived from peripheral lymphoid tissues and B lymphocytes b) Secrete antibodies 3. Macrophages a) Ubiquitous tissue phagocytes b) Differentiated from monocytes 4. Macrophage-lke cells a) Cells that are produced in most tissues b) Are called microglia in the CNS 5. Mast cells a) Produced in almost all tissues and organs b) Differentiate from bone marrow cells Page 1 of 22 Chapter 18 - Defense Mechanisms of the Body - pages 695-738 B. Table 18-1, page 697 - major functions of cells mediating immune responses Cells Neutrophils Basophils Eosinophils Monocytes B cells Cytotoxic T cells Helper T cells NK cells Plasma cells Macrophages and macrophage-like cells Mast cells III. Functions 1. Phagocytosis 2. Release chemicals involved in inflammation (vasodilators, chemotaxins, etc.) Have functions in blood similar to those of mast cells in tissues (see below) 1. Destroy multicellular parasites 2. Participate in immediate hypersensitivity reactions 1. Have functions in blood similar to those of macrophages in tissues (see below) 2. Enter tissues and are transformed into macrophages 1. Initiate antibody-mediated immune responses by binding specific antigens to their plasma membrane receptors, which are immunoglobulins 2. During activation are transformed into plasma cells, which secrete antibodies 3. Present antigen to helper T cells Bind to antigens on plasma membrane of target cells (virus-infected cells, cancer cells, and tissue transplants) and directly destroy the cells Secrete cytokines that help to activate B cells, cytotoxic T cells, NK cells, and macrophages 1. Bind directly and nonspecifically to virus-infected cells and cancer cells and kill them 2. Function as killer cells in antibody-dependent cellular cytotoxicity (ADCC) Secrete antibodies 1. Phagocytosis and intracellular killing 2. Extracellular killing via secretion of toxic chemicals 3. Process and present antigens to helper T cells 4. Secrete cytokines involved in inflammation, activation and differentiation of helper T cells, and systemic responses to infection or injury (the acute phase response) Release histamine and other chemicals involved in inflammation Cytokines A. General term for a large number (over 100) of protein messengers B. Regulate host cell growth C. Function in both specific and nonspecific immune mechanisms D. Complex physiology and a lot not known about function 1. Secreted by more than one type of cell a) Immune system cells b) Non-immune system cells (endothelial cells & fibroblasts for instance) 2. Often operate with cascade effect Page 2 of 22 Chapter 18 - Defense Mechanisms of the Body - pages 695-738 3. 4. 5. Broad range of actions Redundancy in function Involved in non-immune process such as bone formation and uterine function IV. Non-specific immune responses A. Introduction - responses that do not have to recognize specific identity of "invader" B. C. D. E. General “markers” particular classes of carbohydrates or lipids that are part of most microbial cell walls Specific immunity depends primarily on protein markers (later) Defenses at Body Surfaces 1. Skin is physical barrier but includes microflora of protective bacteria 2. Sweat glands, sebaceous and lacrimal glands secrete antimicrobial chemicals 3. Mucus secreted by epithelium of respiratory and G.I. tracts is antimicrobial and sticky helping cilia to sweep away foreign material and microbes 4. Macrophages engulf microbes, etc. 5. Hair in nose, sneezes, coughs 6. Harmless microbes on the skin and other surface linings can suppress the growth of other potentially harmful microbes -How? Inflammation 1. Summary Table 18-2, 699 (details below) a) Initial entry of bacteria (not-self) into tissue b) Vasodilation of the microcirculation in the infected area, leading to increased blood flow c) Marked increase in protein permeability of the venules in the infected area, with resulting diffusion of protein and filtration of fluid into the interstitial fluid d) Chemotaxis: exit of leukocytes from the venules into the interstitial fluid of the infected area e) Destruction of bacteria in the tissue either through phagocytosis or by mechanisms not requiring prior phagocytosis f) Tissue repair 2. Vasodilation and increased permeability to protein a) Histamine secreted by mast cells b) Promote vasodilation and fluid collection c) Local capillaries become more permeable to protein (1) Kinins are derived from kininogens (2) Promote exudation & vasodilation and can hurt like hell d) Fluid collects in area and swelling occurs e) Exudation of neutrophils and monocytes Page 3 of 22 Chapter 18 - Defense Mechanisms of the Body - pages 695-738 f) 3. 