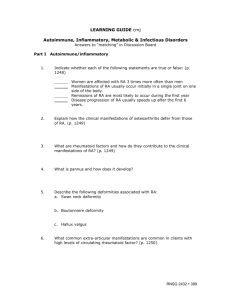
Learning Guide
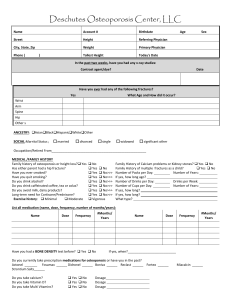
advertisement

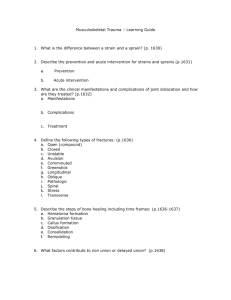
LEARNING GUIDE Musculoskeletal Disorders I. Osteomyelitis, Osteomalacia, Osteoporosis 1. Explain how an infecting microorganism can cause an infection of the bone including the indirect and direct entry, sequestra, and involucrum. 2. What are the clinical manifestations of osteomyelitis? 3. How do each of the following tests assist in diagnosing osteomyelitis? Blood and wound cultures WBC ERS Rationuclide bone scans MRI 4. What are medications used to treat osteomyelitis? What are common side effects and what patient teaching is important? 5. What type of surgery is performed to treat osteomyelitis? When is a wound vac used? Discuss related nursing care. 6. What other treatment measures are utilized in treating osteomyelitis and the related nursing care? 7. What is the most common cause of osteomalacia? What is the etiology? 8. What are the signs and symptoms of osteomalacia? 9. What laboratory tests are used in the diagnosis of osteomalacia? 10. What medications, foods, and treatment are used in correction of the vitamin D deficiency? 11. Why is osteoporosis more common in women than in men? 12. What is the etiology and pathophysiology of osteoporosis? 13. Why is osteoporosis called the “silent disease”? 14. What diagnostic tests are used to confirm the diagnosis of osteoporosis? 15. What foods are high in calcium? Why is vitamin D important in treatment of osteoporosis? 16. What medications are used in treatment of osteoporosis? What is the related patient Teaching? II. Pagets Disease 17. The bones of clients with Paget’s Disease are larger than normal but break more easily. Explain how/why this occurs. 18. What medications are used in the treatment of Pagets disease and related patient teaching? 19. What other supportive measures are important to teach the patient? III. Rheumatoid Arthritis 20. How does the autoimmune theory explain the etiology of rheumatoid arthritis? What is pannus and how does it develop? 21. What are rheumatoid factors and how do they contribute to the clinical manifestations of Rheumatoid Arthritis (RA)? 22. How does Rheumatoid arthritis affect joints? Describe the following deformities associated with RA: a. Swan neck deformity b. Boutonniere deformity c. Hallux valgus (bunion) 23. What are the extraarticular manifestations of RA? What are rheumatoid nodules and what problems do they cause? What are complications of RA? 24. What specific diagnostic tests are used to confirm the diagnosis of RA? 25. Complete the following grid for each of the medication types indicated: Medication ASA NSAIDS Corticosteroids A. Intra-articular injections B. Systemic (Solucortef) Disease modifying Drugs (DMARDS) A. *methotrexate (Rheumatrex) B. suflasalazine (Azulfidine) C. penicillamine (Cuprimine) (how to take) Gold Salts A. Parenteral gold sodium thiomalate (Myochrysine Antimamalarial A. Hydroxychlorog uine (Plaquenil) Mechanism of Action Key Side Effects/Nsg Implications-Key cautions Immunosuppressant A. azathioprine (Imuran) Biologic/targeted Therapy A. etanercept (Enbrel B. infliximab (Remicade) 26. Explain the following nursing interventions and related patient teaching for the patient with RA? Be able to explain how these will assist with preventing pain and deformities? IV. Gout 27. What is the difference between primary and secondary gout? What is hyperuricemia? Why do clients with chronic gout often develop kidney disease? 28. What are the clinical manifestations? What are tophi? 29. How is a definitive diagnosis of gout determined? (What lab results, such as uric acid level, etc) 30. Complete the table on medications used in treatment of gout: Medication Side Effects (major) Nursing Implications Colchicine p. 1716 Allopurinol p. 1716 Probenecid (Benemid) or Sulfinapyrazole (Anturane) p. 1716 Febuxostat p. 1716 * Why should aspirin NOT be given to client receiving probenecid? 31. Patients with gout are sometimes instructed to eat a low purine diet. Name several foods that the client should avoid. Why is a high fluid intake very important for the client with gout? 32. What else should the patient be taught as precipitating factors to gout attack? V. Systematic Lupus Erythematosus 33. Explain the “causes” (pathophysiology) of SLE? (p. 1717) What role do certain drugs such as hydralazine (Apresoline) play in the disease process? 34. What are the clinical manifestations related to multisystem involvement? Why do they occur? 35. Describe the anticipated findings for each of the following diagnostic tests for a patient with SLE: (p. 1717, 1718 -1719) Antinuclear antibody (ANA) Anti-DNA antibody ESR LE cell prep 36. Complete the table on medications used in treatment of SLE: Medication Steroid-sparing drugs (Methotrexate) Antimalarials (Plaquenil) Side Effects (major) Nursing Implications Immunosuppressive Cytoxan, Imuran 37. Patients with SLE often have impaired skin integrity. What should the nurse teach the client as to how to minimize these effects of the disease? Include role of photosensitivity and environmental factors that may trigger SLE. 38. What are important concepts to include in patient and family teaching and related nursing care? P. 1720-1723.