Ergonomic Ultrasound Probe
advertisement
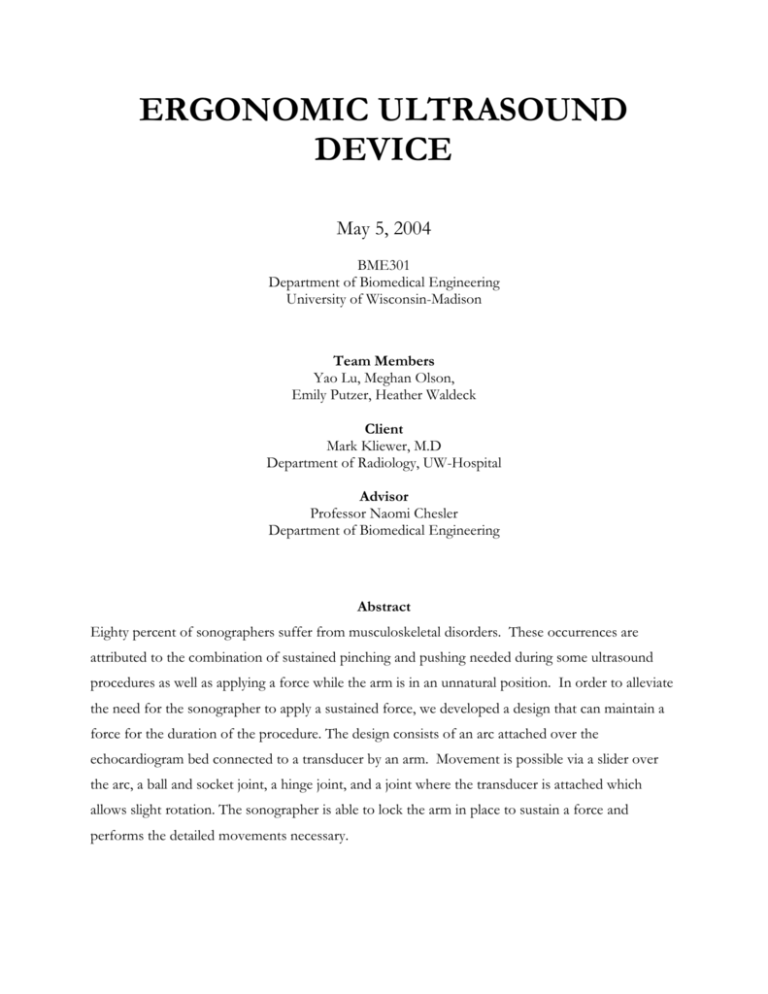
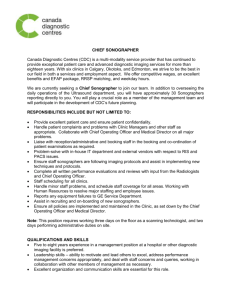
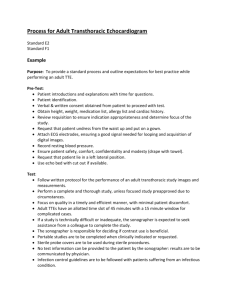
ERGONOMIC ULTRASOUND DEVICE May 5, 2004 BME301 Department of Biomedical Engineering University of Wisconsin-Madison Team Members Yao Lu, Meghan Olson, Emily Putzer, Heather Waldeck Client Mark Kliewer, M.D Department of Radiology, UW-Hospital Advisor Professor Naomi Chesler Department of Biomedical Engineering Abstract Eighty percent of sonographers suffer from musculoskeletal disorders. These occurrences are attributed to the combination of sustained pinching and pushing needed during some ultrasound procedures as well as applying a force while the arm is in an unnatural position. In order to alleviate the need for the sonographer to apply a sustained force, we developed a design that can maintain a force for the duration of the procedure. The design consists of an arc attached over the echocardiogram bed connected to a transducer by an arm. Movement is possible via a slider over the arc, a ball and socket joint, a hinge joint, and a joint where the transducer is attached which allows slight rotation. The sonographer is able to lock the arm in place to sustain a force and performs the detailed movements necessary. Problem Statement During echocardiogram and biopsy procedures, sonographers must apply high levels of pushing force with an unnatural arm position while performing detailed movements. The combination of these factors increases the number of work-related injuries and many times prevents the sonographer from performing their jobs. Our goal is to develop an ergonomic design which will minimize the forces applied and thereby reduce injuries to sonographers. Background Information Ultrasound is a widely used technique for imaging the inner organs of the body using sound waves. An ultrasound transducer (Figure 1) is used by a specialized technician called a sonographer to probe the outer surface of a patient’s body and produce a relevant image of the inner organs. The tip of the transducer made with a piezoelectric material and is used to sense sound waves given off from the body structures and convert them to electric signals so they can be made into an image. A gel must be used on the surface of the skin in order to propagate the sound waves, which do not travel through air. In addition to the transducer, a large console (made up of a keyboard and viewing screen) is used in an ultrasound reading to compile and display the image, make various adjustments, and change settings. 1 Figure 1: An ultrasonic transducer [Murphey] There are many types of procedures performed by sonographers using ultrasound. Two of the most time-consuming and fatiguing procedures are biopsies and echocardiograms [Kliewer]. A biopsy is performed by a doctor, who inserts a needle in a patient’s body, aiming to take a sample of a tumor. The doctor guides the needle using the image created by the sonographer, which must be very exact to include the small dimensions of the needle and to accommodate for the precise nature of the procedure. Similar to a biopsy, an echocardiogram has duration of approximately 45 minutes and can be made difficult in large patients who have excess skin and tissue surrounding the heart. The procedure images the heart of a patient to identify problems in heart valves or the function of the heart muscles. The sonographer must apply a large amount of force to the transducer in order to penetrate the tissue and circumvent the ribs to create a good image. The patient lies on his/her side (Figure 2) while the sonographer first applies pressure on a certain position on the patient’s chest and then on a position on the patient’s side in an upward direction through a hole in the bed. The latter position is to take advantage of the fact that, due to gravity, the patient’s heart will be more superficial and easier to image. [Kliewer] 2 Figure 2: An echocardiogram [The Franklin Institute] These types of procedures, especially the echocardiogram, require the sonographer to apply large amounts of force for long periods of time, while still needing to make detailed movements. These factors lead to a high incidence of musculoskeletal injuries. In fact, 80% of sonographers suffer from an injury such as this, most commonly in the neck, shoulder and/or wrist [Murphy]. Studies show that these disorders arise primarily because of the force needed in certain procedures (See Figure 3). It can also be noted that the pinching motion needed in conjunction with the force may cause problems as well by having the stretched tendons rub across the carpal bones thus causing swelling of the tendons. 