4. Destruction of bacteria by phagocytosis or other means Chemotaxis a) The neutrophils stick to adhesion molecules on the endothelium and start increased amoeboid movement b) Neutrophil "squeezes" between endothelial cells neutrophil exudation via "stronger" adhesion molecules c) Entire response is called chemotaxis and is induced by chemotaxins which cause Ca2+ entry into neutrophils which promotes movement d) Monocytes "show up" later and participate in carnage on foreign agent e) Cytokines that are chemoattractants are called chemokines Phagocytosis, Figure 18-1, 701 and Figure 18-2, page 701 a) Opsonin - a substance that "marks" a foreign substance for phagocytosis (actually binds it and holds for phagocyte) Endocytosis phagosome phagolysosome degranulation exocytosis (1) Phagolysosome produces H2O2 (hydrogen peroxide) which destroys foreign agent (2) Nitric oxide destroys the microbe (3) Phagocyte doesn't necessarily die but can repeat process c) Neutrophils and macrophages also secrete substances that fight invader (1) Help regulate inflammatory response (2) Extracellular killing of microbes (3) Activation of clotting and anticlotting pathways (4) Hormonal regulation of systemic response to infection Complement, Figure 18-3, 702 and Figure 18-4, page 703 a) Group of at least 20 different proteins that normally circulate in blood b) Another mechanism for extracellular microbe killing c) When first protein in chain is activated that triggers a "cascade" effect which results in the final complement protein "attacking" the plasma membrane of the foreign agent (1) The last protein is actually the five different proteins called the membrane attack complex or MAC b) 5. Page 4 of 22 Chapter 18 - Defense Mechanisms of the Body - pages 695-738 (2) The MAC penetrates the membrane and opens channels through which the microbes "guts" leak out (3) This is the major, nonphagocytic, method of protection in nonspecific immunity (4) As the different products of the complement pathway are formed they may also mediate other actions, see Figure 18-3, page 703 (5) C - release of histamine from mast cells 3a (6) C - an opsonin and participates in MAC 3b complex d) Classical complement pathway versus alternate complement pathway (1) Classical pathway - Antibodies from lymphocytes activate C1 (2) Antibodies are a result of specific immunity - how then is nonspecific complement system activated? (3) Alternate pathway plugs in at C3b (by passes C1)and does not involve antibodies but the microbes must have certain carbohydrates on their surface (4) Not all microbes stimulate complement attack 6. Local inflammatory mediators, Table 18-3, page 700 Mediator Source Kinins Plasma proteins Complement Plasma proteins Products of blood clotting Plasma proteins Histamine Mast cells Eicosanoids; Many cell types Platelet-activating factor Many cell types Cytokines, including chemokines Monocytes, macrophages, Examples are interleukin 1, tumor neutrophils, lymphocytes, and necrosis factor (TNF), and several nonimmune cell types, interleukin 6 including endothelial cells and fibroblasts Lysosomal enzymes, nitric oxide, Neutrophils and macrophages and other oxygen-derived substances 7. Tissue repair a) Fibroblast divide and form scar b) Abscess - bag of pus walled off by fibroblasts and collagen c) Granuloma - like tuberculosis and may be contained for years within it 8. Interferon, Figure 18-6, page 704 a) Different sites of production and ranges of biological activity Page 5 of 22 Chapter 18 - Defense Mechanisms of the Body - pages 695-738 b) V. A family of proteins that fight viral infections in particular c) Inhibits viral replication in host cells by the following mechanism (1) Virus enters a cell that can make interferon (2) Interferon leaves that cell and binds to surface membranes of neighboring cells (3) That binding induces synthesis of antiviral enzymes in that cell that block the synthesis of proteins that the viruses need for replication (4) The antiviral proteins are not activated until the virus actually enters the cell (viral RNA activates) d) Interferon stimulates lymphocytes into action to attack and kill virus-infected cells and cancer cells (possible treatment!) Specific Immune Responses A. Lymphocytes mediate specific immune responses, See Table 18-1, page 697 B. Overview of typical immune response 1. 2. Antigen defined as any foreign molecule that can trigger a specific immune response against itself or the cell bearing it a) Specific foreign matter (1) Any foreign matter that can trigger a specific immune response and it can appear from within or from without (2) It is a functional term (3) Normally protein or complex carbohydrate (4) Can part of a smaller molecule or part of a large object such as pollen b) Antigen processing must occur in the body before lymphocytes can interact with it (1) Macrophages play this role - the general term is antigen-presenting cell (APC) (2) The foreign substance or thing is phagocytized and unfolded or otherwise "dismembered" - the unfolding, etc., exposes internal amino acids for recognition (3) The macrophages "shuttle" the processed molecules to the cell surface where they may be accessible by lymphocytes Three stage process - 1) antigen encounter and recognition, 2) lymphocyte activation, 3) the attack a) Antigen Encounter And Recognition: During its development each lymphocyte synthesizes and inserts into its plasma membrane receptors that are able to bind to a specific