MECHANICAL VENTILATION
advertisement

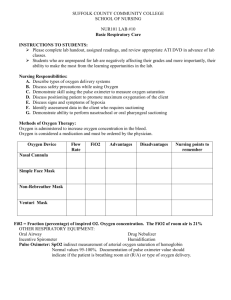
MECHANICAL VENTILATION I. Outcome Goal: Optimal ventilation and oxygenation will be maintained with mechanical support. II. Policy: Patients requiring mechanical ventilation will receive care as outlined. Licensed staff involved in direct patient care of patients requiring mechanical ventilation should exhibit knowledge of basic principles of mechanical ventilation, arterial blood gas interpretation, safe management of ET tubes, basic principles of pulmonary toilet, modes of mechanical ventilation, and emergency airway management in cases of mechanical failure or unplanned extubation. III. Specific Information: A. Endotracheal intubation 1. May be performed by: a. MD b. Trained Respiratory Care Practitioner c. Lifeflight RN 2. No more than 3 attempts at intubation should be made by any individual. B. Maintenance of mechanical ventilation 1. May be performed by: a. MD b. RN c. Licensed Respiratory Care Practitioner (RCP) 2. No more than 3 attempts at intubation should be made by any individual. IV. Equipment/Supplies: A. Ventilator B. Oxygen and air source C. Suction equipment / supplies D. Personal protective equipment E. Manual resuscitator bag F. PEEP valve (ONLY if patient is requiring PEEP > 5cm H20) G. Pulse oximeter V. Protocol: A. Ventilator settings and changes require either a physician order or may be made based on approved protocols (i.e. Weaning Protocols or Acute Lung Injury Protocol). 1. Mode of ventilation 2. Ventilation rate 3. Tidal volume 4. FiO2 5. PEEP 6. Pressure Support B. A qualified MD or RCP will make routine changes to ventilator settings. C. The RN may implement changes for oxygen concentration. D. In the event of any emergency, when neither a qualified MD or RCP are available, the RN should maintain a patient’s ventilatory needs with manual resuscitation. E. Patients receiving mechanical ventilation will have continuous SpO2 F. Repositioning / securing ETT tape requires 2 staff members (one of which should be an RCP, RN or MD). VI. Procedure(s): A. Securing position of ETT: 1. ETT should be secured with cloth tape (adhesive may be used as indicated), with an approved ETT holder device or with trach ties. 2. Change ETT securing device when it becomes soiled / soaked. 3. ETT should be moved to the opposite side of the mouth when ETT securing device is changed or soreness / redness is noted unless contraindication by patient condition / MD order. 4. Proper position of ETT is verified by auscultation of breath sounds, noting tube depth at lip / teeth line, and monitoring X-ray results. B. Suctioning using in-line suction device (preferred method) NOTE: This practice helps to maintain the integrity of a closed circuit in an effort to reduce ventilator-associated pneumonia. 1. The in-line method should be used exclusively if patient is requiring PEEP > 15. 2. Suctioning frequency is determined by patient need – amount of secretions, respiratory pattern / workload, SpO2, breath sounds 3. Personal protective equipment (mask, eye shield, gloves) should be worn by the care provider (s) during the suctioning procedure. 4. Hyperoxygenate with 100% oxygen before and after each suctioning “pass” unless contraindicated. The SpO2 should be allowed to return to baseline in between suctioning passes”. Some patients require long recovery periods. 5. Apply intermittent suction during withdrawal of suction catheter. Entire suctioning "pass" should not exceed 10 seconds. 6. Suction pressure should not exceed 150 mmHg or as outlined by unit protocol. C. Suctioning using sterile catheter / kit 1. Suctioning frequency is determined by patient need – amount of secretions, respiratory pattern / workload, SpO2, breath sounds. 2. Personal protective equipment (mask, eye shield, gloves) should be worn by the care provider(s) during the suctioning procedure. 3. Hyperoxygenate with 100% oxygen before and after each suctioning “pass” unless contraindicated. The SpO2 should be allowed to return to baseline in between suctioning “passes”. 4. Using sterile technique, apply intermittent suction during withdrawal of suction catheter. Entire suctioning “pass” should not exceed 10 seconds. 5. Suction pressure should not exceed 150mmHg or as outlined by unit protocol. D. Transporting patients receiving mechanical ventilation Patients will receive the same level of care and monitoring during transport as provided in the patient care unit. Call Respiratory Care Department as soon as possible to arrange for a Respiratory Therapist to accompany patient during transports both in hospital and outside. E. Weaning from mechanical ventilation 1. Weaning can be accomplished according to unit / department protocol or MD order. 2. The patient should be regularly monitored for tolerance of changes in ventilatory support. VI. Nursing Implications: A. Assessment 1. Verify position of ETT in reference to lip / teeth with securing device change and position change (minimum q shift). 2. Assess skin condition around ETT / oral mucosa q shift. 3. Verify ventilator settings q shift and with order changes. 4. Continuously monitor patient for tolerance of ventilator support (minimum every 2 hours) a. breath sounds b. respiratory rate / pattern c. SpO2 d. Peak inspiratory pressure e. Exhaled tidal volume / Minute Volume f. Amount / consistency of secretions g. Response to suctioning / ventilator changes / activity h. Anxiety B. Interventions 1. Sedation should be considered to optimize patient comfort. 2. Provide a means for patient to communicate with family / staff - pen / paper, letter board, etc. 3. Keep patient / family informed of progress, plan of care, and anticipated outcomes. 4. An oral airway may be used if patient bites or gums ETT. It should be removed and oral mucosa assessed q 24 hours. 5. Notify MD for: a. SpO2 < 90% or change greater than 5% b. Unplanned extubation c. Respiratory distress d. Inadequate sedation e. Increased peak airway pressure VII. Patient/Family Education: A. Orientation to unit / equipment B. Rational for mechanical ventilation C. Anticipated outcomes of ventilator therapy D. Methods of communication VIII. Documentation: A. Assessment parameters as outlined. B. Ventilator changes will be documented on the ventilator flowsheet, and the patient care flowsheet. C. Patient / Family Education. D. Other documentation as per unit guidelines. IX. Cross References: A. Clinical Policy Manual CL 30-02.01 "Clinical Practice Guidelines CL 30-05.01 "Pathway" B. Operations Manual OP 10-16 "Patient Restraints" OP 20-11 "Patients on Artificial Mechanical Ventilation" C. Comprehensive Accreditation Manual for Hospitals: PF.3.3, PF.1.1, PF.2 . X. References: Carrol P. Closing in on Safer Suctioning, RN 1998; 61 (5); 22-6 Crimlisk, JT, Paris R, McGonagle, EG. The closed Tracheal Suction System: Implication for Critical Care Nursing. Dimensions of Critical Care Nursing 1994; 13 (6):292-300. Hagler, DA, Tranver, GA. Endotracheal Saline and Suction Catheters: Sources of Lower Airway Contamination. American Journal of Critical Care. 1994; (3) 6;444-7 DePew CL, Moseley MJ, Clark EG, Morales CC. Open vs Closed-system Endotracheal Suctioning: a Cost Comparison. Critical Care Nurse 1994; 13(1); 94-100. XI. Distribution: A, B, C, D, F XII. Endorsement: Practice Committee - September 2000