3 Figure 3: Survey of sonographers – Tasks that aggravate musculoskeletal symptoms (Mean scores on a 5 point scale) [Murphy] Some of the main musculoskeletal injuries affecting sonographers are carpal tunnel syndrome, tendonitis, and shoulder bursitis. [Chattanooga Website] The former occurs in a region of the wrist that forms a tunnel of ligaments and tendons. When these structures become overused, as can happen with the repetitive movements made by a sonographer, they become inflamed and cut off the nerve that runs from the arm to the hand through the “carpal tunnel.” Tendonitis develops when the tendons in the wrist or elbow (connecting muscle to bone) become inflamed. Bursitis arise when the bursa (fluid filled sacs located at the joints) is inflamed, putting pressure on the joints and causing discomfort. The symptoms of all three musculoskeletal disorders mentioned can include pain, numbness, swelling, or weakness [Chattanooga Website]. A visual description of carpal tunnel syndrome, tendonitis, and bursitis is shown in Figure 4. 4 (a) (b) Figure 4: (a) Carpal Tunnel Syndrome [Everybody Health] (b) Shoulder Bursitis and Tendonitis [Orthopaedics Northeast] Due to the prevalence of the aforementioned injuries, many companies and research groups have tried to improve the current design and ultrasound procedure, all with little improvement. Companies have designed more ergonomic transducers with grooves or varied shapes that accommodate a palmer grip [Chattanooga Website]. Also, groups have urged sonographers to use proper posture and to stretch occasionally. However, these improvements have not lowered the incidence of injury because they do not eliminate the most important contributing factor: force applied for an extended period of time with an unnaturally positioned arm. Currently, research groups are working on more handle re-designs in the hopes of alleviating sonographer injuries. Client Requirements The client specified several requirements for the new transducer design. First, the design should not interfere in any way with the sonographer collecting the ultrasound data of the patient. Next, the design should minimize the force the sonographer must apply, especially the pushing force required for maintaining transducer position during a procedure. The design should also minimize 5 strain on the joints and muscles from being in unnatural positions to perform the procedures. While eliminating the current ergonomic problems, the design must not induce any new injuries upon the sonographers. Thirdly, since the ultrasound procedures of interest usually require small and precise movements of the transducer, the design must still allow for those movements. The design should also be capable of withstanding the various necessary forces such as those applied by the sonographer. Also, the device must be adaptable to varying situations like different sized patients, beds and various ultrasound transducers. Finally, the design must be user friendly, suitable for a hospital environment, and should not pose any danger to the patients or hospital staff. (See appendix A). Design Alternatives Handle Redesign The first design proposal is aimed at decoupling the push and pinching forces the sonographer must apply simultaneously during a procedure. The design is composed of three parts: a handle, the transducer, and a wrist splint (see Figure 5). Figure 5: The transducer is attached to the handle by a flexible attachment. The handle fits snugly into the palm of the hand. The wrist splint is not shown in diagram. 6 The transducer is attached to the handle but it is still free to rotate in any direction, allowing for the exact adjustments the sonographer must make. The handle will be composed of a firm but soft material, and it will fit tightly into the palm of the sonographer. The goal of this design is that the sonographer does not have to push with the small muscles of the fingers while pinching; instead he/she applies the pushing force with the palm, and still can use the agile fingers for small movements. The wrist splint is to help stabilize the sonographer’s wrist and forearm to reduce strain. The advantages of this design are that the transducer is still very mobile and therefore the ultrasound procedure will not be obstructed. The design also helps to prevent wrist and forearm strain since the sonographer does not have to apply a large pinching force. Also, there is the possibility of making the part of the handle in contact with the palm to be replaceable so that it is comfortable for people with