antigen. Page 6 of 22 Chapter 18 - Defense Mechanisms of the Body - pages 695-738 (1) b) c) If the lymphocyte encounters that antigen later, the antigen binds to the receptor. This binding is termed "recognition" in immunology. (2) Lymphocytes are able to distinguish one antigen from another by the nature of their plasma-membrane receptors. (3) Each lymphocyte is specific for just one type of antigen (a) Estimated that the lymphocyte population expresses more than 100 million distinct antigen receptors. (b) A single type of antigen receptor may be expressed by a small number of lymphocytes, termed a clone. (c) That is, there are more than 100 million distinct small clones of lymphocytes in the body. (d) Called the Clonal Selection Theory Of Immunity Lymphocyte Activation: The binding of antigen to receptor is the trigger for lymphocyte activation. (1) The lymphocyte undergoes multiple mitotic divisions (2) Only one still has the antigen combined with it. (3) Many lymphocytes are formed that are identical to the one that started the cycles and can recognize the antigen; this is termed clonal expansion (4) Lymphocyte Activation: lymphocytes undergo a differentiation process, depending upon the lymphocyte type. (5) After activation, types-B cells and cytotoxic T cells-then function as "effector lymphocytes," which are actors in the attack phase. (6) Helper T cells, after activation, secrete cytokines that enhance the function of B cells and cytotoxic T cells. The Attack: The activated effector lymphocytes launch an attack against all antigens of the kind that initiated the immune response. (1) It takes only one or two antigen molecules to initiate the specific immune response - an attack on all of the other antigens of that specific kind in the body. (2) B cells differentiate into cells termed plasma cells, which secrete antibodies into the Page 7 of 22 Chapter 18 - Defense Mechanisms of the Body - pages 695-738 C. blood, and these antibodies then recruit and guide other molecules and cells to perform the actual attack. (3) Cytotoxic T cells directly attack and kill the cells bearing the antigens. Lymphoid organs and lymphocyte origins 1. Lymphocytes circulate in the blood but most are in lymphoid organs a) Primary lymphoid organs (1) Bone marrow and thymus (2) Supply peripheral lymphoid organs with mature lymphocytes ready to do the job b) Secondary lymphoid organs (a.k.a. peripheral lymphoid organs) (1) Lymph nodes, spleen, tonsils, and lymphocytes found in the intestinal, respiratory, genital and urinary tracts (2) Lymphocytes in the secondary organs can undergo mitosis and form clones (3) It is in these locations that lymphocytes do their thing 2. Lymphoid organs versus lymphatic system a) Lymphatic system is a conducting system b) Only the lymph nodes are part of the lymphoid "organs" 3. Thymus a) Lies in upper chest and is large in infant and gradually gets smaller b) Secretes thymosin (thymopoietin) which is a group of hormones that is largely not understood 4. Lymph nodes, Figure 18-7, page 705 a) Lined with macrophages b) Have large clusters of lymphocytes 5. Spleen a) Largest lymphoid organ (lies in abdomen) b) Blood percolates through (1) Large collection of lymphocytes and macrophages (2) Also phagocytize aging and dead erythrocytes c) In adult only lymphocytes are formed in spleen, in fetus all types of blood cells are formed there 6. Tonsils a) In pharynx b) Filled with lymphocytes and macrophages 7. Recirculation of lymphocytes goes on constantly all over the body Page 8 of 22 Chapter 18 - Defense Mechanisms of the Body - pages 695-738 D. Lymphocyte origins B and T cells 1. B cells mature in blood marrow and are carried to lymphoid organs (first called B cells because they pass through the bursa of the chicken and that is where they were first discovered) 2. T cells leave bone marrow in an immature state during fetal and neonatal life and are carried to the thymus a) That is why they are called T cells Subsets of T cells cytotoxic, helper and suppressor 3. Natural killer cells (NK cells) a) Arise in bone marrow but exact origin is unclear b) Are not dependent on specific antigens (more later) Functions of B cells and T cells 1. Figure 18-8, page 707 – derivation of B and T cells 2. B-cells, "humoral", antibody mediated a) B cells differentiate into plasma cells following activation b) Antibodies are proteins in group called immunoglobulins (more detail later) (1) Figure 18-9, page 708 (2) Present in plasma membranes of B cells (3) Are produced by plasma cells after activation (4) The secreted antibodies travel via the blood stream all over the body (5) Defend against bacteria, viruses, other microbes in extracellular fluid and against toxins 3. T-Cells (cytotoxic and helper) and natural killer cells - known as cell mediated immunity a) Will not discuss hypothesized suppressor T b) Cytotoxic T cells travel everywhere but attack cells with antigens that initiated the original immune response b) E. 4. 