Enzyme Inhibition
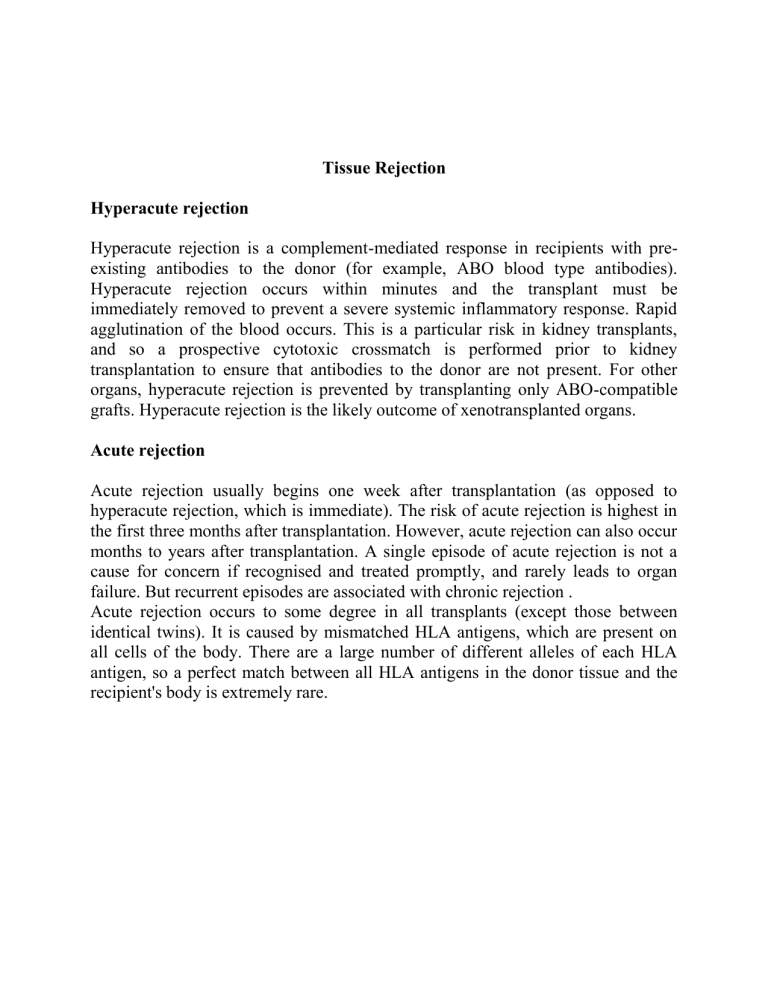
Tissue Rejection
Hyperacute rejection
Hyperacute rejection is a complement-mediated response in recipients with preexisting antibodies to the donor (for example, ABO blood type antibodies).
Hyperacute rejection occurs within minutes and the transplant must be immediately removed to prevent a severe systemic inflammatory response. Rapid agglutination of the blood occurs. This is a particular risk in kidney transplants, and so a prospective cytotoxic crossmatch is performed prior to kidney transplantation to ensure that antibodies to the donor are not present. For other organs, hyperacute rejection is prevented by transplanting only ABO-compatible grafts. Hyperacute rejection is the likely outcome of xenotransplanted organs.
Acute rejection
Acute rejection usually begins one week after transplantation (as opposed to hyperacute rejection, which is immediate). The risk of acute rejection is highest in the first three months after transplantation. However, acute rejection can also occur months to years after transplantation. A single episode of acute rejection is not a cause for concern if recognised and treated promptly, and rarely leads to organ failure. But recurrent episodes are associated with chronic rejection .
Acute rejection occurs to some degree in all transplants (except those between identical twins). It is caused by mismatched HLA antigens, which are present on all cells of the body. There are a large number of different alleles of each HLA antigen, so a perfect match between all HLA antigens in the donor tissue and the recipient's body is extremely rare.





![Immune Sys Quiz[1] - kyoussef-mci](http://s3.studylib.net/store/data/006621981_1-02033c62cab9330a6e1312a8f53a74c4-300x300.png)