SBAR - Austin Community College
advertisement

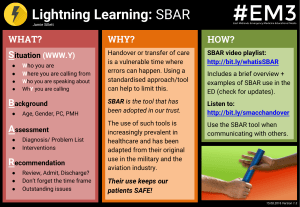
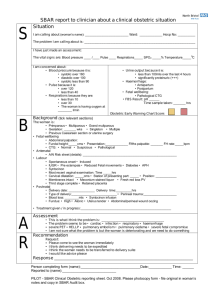
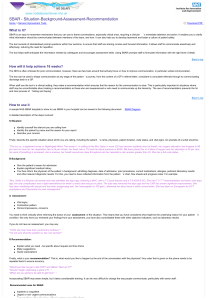
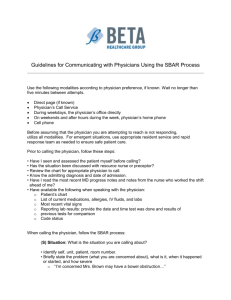
SBAR - A Communication Technique for Today's Healthcare Professional Situation, Background Assessment, Recommendation SBAR is a standardized way of communicating with other healthcare givers. It promotes patient safety because it helps physicians and nurses communicate with each other. Staff and physicians can use SBAR to share what information is important about a patient. It improves efficiency because this standardized form of communication helps caregivers speak about patients in a concise and complete way. SBAR is an acronym that stands for: Situation Background Assessment Recommendation Standardize Communication among Staff and Caregivers SBAR offers hospitals and care facilities a solution to bridge the gap in hand-off communication through a standardized approach to patient reporting at shift changes and during patient transfers. Using SBAR, patient reports are more accurate, efficient, and consistent enterprise-wide. This simple, yet highly effective communication technique can be used when: A nurse is calling a physician Nurses are handing off patients to one another Nurses are transferring patients to other facilities or to other levels of care Why is SBAR recommended for calls to physicians? SBAR promotes better communication. In most cases nurses and physicians communicate in very different ways. Nurses are taught to report in narrative form, providing all details known about the patient. Physicians are taught to communicate in using brief “bullet points” that provide key information to the listener. Here is an example of a call to a physician using SBAR: Dr. Jones, this is Deb McDonald RN, I am calling from ABC Hospital about your patient Jane Smith. Situation: Here's the situation: Mrs. Smith is having increasing dyspnea and is complaining of chest pain. Background: The supporting background information is that she had a total knee replacement two days ago. About two hours ago she began complaining of chest pain. Her pulse is 120 and her blood pressure is 128/54. She is restless and short of breath. Assessment: My assessment of the situation is that she may be having a cardiac event or a pulmonary embolism. Recommendation: I recommend that you see her immediately and that we start her on 02 stat. Why implement SBAR in your organization? The safe and effective care of patients depends on consistent, flawless communication between caregivers. Hand-offs or the process of passing on specific information about patients from one caregiver team to another, is an area where the breakdown of communication between caregivers often leads to episodes of avoidable harm to a patient. The Joint Commission on Accreditation of Hospitals has added to Goal 2 in the 2007 Patient Safety Goals. The additional statement (2e) reads, “Implement a standardized approach to “hand off” communications, including an opportunity to ask and respond to questions.” SBAR Tool for Calling a Physician BEFORE Calling the physician: • Assess the patient. • Review the chart for the appropriate physician to call. • Have chart in hand. Read the most recent physician and nursing notes. • Have all lab results available — either in print or be logged into Meditech Every SBAR report is different. Focus on the problem. Be concise. Not everything in the outline below needs to be reported — just what is needed for the situation. Check all that apply. ___Code Status: ___________ ___ Allergies:_____________ ___ IV Fluids: ______________ S Situation Your Name __________ Patient Name I am concerned about B Background The patient is in the hospital because ________________________________ Significant Vital Signs are _________ Significant Labs:___________________________________________________ Significant Test Results:_____________________________________________ The patient if complaining of_________________________________________ The patient’s physical assessment demonstrates ________________________ _________________________________________________________________ This is a change from _______________________________________________ The following interventions have been tried: ___________________________ _________________________________________________________________ A Assessment My assessment of the situation is _____________________________________ _________________________________________________________________ might be happening. Tell the physician if the problem is severe and may be life threatening. R Recommendation/Request I think the following needs to be done: Medication ___________________________ Tests ___________________________ Physician needs to come now and assess the patient. ___________________________ Transfer to ICU ___________________________ Do you want me to call you back for any reasons? ______________________________________________________ What would you like me to do if the patient does not improve? Unit Room # ___________________________ Shift Report Using SBAR Format Situation: Patient Name .Room Number .Admission Date .Physician(s) Background: Admission Diagnosis (date of surgery) Past medical history that is significant (hypertension, CHF, etc) . Allergies Code Status (any advance directives, DNR orders,) . Procedures done in previous 24 hours including results/outcomes (include where we stand with post procedure vitals/assessment) Assessment: Biophysical assessment (abnormals) . Abnormal vital signs . Dressing condition (changes) NG/Drain output IV fluids/drips/site; when is site to be changed . Current pain score-what has been done to manage pain . Rhythm (if on telemetry) Recommendations: Do we need a change in the plan of care? . What are you concerned about? What are you uncomfortable with? . Discharge planning . Pending labs/x-rays, etc We need to request a change in _________ (diet, activity, medications) . We need to request a consult with PT/ST/OT, dietician, diabetes nurse, social worker, wound care nurse, etc) We need to contact Dr. __________about___________