5. (1) Cytotoxic T cells CD8 proteins in plasma membrane, a.k.a. CD8+ cells (2) Helper T cells CD 4 proteins in plasma membrane, a.k.a. CD4+ cells Helper T cells CD4+ cells a) Undergo activation but do not attack antigen b) Secrete messenger substances that facilitate the activation and function of B cells and cytotoxic T cells Generalizations a) Antibody mediated responses are more varied than cell mediated Page 9 of 22 Chapter 18 - Defense Mechanisms of the Body - pages 695-738 b) F. Cell mediated attacks are limited, in particular, cancerous or cells infected with viruses 6. Figure 18-9, page 708 – summary of roles of B and T cells Lymphocyte receptors 1. B-cell receptors a) Has copies of "its" antibodies on cell surface and acts as the receptor - technically it's not an antibody but a glycoprotein b) There are millions of different kinds B cells (1) There are more kinds of B cells than there are genes (200) to make them (2) Clonal selection (3) Different kind of DNA and enzymes to create such a large variety of B cells c) Structure, Figure 18-10, page 709 (1) Four interlinked polypeptides (2) Two heavy or long chains and two short or light chains (3) Five classes of immunoglobulins, A, D, E, G and M (4) Fv for variable and contains the antigenbinding site - there are many kinds of these - millions! (5) B cell receptors can bind either freely circulating antigens or antigens on surface of a foreign cell -- the B cell can be attached to the foreign cell via the connection 2. T-cell receptors a) T cells do not produce immunoglobulins b) Have two-chained proteins that differ in one region from T cell to T cell c) T cells mature in the thymus d) The antigen in question must form a complex with certain of the body's own plasma-membrane proteins in order to combine with the T cell receptor (1) Major histocompatibility complex (MHC) MHC proteins - two classes, I and II (2) Except for identical twins, no two people have the same MHC proteins (3) With the exception of erythrocytes, Class I MHC proteins are found on the surface of all the cells in the body (4) Class II proteins are found primarily on the surfaces of macrophages and a few other cell types including B cells (5) Restriction elements is a termed used to describe MHC proteins since the different T Page 10 of 22 Chapter 18 - Defense Mechanisms of the Body - pages 695-738 G. cells have different requirements for recognition, Table 18-4, page 710 Cell type MHC restriction B None (do not interact with MHC proteins) Helper T Class II, found only on macrophages, macrophagelike cells and B cells Cytotoxic T Class I, found on all nucleated cells of the body NK No MHC interaction for activation 3. NK-cell receptors a) These cells may have no MHC restriction b) Less specific than cytotoxic T cells c) NK cell receptors are not understood Antigen presentation to T cells - APC (antigen-presenting cells) 1. T cells can bind antigen only when the antigen appears on the plasma membrane of a host cell that is complexed with the cell’s MHC proteins. 2. Presentation to helper T cells a) Helper T cells require class II MHC b) Class II MHC is found only on macrophages, B cells and macrophage-like cells c) Only the cells above can act as APCs for helper T cells d) Antigen processing and recognition, Figure 18-11a, page 711 e) An antigenic determinant is known as an epitope f) Macrophage may process and present antigen at the site of entry g) Macrophage may enter lymphatic vessel and travel to lymph node h) Bacteria may enter lymph vessels or blood untouched and be processed in lymph nodes or by spleen in the blood 3. B-cell activation: The role of helper T cells - Figure 18-11b, 711 a) B cells can not, on their own, inactivate an antigen, helper T cells must secrete lymphokines b) B cell binds antigen, T cell binds Class II MHC on surface of macrophage (or other antigen presenting cell) - the macrophage is being bound by B cells and helper T cells c) T cell "costimulus" activation, Figure 18-12,page 711 (1) Non-receptor plasma membrane proteins (non-antigenic matching proteins) (2) APC secretes interleukin 1 (IL-1) and TNF in response to binding Page 11 of 22 Chapter 18 - Defense Mechanisms of the Body - pages 695-738 d) 4. Activated helper T cell secretes cytokines that act as paracrines, autocrines Presentation to cytotoxic T cells, Figure 18-13, page 712 a) Any cell with class I MHC can act as APS for a cytotoxic T cell b) Antigens that complex with class I MHC arise within the body's cells - they are endogenous (1) Virus infected cells (virus can not trigger immune response since it is in a cell) (a) The resident virus causes foreign protein to end up in the cell membrane of the host (b) The foreign protein is complexed with the Class I MHC (c) This complex can then be bound by antigen-specific cytotoxic T cells (2) Cancer cells (a) Cancer cells also produce "foreign" protein and it complexes with the Class I MHC in the plasma membrane (b) This complex can then be bound by antigen-specific cytotoxic T cells (c) Oncogenes genes that have been altered and generate cancerous tissue 5. H. Natural killer cells a) Distinct class of lymphocytes b) Functions (1) Target virus infected cells and cancer cells (2) Attack and kill target cells directly c) Not antigen specific - require no prior exposure and no antigen presentation d) Not known if there is an MHC restriction, e) Why not cover under non-specific immunity? (too complex) Development of immune tolerance: Self versus Not-Self or how does body recognize its own proteins? 