many different sized hands. The main disadvantage of this design is that since the sonographer still must apply all the pushing force for the entire duration of the procedure, the strain on shoulder and upper arm is not reduced. Other issues include sanitation concerns since the handle and wrist splint may be difficult to clean. Also, the design may still be uncomfortable for the sonographer since the fingers are positioned around the transducer head in a slightly unnatural position. Transducer Redesign The second design proposed focused on redesigning the transducer completely in order to allow the hand to be in a more natural position. The main body of the transducer would fit around the sonographer’s hand. 7 Figure 6: Outside side view of second design option. Inside, there would be a handle, similar to a bicycle handle, which the sonographer would grip and with which they would apply the force. Figure 7: Bottom view of second design option showing the handle grip inside. The actual transducer portion of the design would be a separate piece that would be attached with some sort of elastic material to the main body. Figure 8: Top view of second design option. 8 Ideally, this method of attachment would allow the transducer portion of the design to move a small distance relative to the main body when the sonographer makes movements with his/her wrist. The main advantage with this design is that it allows the sonographer to apply the force with a very natural position of the hand thus reducing the strain on the fingers, wrist, and elbows. Also, the transducer would be able to be used for many procedures and by many different sonographers. The disadvantages, however, are that the design may not allow for the needed precise movements. Even if the elastic material did allow for very small movements, the sonographer would have to adjust to the subtleties of the types of wrist movements are needed which may be hard to adapt to. Also, this design does not eliminate the unnatural positioning of the arm used when applying the force and thus, the injuries to the shoulder would still be a problem. Thirdly, the elastic material used may cause sanitation concerns if it cannot be cleaned easily. Mechanical arm with Slider The third design’s main objective is to reduce or eliminate the constant force that must be applied by the sonographer during the long duration procedures. This design consists of an arc which is positioned above the bed and patient and a mobile arm which can move along the arc and lock into place. The arc itself will use clamps to attach to the sides of the bed (Figure 9A). The arm is attached to a slider (Figure 9B) which can move along the arc and can be locked at any position allowing for 180˚ adjustability. The arm itself is composed of two segments. The first segment is attached to the slider with a ball and socket joint allowing for 360˚ rotation which can also be locked in place. The second segment is attached to segment 1 through a hinge joint which allows for 180˚ mobility in one plane. This mobile capability should be sufficient since segment 1 has 360˚ rotation. Segment 2 is also unique in the sense that it is actually composed of two components: one hollow tube, and a smaller solid tube (Figure 9C). The solid tube is placed inside the hollow tube and is 9 allowed to move in and out of the hollow tube and can be locked in place with respect to the hollow tube. This allows for length adjustment in the arm, which is useful since not every patient is the same size. Finally, the transducer would be placed at site D in Figure 9, and connected to the arm segment with soft compression springs. The springs will allow the sonographer to make precise movements with the transducer, while helping to maintain stability of the entire system since a soft springs minimizes the force upon the system caused by normal movements of the patient or sonographer. B C D A Figure 9: Diagram of mechanical arm design. Consists of an arc, a slider (B), and an adjustable arm(C). The arc attaches to a hospital bed with clamps (A). The transducer is attached at site D. The idea of this design is that the sonographer applies an initial force that is needed during a procedure, such as an echocardiogram. The sonographer can then lock the joints of the arm so that the arm will maintain the position of the arm and thereby the force. This will eliminate harmful forces applied over a long period of time which causes injuries to the wrist and shoulder of the sonographer. The mechanical arm design has several advantages as well as disadvantages. The advantages include the versatile