Improve Outcomes through Effective Communication Effective
advertisement
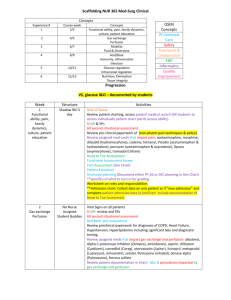
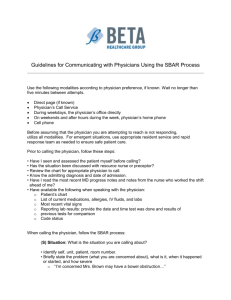
8/20/2013 Improve Outcomes through Effective Communication M Mary Narayan, N MSN, RN, HHCNS-BC, COS-C Home Health Clinical Nurse Specialist Narayan Associates mary.narayan@cox.net Objectives 1 Discuss issues & barriers to effective 1. communication between home health clinicians & physicians. 2. Describe how to prepare for & follow-through on SBAR communication. communication 3. Apply SBAR communication to specific home health situations. 1 8/20/2013 Joint Commission reports…. . Almost 70% of sentinel events related to communication problems. Ineffective Inadequate Untimely Happens in home care too And Ï hospitalizations And Ð outcomes “ What we have here is a failure to communicate.” Cool Hand Luke, 1967 2 8/20/2013 Research in Nurse-Physician Communication Training in communication methods differs Nurses: Narrative, timed sequence, descriptive Physicians: Concise bullet-point summaries When nurses call, doctors want to know: What is the problem? p What do you need me to do? By when do I need to respond? Nurses lose physician’s attention and their credibility if they can’t get to the point in first 10 seconds. Research in Nurse-Physician Communication Physicians Ph i i & nurses both b th learned l d that th t doctor d t is i “in “i charge” h ” BUT hierarchical communication is not effective in complex situations Healthcare is complex Culture/gender/pecking order are barriers to effective communication Nurses are less likely to communicate if they feel psychologically unsafe. “If I speak up….” Will I be subject to anger or ridicule. Will it be worth it? Will it make a difference? 3 8/20/2013 Came out of military operations and aviation industry 4 8/20/2013 Solution = SBAR Communication Situational Briefing Model Practical structure for communicating critical information concisely. Relevant, timely, important data communicated succinctly. SBAR Communication Situation. The problem. “Punch” Background. The context. Assessment. Analysis of situation. Recommendation. The fix. 9 Subordinates to Commanders : Averting Disaster Nuclear Submarine Sailor to captain S: Emergency! B: Ship above position A: Our p Their position Crash imminent! R: Go down! Not up! S: B: A: R: Airplane Co-pilot to pilot Emergency! In path of other plane! Crash imminent Pull up; turn left! 5 8/20/2013 Evolution of SBAR Leonard Graham Leonard, Graham, Bonacum–Kaiser Bonacum Kaiser Permanente (2004) Institute for Healthcare Improvement (2006) Home Health Quality Initiative (2007) Joint Commission’s National Patient Safety Goals (2008) Evidence in Home Healthcare Kogan, Underwood, Kogan Underwood Desmond Desmond, Hayes & Lucien (2010) (2010), Physician communication in managing community-dwelling older adults. Home Healthcare Nurse, 28(2):105-114. Evdokimoff, M. (2011). One home health agency’s quality improvement project to decrease rehospitalization. Home Healthcare Nurse Nurse, 29(3), (3) 180 – 193. 193 AHRQ (2012): Outcomes: Ï Effective communication Ï Patient outcomes Ï Collaboration Ï Patient satisfaction 6 8/20/2013 The SBAR about SBAR Situation: Inadequate communication in health care Î Ð quality of care, Ï hospitalizations and Ï costs Background: Nurses and physicians communicate differently Hierarchy -> lack of assertive communication Lack of Structure -> > missed information Assessment: Need for one effective communication method for all clinicians Recommendation: SBAR communication SBAR Communication Situation •Capture attention • Clinical problem • • • Background •Context • • Assessment •Current status •Analysis Recommendation •Action • statement needed •Timeframe I am … from… agency Patient name Problem is… Age, Diagnoses Recent relevant medical hx Current relevant assessment data • I think the patient has…. • I think the pt needs… Do you want me to… • 7 8/20/2013 If Patient Has a “Situation” Symptoms Signs What patient reports What you see, hear, palpate, measure New problem Exacerbation Zone Tools Yellow = “Situation” Clinical Judgment Critical Thinking HHQI Fundamentals of Reducing Acute Care Hospitalizations BPIP 8 8/20/2013 Before calling physician… 1. 2. 3. 