1. Clonal deletion a) T cells are exposed to variety of self proteins in utero and postnatal by unknown mechanism the thymus cells destroy the cells that “recognize” these proteins and they are destroyed via apoptosis b) Thus the cells which would destroy self proteins are themselves destroyed early in life 2. Clonal inactivation a) Some proteins do not pass through thymus Page 12 of 22 Chapter 18 - Defense Mechanisms of the Body - pages 695-738 b) I. By unknown mechanism self-reactive T cells are inactivated 3. Mechanisms? a) Costimulus is not provided in early development so T cell is not activated b) This can occur later in life also Antibody-mediated immune responses: defenses against bacteria, extracellular viruses and toxins; Table 18-5, page 713 and Figure 18-14, page 714 1. In peripheral lymphoid organs, bacterial antigen binds to specific receptors on the plasma membrane of B cells. 2. Simultaneously, antigen-presenting cells (for example, macrophages) (APCs) present to helper T cells processed antigen complexed to MHC Class II proteins on the APCs and secrete IL-1 & TNF, which acts on the helper T cells. 3. In response, the helper T cells secrete IL-2, which activates the helper T cells to proliferate and secrete IL-2 and other cytokines. These activate the antigen bound B cells to proliferate and differentiate into plasma cells. Some of the B cells differentiate into memory cells rather than plasma cells. 4. The plasma cells secrete antibodies specific for the antigen that initiated the response, and the antibodies circulate all over the body via the blood. 5. Antibodies combine with antigen on the surface of the bacteria anywhere in the body. 6. Presence of antibody bound to antigen facilitates phagocytosis of the bacteria by neutrophils and macrophages. It also activates the complement system, which further enhances phagocytosis and can directly kill the bacteria by the membrane attack complex. It may also induce antibody-dependent cellular cytotoxicity mediated by NK cells that bind to the antibody's Fc portion. 7. B cells undergo great cytoplasmic expansion, especially granular endoplasmic reticulum as they become plasma cells (plasma cells belly up in a day or two after producing millions of antibodies) a) Memory cells - some plasma cells become memory cells which can respond later in a rapid fashion b) The antibodies travel everywhere in the extracellular fluid and "attack" their specific antigen c) Antibodies play two roles in immune response (1) Initial recognition on B cells (2) Circulating antibodies bind to bacteria bearing the same antigen, marking them as targets to be attacked 8. Antibody secretion a) Plasma cells produce thousands of antibodies until they die within a day or two Page 13 of 22 Chapter 18 - Defense Mechanisms of the Body - pages 695-738 b) 9. 10. IgG (gamma globulin) - most abundant plasma antibody c) IgM - provide bulk of antibodies against bacteria and viruses d) IgE - mediate allergic responses e) IgA - secreted by gastrointestinal, respiratory, genitourinary tracts and breast milk f) IgD - unknown function g) ALL ANTIGEN-ANTIBODY COMPLEXES ENHANCE THE INFLAMMATION RESPONSE The attack: effects of antibodies a) Direct enhancement of phagocytosis (1) The presence of an IgG antibody-antigen complex enhances phagocytosis (2) Acts as an opsonin - Figure 18-14, page 708 (3) Phagocyte has Fc receptors b) Activation of complement system – Figure 18-15, page 716 (1) The most important mechanism for antigenantibody complex enhancing inflammation is the via the complement system (2) Classical complement pathway (a) C1 binds to complement receptors on the Fc portions of the antibody (IgG and IgM) that is combined with antigen (b) This activates the enzymatic portion of the complement pathway (c) The C1 will attach to all classes of immunoglobins and that is why it is such a powerful enhancer of the inflammatory response. c) Antibody-dependent cellular cytotoxicity (ADCC) (1) Complement (C1) and a phagocyte can bind nonspecifically to Fc (2) NK cells can do the same (3) The NK cells secrete cytotoxins but there must be antibody present (ADCC) d) Direct neutralization of bacterial toxins and viruses (1) Toxins can trigger immune response via antibodies (2) The antibody-antigen complex can form chains which can then be phagocytized (3) The toxin or viruses can not then enter or do damage to the body or cells Active and passive humoral immunity Page 14 of 22 Chapter 18 - Defense Mechanisms of the Body - pages 695-738 a) Time for immune response? - First challenge takes several days to produce antibodies, Figure 18-17, page 717 Vaccine may consist of attenuated