movement of the arm which allows for various positions needed in procedures. It also reduces the force applied by both the shoulder and wrist of the technician, is feasible to 10 produce and could be used in any hospital. Some disadvantages are that it is not efficient to use in all ultrasound procedures, it does not have the ability to make fast adjustments since the sonographer must unlock, move, and re-lock each segment to make large adjustments, and it may have overall system stability problems. Design Evaluation - Design Matrix To decide on a proposed design, a design matrix was used to evaluate the three design ideas (Table 1). The designs were assessed based upon seven requirements, with emphasis on ability to reduce force and make precise movements. The mechanical arm scored highest in these categories, and also has the highest overall score (higher scores are more favorable). Hence, the mechanical arm design is chosen as the proposed design. Handle redesign Transducer redesign Mechanical arm Ability to reduce force 1 1 3 Ability to make precise movements Comfort 2 1 3 1 2 3 Feasibility 3 1 2 Ease of use 3 2 2 Adaptability to different people 1 3 3 Lack of interference with procedures Total 3 2 2 14 12 *18* Table 1. Design matrix. Each design was evaluated with the criteria listed in the first column. Each criterion was given equal weight in the scoring. Each design was given a score from 1 to 3; 1=poor, 2=good, 3=excellent, based on its performance relative to the criteria. The handle redesign, transducer design, and Mechanical arm design scored 14, 12, and 18 respectively. The mechanical arm design was chosen for the final design based on these criteria. 11 Proposed Design - Prototype After consulting with various professors we as a team decided it would not be efficient to build a working prototype before building a model of our design. The exact mechanisms we would use on a working prototype are unclear and by making a model we can find and address potential problems that may arise in later production. Our prototype consists of a steel metal to simulate the transducer attachment, a ball and socket joint, a hinge joint, and a wood slider piece. The model was mounted on a two by four bar of wood for stability (figure 10). Figure 10. The finished model with all components assembled While producing the model we had several problems which need to be addressed. The first problem was that the slider piece design is unique and is not available for purchase from any store; therefore we have to fabricate this component. Professor Fronczak of UW-Madison suggested we use the rapid prototype machine (a procedure where a machine glues layers of paper together and cuts out a design with a laser to form a wood like model) to make a model of the slider. However John Ma (ME department) informed us that the arc shape of the hole in the slider would be difficult 12 to reproduce with rapid prototype machine. Our alternative was to construct the slider using the C and C mill machine with the help of Chris Arnold (ME department. Due to the arc shaped groove, we made two separate pieces. The first is a flat piece of wood for the side of the slider and the second is the bulk of the slider and consists of the hole for the arc. The two pieces were then fastened together using five screws (Fig 12). This procedure made a precise and accurate component. The dimensions of the slider are shown in Table 2. We plan on using the mill machine to fabricate our working prototype slider component using aluminum. b g a i c f h d e Figure 11. 13 Measurement Symbol on Figure Actual Dimensions (in) Radius of arc r 18 Length of slider l 6 One half of angle of arc covered by slider o 0.1667 (radians) Height of hole a 0.25 Width of hole - 0.76 Distance to bottom of hole c 1 Distance to top of hole b 0.75 Distance from side to hole - 0.5 Large length d 6.635 Small length e 5.641 Large height f 2.249 Small height g 1.973 Top of hole to bottom h 1.232 Bottom of hole to bottom i 0.968 Table 2 and Figure 11: Dimensions for the slider prototype. 