Dr Henrik Malchau`s Service
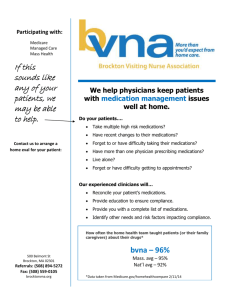
advertisement

Dr Henrik Malchau’s MGH Service 2009 Clinical Secretary: Research Secretary: Direct line to office: Mobile phone: Mrs Linda Comeau 617 643 1322 Ms Betty Gilman 617 726 3866 47548 617 331 1055 Schedule: Monday – Research Tuesday – OR in afternoon following Dr Rubash’s AM OR; occasional full OR day Wednesday- Morning clinic of 10-15 patients; usually done by noon or 12.30pm; dictations to follow clinic Thursday – Research usually; one full OR day monthly; assisting in Dr Bedair’s OR monthly Friday – Research Care and rounding of Drs McCarthy/Bedair patients as needed. OR cases Templating: Please see appendix for MDesk instructions; the fellow is expected to template, select the implants, confirm the implant requests (with the reps), and submit the instrumentation & equipment sheet (via email) to Mrs Linda Comeau (at the latest by the Thursday before the Tuesday OR); the MDesk template and implant choice are usually reviewed informally the week before the Tuesday/Thursday OR on Monday/Tuesday/Wednesay while walking back to Dr Malchau’s office after morning conference Implant Selection: RSA cases: Biomet Regenerex Cup, E poly, Taperloc Stems; with tantalum beads Primary hips: Smith & Nephew R3 cups and Spectron (cemented) or Synergy (uncemented) stems; Zimmer ML taper or Biomet taperloc stems PRN depending on the templating Smith & Nephew Birmingham Resurfacing; always also template the femur with a Synergy stem for contingency should the resurfacing procedure be aborted Revision Hips: Smith & Nephew Spectron primary or revision long-stem (cemented) Stryker Restoration or GMRS tumour prosthesis systems Depuy SROM Allograft struts with cables Cobalt cement on ice Post-operative protocol Drains & catheters out POD1; DVT prophylaxis with LMWH for 10 days postop; generally WBAT, but should confirm for patients who have had hip resurfacing Appendix MDesk Computer Templating Save image (that contains marker ball) as JPeg file Open MDesk and select ‘New Session’ under ‘File’ Open pelvis radiograph Select ‘Tools’, then choose ‘Open measuring guide’; then select ‘calibration’ (sphere scaling – 30mm) Select ‘Tools’ again and choose ‘Open measuring guide’ once more; but then select ‘basic-Pelvis.mmg Preoperative Planning’ (1st column, 2nd row) Follow instructions on side-bar afterwards; user can go back by choosing ‘Undo’ under ‘Edit’ tab; and then choose ‘Play’ on side-bar to resume templating Print image in landscape format for reference Implant Reps Zimmer Ed Mahoney (617 538 4560) Biomet Vince Palmer (781 799 6533) John McDonough (617 640 3833) Depuy Lou Silva (781 764 5626) Stryker Ed McVeigh (617 413 3525) John Sheehan (781 964 4334) Discharge Summary Templates Please call Dr Malchau, your PCP or report to the Emergency Department if you have any nausea, vomiting, fever greater than 101.5, swelling, chest pain, shortness of breath, increased pain/redness/drainage from your incision sites, numbness/tingling, or any other concerning symptoms. ACTIVITY: Weight-bearing as tolerated. MEDICATIONS: Take all medications as prescribed and resume home medications. Take a stool softener if taking narcotic pain medications. Stool softeners work better if you drink adequate amounts of fluid, ideally water. Try and drink 6-8 glasses of water a day, unless otherwise contra-indicated. If you are taking a stool softener but have not had a bowel movement in 3 days, please call the office and we will recommend alternatives. Taper down pain medication use as tolerated. No driving or operating heavy machinery while using narcotic pain medications. ANTICOAGULATION: Common symptoms of DVT/blood clots include: Localized pain, swelling, calf tenderness, redness or discoloration of the skin. PE symptoms include: shortness of breath, rapid pulse, sweating, chest pain that worsens with inspiration, coughing up blood, light headedness, feelings of apprehension. If you experience any of these symptoms call the office or go to the closest Emergency Department. WOUND CARE: Keep your incision clean and dry. You can shower but should not tubbath or submerge your incision. Prior to any wound care please wash and dry your hands. Place a dry sterile dressing over the wound each day if there is drainage, otherwise you can leave it open to air. The visiting nurse or rehab facility can remove the staples on post-op day 14 and place steri-strips across the wound. Leave the Steristrips in place until they fall off on their own. Walker or Crutches for ambulation. Please follow-up with Dr Malchau at the orthopaedic clinic in about 5-6 weeks from the date of surgery; call Mrs Linda Comeau at 617-643-1322 to make an appointment.