microbes, toxins are harmless antigens c) Subsequent challenges have almost immediate effect d) Active immunity is what has been discussed thus far e) Passive immunity is through mother's breast milk and through injection of antibodies such as in pooled gamma globulin Defenses against virus-infected and cancer cells, Figure 18-18, page 718 1. Introduction a) Previous immune response was about “exogenous antigens” b) This section deals with how cells infected with viruses or are cancerous are dealt with by cytotoxic T cells, NK cells and activated macrophages c) How the body's own cells are killed 2. Role of cytotoxic T cells b) J. a) b) Similar to antibody-mediated immunity macrophages process and present antigens in association with the macrophage's Class II MHC proteins to helper T cells Helper cells respond to stimulation by TNF & IL-1 and release IL-2 (1) Acts as autocrine to stimulate helper T cell proliferation (2) The IL-2 also activates cytotoxic T cells and NK cells to proliferate and attack the target cells Gamma interferon (a lymphokine) secreted by helper T cells and by NK cells where it acts as an autocrine for cytotoxic T cells c) Cytotoxic T cells release cytoplasmic secretory vesicles by exocytosis into extracellular space between itself and target cell d) The vesicles contain pore-forming protein that insert into the target cell's membrane perforin e) The target cell becomes leaky and loses cytoplasm, etc. Role of NK cells and “activated macrophages”, Figure 18-19, page 719 a) These two destroy virus-infected and cancer cells also b) Major signal is IL-2 and interferon-gamma secreted by helper T Cells (3) 3. Page 15 of 22 Chapter 18 - Defense Mechanisms of the Body - pages 695-738 c) 4. 5. 6. NK cell response is non-specific but requires a specific response by helper T Cells to trigger response secrete cytotoxins d) Macrophages can be activated also by this mechanism an are called activated macrophages secrete tumor necrosis factor (TNF) Interleukin 1 (IL-1), TNF and IL-6 (Interleukin 6) - secreted by macrophages and is required by lymphocytes for activation Table 18-6, page 720, summary of host responses to viruses Role of macrophages in immune response, MAIN CELLS INVOLVED Nonspecific defenses Anatomical barriers Inflammation Interferon COMMENT ON ACTION Body surface linings Tissue macrophages Most cell types after viruses enter them Physical barrier; antiviral chemicals Phagocytosis of extracellular virus Interferon nonspecifically prevents viral replication inside host cells Antibody-mediated Plasma cells derived from B cells secrete antibodies Direct cell killing Cytotoxic T cells, NK cells, and activated macrophages Antibodies neutralize virus and thus prevent viral entry into cell Antibodies activate complement, virus Antibodies recruit NK cells via cytotoxicity Via secreted chemicals, destroy host cell and thus induce release Activity is stimulated by IL-2 and interferon-gamma. Specific defenses VI. Systemic manifestations of infection, Figure 18-20, page 721 A. Acute phase response B. Most significant is the secretion of endogenous pyrogens which reset the hypothalamus thermoregulatory center and cause "fever" (up to a certain point an elevated temperature is probably beneficial to the organism) 1. Plasma concentration of iron and zinc decrease and are thus unavailable for bacteria to reproduce 2. Loss of appetite deprives microbes of nutrients 3. Acute phase proteins - liver secretes these during stress and they effect inflammatory process, immune cell function and tissue repair 4. Bone marrow releases neutrophils and other granulocytes (granulopoiesis) 5. Release of amino acids from muscle for synthesis of proteins to fight infection and for tissue repair C. Colony-stimulating factors - stimulate bone marrow to produce more neutrophils and monocytes D. Role of macrophages in immune response, Table 18-7, page 722 1. In nonspecific inflammation phagocytize particulate matter, including microbes. Also secrete antimicrobial chemicals and protein messengers (cytokines) that function as local inflammatory mediators. The inflammatory cytokines include IL-1 and TNF Page 16 of 22 Chapter 18 - Defense Mechanisms of the Body - pages 695-738 2. 3. Process and present antigen to helper T cells. Secrete IL-1, which stimulates helper T cells to secrete IL-2 and to express the receptor for IL-2. 4. During specific immune responses, perform same killing and inflammation inducing functions as in (1) but are more efficient because antibodies act as opsonins and because the cells are transformed into activated macrophages by IL-2 and gamma interferon, both secreted by helper T cells. 