14 Figure 12: Pictures of the actual slider prototype as it fits on to the arc. A second major problem while making the model was obtaining a metal arc. Metal arcs are not sold commercially so we must buy a straight bar and bend it to our required dimensions. The university does not have the appropriate equipment for bending bars of our length, therefore we obtained a welding steel bar (3/4 x 1/8 x 72 in.) that was easy to bend manually. We then proceeded to bend the bar around a circular object to obtain a 36 in. diameter arc. This method worked for our model but for our working prototype we will use a thicker and sturdier bar which we will not be able to bend without a machine. The cost of our model was relatively inexpensive. See Appendix B for list of costs quantity of the material used for the arc design model. The total cost of the model was approximately $75. While our model is not a functional prototype it gave us an advantage in addressing certain problems which would have came up in future production of the actual prototype. We now have a better grasp of how to manufacture our design and how it will work. Building a model before a prototype was a good decision and has given us a head start in building the prototype. 15 Future Work Our current prototype is not functional nor does it include several features we hope to incorporate into the final design. Several additions and improvements need to be made to the design of the arc, arm, and transducer portion of the device. Arc Design As of now, we do not have a way to attach the arc to the echocardiogram bed. On one side of the arc, a clamp is required which will attach to the bars on the bed as well as to the end of the arc which is perpendicular to the bars. Ideally, this clamp will be user-friendly in the sense that it will easily detach from the bed to allow rotation. On the other side of the arc, instead of attaching directly to the arc, the clamp will attach to a ball and socket joint which is used to rotate the arc under the bed. Depending on the type of ball and socket joint used, it may be positioned horizontally or vertically from the floor. However, horizontal placement would allow for a larger arc radius and also could make rotation under the bed easier, which is discussed further below. The clamp should also attach to a large length of the bar order to compensate for the torque that results from the force that is applied against the arc. Research into currently available clamps has found no commonly manufactured clamps that will work for our device. Therefore, it is likely that we will have to design and manufacture our own clamp. The site of attachment is also an issue which needs to be resolved. As of now, there are two likely bars on which the arc can be attached. One position is on the handle bars on the side of the bed and the other is a bar underneath the bed slightly inside the width of the bed. The handle bars have a rectangular shape and can more up and down. One problem which will need to be worked out is that the rotation of the arc may be hard to accomplish with our current design. If the arc is attached to the bar underneath the bed, the radius that the arc needs to be in order to correctly clamp to the bed will be different above the bed than below. One possible solution to this problem 16 is to make two attachment points on the clamp so that the attachment point is inside the arc diameter when it is under the bed. If the arc is attached to the handle bars, the rectangular shape of the handle bars will prevent rotation of the arc under the bed. One possible solution to this situation is to develop a method to have the arc clamp to both the top and bottom of the handle bar. Ideally, this method would be user friendly in that is would not require the sonographer to unclamp the arc, lift it, and reattach it to a different site. Another possible solution is to increase the radius of the arc so that the handle bar will not interfere with rotation. To do this, we can extend the clamp further out from the bed and/or use a ball and socket which extends parallel to the floor. The width of the bed is approximately 31.5 in.; even if we are successful in extending the diameter of the arc to, for example, 36 in., the radius, and thus the height of arc, is only 18 inches. This height would interfere with the procedure since a person of average size lying on their side would have a height of ~12 inches. The arm would not fit in the small space between the patient and the arc. Not to mention, that many patients are considered overweight and may not be able to fit under the arc at all. In order to compensate, we plan to make the arc height adjustable by attaching straight pieces at the ends of the arc. The straight pieces would consist of two pieces, one which fits inside the other, which would be able to extend above the bed. Ideally, the extendable piece would self lock while being extended and contain a release button to reduce the height. To make this design user friendly, only one side would lock while the other would have free movement. One last improvement that needs to be made to the arc is to construct the final arc out of stainless steel. This material is the most appropriate for a hospital environment as it will not cause irritation to the patient or the sonographer and is easy to keep sterilized. It also is also strong enough to maintain the force that will be applied. One problem that will need to be resolved is with the construction or the arc as we well need to find a way to bend the arc to the appropriate radius. 