5. Secrete IL-1, TNF, and IL-6, which mediate many of the systemic responses to infection or injury, VII. Factors that alter the body's resistance to infection A. The term resistance is difficult because so many factors come into play - generally it is all the immune factors working in concert to protect the body and it can either be optimal or below optimal B. Examples that lower resistance 1. Protein-calorie malnutrition (PCM) - poor nutrition is directly linked to lowered immune response 2. Preexisting disease - e.g., diabetes, or an injury 3. Congenital defects - boy in a bubble 4. Acquired immune deficiency syndrome (AIDS) - no cure 5. Prolonged stress - more later C. Antibiotics - drugs that can selectively kill pathogens (especially bacteria but not viruses) and not harm the host too much VIII. Harmful Immune Response A. Graft rejection 1. Cytotoxic T cells are mainly responsible 2. Half of the genetic make up of the placenta is foreign tissue to mother a) Why doesn't mother reject? b) Trophoblasts may not present adult MHC class I proteins but rather an "acceptable" form c) Much more to learn about this B. The Fetus as a graft C. Transfusion reactions and blood types 1. ABO system, Table 18-8, page 725 a) This is an atypical system in that the individual can have antibodies for an antigen without prior exposure - called natural antibodies (may be induced from intestinal bacteria) (1) A person has B antibodies, B person has A antibodies, AB has neither and O has both A and B antibodies (2) No one has anti-O antibodies b) Natural antibody production is unknown (antibodies without prior exposure) otherwise c) No such thing, in practice, of universal donor or recipient, must do direct cross matching Page 17 of 22 Chapter 18 - Defense Mechanisms of the Body - pages 695-738 d) Rh factor - requires prior exposure Rh incompatibility Rh-negative mother bearing Rh-positive child (2) Antigens cross placental barrier and mother synthesizes antibodies - for first child it happens at parturition so not dangerous, subsequent births may be jeopardized (3) Give mother rhogam, antibodies that bind to antigens of RBCs that might have entered mother's circulation and prevent them from inducing antibody production (a clinical "blocking antibody" so to speak) Allergy (Hypersensitivity Reactions), Table 18-9, page 726 a) Some people show immune responses to environmental factors such as dust, ragweed etceteras, called allergy or hypersensitivity (1) Can be very debilitating to fatal (2) The phenomenon is paradoxical since the response is not warranted by the antigen (3) There is immediate responses and delayed hypersensitivity like poison oak (4) (Discuss misuse of the word allergy) b) Immediate hypersensitivity, Figure 18-21, page 727 (1) The antibodies involved here are of the IgE class (2) Attach to mast cells and stimulate the release of histamine, chemotaxins for eosinophils and the synthesis of prostaglandins in the mast cells (3) All this leads to a local inflammatory response which in the respiratory system can be severe (4) If inflammatory response goes beyond local that can lead to anaphylactic shock which can be fatal, as in a bee sting (5) Treatment is with antihistamines and/or cortisols in extreme situations (6) The normal role of this response and IgE antibodies and eosinophils is in the body's defense against parasitic worms Autoimmune disease a) Recognized as autoimmune in origin (1) Multiple sclerosis (2) Myasthenia gravis (3) Rheumatoid arthritis (4) Insulin-dependent diabetes mellitus b) Normally the lymphocytes that would attack self are destroyed or suppressed in fetus and early infancy (1) 2. 3. Page 18 of 22 Chapter 18 - Defense Mechanisms of the Body - pages 695-738 (1) 4. 5. 6. This is an unanswered question. It is not known how the immune system determines self and not-self (2) See Scientific American, December, 1990, page 106, Trends in Immunology: The Body Against Itself by John Rennie c) Possible causes of autoimmune attack, Table 18-10, page 728 (1) There may be failure of clonal deletion in the thymus or of clonal inactivation in the periphery (2) Normal body proteins may be altered by combination with drugs or environmental chemicals. This leads to an attack on the cells bearing the now--foreign" protein. (3) In immune attacks on virus-infected bodily cells, so many cells may be destroyed that disease results. (4) Genetic mutations in the body's cells may yield new proteins that serve as antigens. (5) The body may encounter microbes whose antigens are so close in structure to certain of the body's own proteins that the antibodies or cytotoxic T lymphocytes produced against these microbial antigens also attack cells bearing the self proteins. (6) Proteins normally never encountered by lymphocytes may become exposed as a result of some other disease. Excessive inflammatory responses to microbes a) In systemic immune response the mediators can cause harmful responses such as IL-1 and TNF b) Septic shock can result c) Excessive inflammation caused by HIV which causes microglia to produce large amounts of inflammatory cytokines that are toxic to neurons d) This same mechanism may be implicated in Alzheimer's disease Chronic inflammatory diseases – asthma, rheumatoid arthritis and inflammatory bowel disease Immune-privileged sites and tissues (NOT IN TEXT) a) Immune-privileged sites are regions of the body where grafts of foreign tissue survive for extended