17 We are currently looking for a bending device that we may use. Some places that may be equipped to bend a bar are car shops and the physical plant science building. Slider Design The main problem with the slider is to find a way to lock it in place on the arc. Our current idea is to create a lock in the slider which when it is snapped closed applies pressure on the arc. This lock will need to be factored into the design of the slider. Another improvement which will need to be made to the slider is to find a method to prevent excessive friction between the arc and the slider. One possible solution is to place rollers on the inside of the slider where it comes in contact with the arc. Another possibility is to add a Teflon coating to the inside of the slider. In regards to the construction of the slider, we must decide whether to construct the slider as one or two pieces. Constructing it as two pieces is easier, but making one piece may be more stable. To construct the slider as one piece, we will need to employ the use of a mold since the curved groove cannot be made with other forms of construction. The exact dimensions of the slider can only be determined after the radius of the arc is decided. The equations used to determine the slider dimensions are shown below: a 18 b g a i c f h d e 13. Figure Measurement Symbol on Figure Equation Radius of arc r - Length of slider l - One half of angle of arc covered by slider o l/r (radians) Height of hole a - Distance to bottom of hole c - Distance to top of hole b - Large length d 2(r+a+c+b)sin(o) Small length e 2(r-c)sin(o) Large height f (r+a+b+c)-rcos(o) Small height g (a+c+b)cos(o) Top of hole to bottom h (a+c)cos(o) Bottom of hole to bottom i (c)cos(o) Table 3 and Figure 13 : The information and equations needed to determine the final dimensions of the slider piece. 19 Arm Design The main concern for the future development of the arm is to find a way to lock the joints so that they are able to hold the arm and therefore a constant force at a stable position. Our current idea includes placing pins in the joint to prevent movement. However, this may prove difficult for the joints we used in the prototype as they unexpectedly allowed more degrees of rotation than we desired. We also need to find an easy, user-friendly way to adjust the second arm. One possibility is to have the arm automatically lock to prevent contraction when it is being extended, then a release button can be used to allow contraction. This method would be accomplished by a series of groves or holes on the inner tube into which fits a retractable protrusion located on the inside of the outer tube. The release button would hold the button in the retracted position to allow free movement. We also need to determine the best materials for the construction of the arm. For example, we need to find a way to ensure stable connections between the joint and tubes since they will most likely not fit together perfectly. At this point, stainless steel tubes would be the best options for reasons similar to the arc design. Transducer Design The method of attachment for the transducer has room for improvement. We plan to incorporate soft springs (spring with a low spring constant) in order to allow the transducer to move slightly in response to small movements of the patients, such as breathing, without reducing the force apply a great deal. We also need to design a mechanism to allow sonographers to make small adjustments with the transducer. We can use a joint which places a circle of ball bearings in contact with the part of the transducer handle near the head to allow for small rotations about and axis. The transducer also needs to be removable for cleaning and well switching to different transducers. One small improvement we hope to make to the transducer itself in order to improve the comfort for the sonographer is to add a phalange to the head of the transducer. We could use this addition to make 20 improvements to the handle design in order to account for the change in procedure caused by the addition of the arc; the grip that the sonographer employs may be different since they will not need to be applying high forces with as they do with their current grip. One problem that may become an issue is the possibility of the transducer slipping off the patient during the procedure. This risk is greatly increased by the use of gel between the transducer and the patient to improve the ability to collect data. One possible solution is to have a separate, stable piece come in contact with the patient. The piece would be at the same level as the transducer head, does have any gel applied to it, and would not be subject to manipulation by the sonographer Thus it would prevent the arm from slipping while maintaining the force. Possible problems with this solution, however, is that it may interfere with the sonographer’s ability to manipulate the transducer depending on how it is designed and it also may be problematic to use on patients with excess adipose tissue: the sonographer would have to force a larger surface area (as compared to just the transducer head) into the tissue of the patient. Ethical Considerations Ethically we must produce the safest design possible. Since our proposed design sustains forces on a human body, we must be very careful to keep the patient from being harmed. To achieve this, extensive testing will need to be performed to ensure the proper performance of the device. All safety guidelines must be followed and no injury of the patient or the sonographer can result from testing. Another human factor to consider is aesthetics. The patients may already feel anxious about the procedure, and if our design appears unsafe rather than non-invasive medical equipment, he/she may become very uncomfortable; this is something we want to avoid. Finally, we need to build our design to accommodate various body sizes. Not all patients will easily fit below the arc; therefore, adjustability is necessary. Finally, we try to be considerate of the client’s budget 21 (see Appendix B for summary of costs); our goal is to minimize the cost of the prototype without sacrificing quality. Conclusions Currently the construction of a model of the mechanical arm design was successful in portraying the functionality of the prototype, and the next step of the project is to build a working device. The device will be tested repeatedly, both with the patients and sonographers to ensure the product meets the product specifications. The goal of the testing is to eliminate any flaws of the design and to make certain the device reaches its potential to alleviate discomfort to the sonographer. 22 References 1) Baker, J.P. Murphey, S.L. Ultrasound Ergonomics. Sound Ergonomics. Kenmore WA, USA. http://www.soundergonomics.com/PDF%20Files/SeimensWhitePaper.pdf 2) Everybody Health website. New Zealand. www.everybody.co.nz/gifs/carpal.jpg. Last accessed 4/29/04. 3) The Franklin Institute Online. sln.fi.edu/biosci2/monitor/images/echo.jpg. Last accessed 4/29/04. 4) Kliewer, Mark. UW Hospital. Radiology Dept. Personal Interview. January 2004. 5) Murphey, Susan L. Coffin, Carolyn T. Ergonomics and Sonographer Well-Being in Practice. Sound Ergonomics. LLC. 2002. http://www.soundergonomics.com/PDF%20Files/ErgSonWellBeing.pdf 6) Murphy, Carmel, MS. Russo, Andre, BS. An Update on Ergonomic Issues in Sonography. Healthcare Benefit Trust. July 2002. http://www.sdms.org/pdf/sonoergonomics.pdf 7) Orthopaedics Northeast Website. www.orthone.com/hand/shoulder.asp. Last accessed 4/29/04. 8) Work-Related Injuries and Scanning Ergonomics in Diagnostic Medical Sonography and Preventative Considerations. Sound Movements: Posturing the Profession. Ultrasonography website of Chattanooga State. 2002. http://www.chattanoogastate.edu/Allied_Health/index2.htm 23 PRODUCT DESIGN SPECIFICATIONS TITLE: ERGONOMIC ULTRASOUND PROBE MAY 3, 2004 YAO LU MEGHAN OLSON EMILY PUTZER HEATHER WALDECK FUNCTION: During echocardiogram and biopsy procedures, sonographers must apply high levels of force with an unnatural arm position while performing detailed movements. The combination of these factors increases the number of work-related injuries and many times prevents the sonographer from performing the procedures. Our goal is to develop an ergonomic design which will minimize the forces applied and thereby will reduce injuries to sonographers. CLIENT REQUIREMENTS: The design should: o Cause no interference with the collection of data. o Minimize force applied by sonographer o Eliminate the need to apply large, sustained forces. o Reduce strain on joints and muscles which occurs when applying a large force in an unnatural arm position. o Allow for precise movements and adjustments. o Be adaptable to different transducer models and consoles. o Be able to be held in a stable position while allowing for fine