periods (even indefinitely), compared to conventional (nonprivileged) sites. b) Sites and tissues (1) Anterior chamber of the eye (2) Cornea (3) Retina Page 19 of 22 Chapter 18 - Defense Mechanisms of the Body - pages 695-738 IX. (4) Brain (5) Hair follicles (6) Cartilages (7) Liver (8) Adrenal cortex (9) Pregnant uterus (10) Placenta (11) Ovary (12) Testis (13) Prostate (14) Tumors (15) Hamster cheek pouch SUMMARY AND GLOSSARY, TABLE 18-11, PAGE 729-730 SECTION B - NONIMMUNE METABOLISM OF FOREIGN CHEMICALS X. Introduction, Figure 18-22, page 736 A. Foreign chemicals are chemicals that have been synthesized since the industrial revolution and not enough time has passed for evolutionary adaptation - there are about 10,000 in common use B. Immune system can not handle most of them but rather they undergo biotransformation or excretion or storage XI. Absorption A. Many chemicals can move into body through G.I. tract since it is rather undiscriminating B. Some substances are absorbed through the lungs, especially airborne metals 1. Substances that enter lung are not subject to possible biotransformation in liver as ones absorbed by intestine 2. Substances toxic to liver are also avoided by liver C. Lipid solubility is critical for penetration through skin of oils, steroids and other lipids and for things dissolved in them! (DDT) D. The placenta is quite vulnerable to passage of foreign substances XII. Storage Sites A. Cell proteins, bone and adipose tissue B. The storage sites are in equilibrium with the blood and the substances can move in and out as plasma concentration changes C. Storage sites can be damaged by presence of substance or it can be "protective" XIII. Excretion A. To be excreted a substance must be filtered or secreted across renal tubule 1. Small unbound molecules may be filtered 2. Protein bound molecules are not filtered and this can be a mixed blessing B. Once the substances are in the tubule they may be transformed to more polar substance so they are not reabsorbed or they may be Page 20 of 22 Chapter 18 - Defense Mechanisms of the Body - pages 695-738 reabsorbed and just keep circulating like the enterohepatic circulation XIV. Biotransformation A. Mainly in liver but can occur kidney, skin, placenta 1. Most are transformed into more polar, less lipid-soluble substances and may be rendered less toxic or it can be made toxic! (The process does not make value judgments) 2. Microsomal Enzyme System (MES) - hepatic enzymes located in the hepatic cells smooth endoplasmic reticulum a) System is inducible b) Some substances can inhibit the MES XV. Inorganic Elements A. Heavy metals like mercury and lead B. G.I. tract does not readily absorb these but lungs can C. Not easily dealt with by body and can be dangerous, e.g., lead poisoning SECTION C - RESISTANCE TO STRESS XVI. A. B. XVII. A. B. XVIII. A. Introduction Stress - anything that causes the cortisol levels of the blood to increase - varies widely among individuals Pathway for cortisol- Figure 18-22, page 729 1. Corticotropin releasing hormone 2. ACTH 3. Cortisol Functions of Cortisol in Stress, Table 18-12, page 730 Functions (all covered previously) 1. Effects on organic metabolism a) Stimulation of protein catabolism b) Stimulation of liver uptake of amino acids and their conversion to glucose (gluconeogenesis) c) Inhibition of glucose uptake and oxidation by many body cells ("insulin antagonism") but not by the brain d) Stimulation of triacylglycerol catabolism in adipose tissue, with release of glycerol and fatty acids into the blood 2. Enhanced vascular reactivity, that is, increased ability to maintain vasoconstriction in response to norepinephrine and other stimuli 3. Unidentified protective effects against the damaging influences of stress 4. Inhibition of inflammation and specific immune responses 4. Inhibition of inflammation and specific immune responses Cortisol's pharmacological effects and disease - effects on body due to LARGE doses (hard to interpret) Functions of the Sympathetic Nervous System in Stress - Fight or Flight Functions, Table 18-13, page 731 Page 21 of 22 Chapter 18 - Defense Mechanisms of the Body - pages 695-738 1. 2. B. XIX. A. B. C. Increased hepatic and muscle glycogenolysis Increased breakdown of adipose tissue triacylglycerols providing glycerol for gluconeogenesis and fatty acids for oxidation 3. Decreased fatigue of skeletal muscle 4. Increased cardiac output secondary to increased cardiac contractility and heart rate 5. Shunting of blood from viscera to skeletal muscles by means of vasoconstriction in the former beds and vasodilation in the latter 6. Increased ventilation 7. Increased coagulability of blood Excessive, prolonged stress is major health problem in U.S. (Discuss) Other Hormones Released During Stress Aldosterone, vasopressin, growth hormone, glucagon Insulin is usually decreased Endorphin and B-lipotropin secretions are increased Page 22 of 22


![Immune Sys Quiz[1] - kyoussef-mci](http://s3.studylib.net/store/data/006621981_1-02033c62cab9330a6e1312a8f53a74c4-300x300.png)