manipulations. DESIGN REQUIREMENTS: 1. PHYSICAL AND OPERATIONAL CHARACTERISTICS A. PERFORMANCE REQUIREMENTS: Device will be used at least 10 times per day. Duration of each use will vary depending on the medical procedures; duration will vary from minutes to hours. Device must withstand the force it takes to maintain appropriate contact with the patient as well as the force from the grip by the sonographer. Device will have direct contact with the patient and sonographer. Device must operate with the current console designs. B. SAFETY: No sharp edges are allowed. Any electrical components of the transducer must not be in contact with either the patient or the sonographer. The materials from which the device is constructed must not have potential toxic dangers. 24 C. ACCURACY AND RELIABILITY: Device shouldn’t interfere with the ultrasound procedure. Device must remain mechanically stable. Device must allow precise movements of transducer. D. LIFE IN SERVICE Device must operate for a minimum of 5 years. Device must withstand 8 hours of operation each day, seven days a week. E. SHELF LIFE Stored in hospital environment Shelf life of 10 years F. OPERATIONAL ENVIRONMENT Standard hospital setting Room temperature Handled by many sonographers and other technicians Patient contact G. ERGONOMICS: Device should reduce the levels of pinching and pushing forces that sonographers must apply currently Device should allow the sonographer to be able to easily use the console while manipulating the probe The maximum force applied by the sonographer should be no more than 200N. H. SIZE: Device should not be too big to hinder the sonographer Device should be easily stored and transportable in a hospital setting. Device should be adaptable to different sized transducers. Size of device should be adjustable for a variety of people to use and on patients of different sizes. I. WEIGHT: The weight of the device should be supported by the hospital bed. Device must not be too heavy to impede device translocation. J. MATERIALS: Heavy-duty plastics or metals should be used for the mechanical arm design. Materials must be able to withstand force the sonographer applies. Materials should not pose any risk to patient or sonographer. K. AESTHETICS, APPEARANCE, AND FINISH: 25 Transducer should be comfortable for the sonographers to grip. The form should conform to the hand, wrist, and/or arm as much as possible The finish should be non-irritating to the skin Device should have a smooth, sleek appearance which conforms to the standard hospital environment. The appearance should not be overwhelming for the patient. 2. PRODUCTION CHARACTERISTICS A. QUANTITY: One functional prototype at the minimum, One per echocardiogram bed if prototype is successful. B. TARGET PRODUCT COST: The cost to produce the mechanical arm design model will be ~ $75. o Aluminum arc: $33 o Actual arc that we used: $2.99 o Joints: $30 o Slider: $0 o Arm segments: $5 o Other accessories: $10 The cost to produce mechanical arm design prototype will be ~ $205. o Arc and arm segments: ~$75 o Joints: ~$30 o Slider: ~$30 o Pins and other accessories: ~$30 o Outside Labor: ~$40 The cost to the public and industry will be comparable to the current design. 3. MISCELLANEOUS A. STANDARDS AND SPECIFICATIONS: FDA approval is required. B. CUSTOMER: Many different sized patients with different amounts of adipose tissue. Private practices would like to use their staff as efficiently as possible; if possible, they would like to eliminate the role of the sonographer. C. PATIENT-RELATED CONCERNS: Sterilization may be necessary depending on the invasiveness of the procedure. Device needs to avoid making the patient uncomfortable or nervous. Device should not cause pain or irritation due to reaction to the materials used to construct the device. 26 D. COMPETITION: The following improvements have been made to the ultrasound devices: a more lightweight transducer probe, grooves in the transducer, a lightweight cable attachment, and adjustable chairs and consoles Many manufacturers are currently working on possible handle redesigns. The mechanical arm design is a novel idea. 27 Appendix B – Costs Materials Steel welding bar (1/4 X 1/8 X 72 in.) Compression springs PVC Piping ($0.67/ft.) bolts nuts Ball joint Hinge joint Plastic cup wood Wire, misc. Aluminum bar TOTAL (rounded): $75 Quantity cost 1 3 2 ft. $2.99 $2.25 $1.34 5 $0.50 5 1 1 2 $0.25 $20.84 $9.31 $0.25 n/a $0.00 n/a $0.00 1 $33 Future Costs of the Final Design Arc and arm segments: ~$75 Joints: ~$30 Slider: ~$30 Pins and other accessories: ~$30 Outside Labor: ~$40 TOTAL (approximate): $205 28