4. Critical thinking Clinical judgment In-depth data gathering What does MD need to know? Assess the patient Determine urgency Review Medical Record Organize data Before calling physician, 1) Assess the patient Symptom & physical assessment Focus in on diagnosis & S/S with a “focused comprehensive assessment” of system(s) involved 9 8/20/2013 Body Systems Cardiovascular Respiratory Neurological Gastrointestinal Genitourinary Musculoskeletal Integumentary Endocrine Immunologic Which system(s) is/are involved? What assessment techniques can you use? What data will the doctor want to know? Before calling physician, 2) Determine urgency How quickly must I communicate? What is the severity/urgency? What is the risk for hospitalization? Routine R ti – Within Withi business b i hours h Urgent – Within 6 to 12 hours Emergent – Within 1 to 2 hours 10 8/20/2013 Before calling physician, 3) Review Medical Record Age & Diagnoses Reason for home care Recent assessments Recent change in POC Lab results Medications Allergies Pharmacy number Advanced Directives Before calling physician, 4) Organize data Organize data Primary & secondary data SBAR format What do you need physician to do? Required: Critical thinking Clinical judgment 11 8/20/2013 Clinician Call to Physician Try to make it 60 seconds or less! Situation 10 seconds Background 20 seconds Assessment 20 seconds Recommendation 10 seconds Situation Your name name, discipline discipline, agency Patient’s name Patient’s problem Concise statement Reason for concern Sign/symptom & severity 12 8/20/2013 Background Age g Relevant diagnoses Relevant recent events Hospital discharge Surgical procedures New medication started Other relevant history Advanced directives No caregiver in the home Assessment - Data Physical assessment data pertinent to problem Clinical judgment and critical thinking required Primary not secondary data Not whole assessment Omit the normal… “Rest of assessment normal.” 13 8/20/2013 Assessment – “Diagnosis” Wh t iis your analysis What l i off the th problem? bl ? How severe & urgent is the problem? Hints It “might be…” “I think it could be…” If no clue, what body system seems involved? Recommendation What do y you want to happen and by when? What action is needed? What option(s) do you recommend? By when is action needed? Hints: Focus on goal & team approach: “To prevent avoidable hospitalization, do you think we should try….” “Would you recommend….”; “Should we consider...”: “I think… might work…” 14 8/20/2013 SBAR Communication about Exacerbation of COPD Symptoms Situation: • Dr. (name), this is (your name, discipline) from (name of your home health agency). • I am calling about (patient’s name), who is experiencing increased dyspnea. SBAR for COPD Exacerbation Background: • Patient’s age ______ • Primary diagnoses: COPD ( GOLD stage, if known: A‐Mild, B‐Moderate, C‐Severe, D‐Very Severe); other primary/pertinent diagnoses • Recent important events. Examples include: o Admitted to home care on (date) for (reason for home care) o Discharged from the hospital on (date) after being treated for ___________. • Oxygen use: _________ liters/minute, intermittent or continuous • Current respiratory medications, and frequency of use; recent increased frequency • DNR status if applicable pp • Have available: Medication Profile, allergies and phone number of pharmacy Assessment: (Only report primary/abnormal/pertinent data) • Patient’s current symptoms: Dyspnea: Severity on Berg Scale: 1 – 2 – 3 – 4 – 5 – 6 – 7 – 8 – 9 – 10 Intermittent Constant Cough: Increased frequency Increased sputum Increased purulence description Fatigue Restlessness Anorexia Difficulty sleeping Vomiting Anxious When did symptoms develop? __________ How severe are symptoms? ______________ • Physical assessment: Vital signs: Temp ________ Pulse _________ RR ________ BP __________ SaO2 _________ Mental status changes: LOC _________________ Confusion Anxiety Skin color: Cyanosis Location: ______________________ Capillary refill _________________ Breathing effort: Tripod positioning Pursed lip breathing Retractions Nasal flaring Sputum: Color: _______________ Consistency: ________________ Amount _______________ Lung sounds: Crackles Wheeze Diminished Location: ________________________ Peripheral edema: 1+ 2+ 3+ 4+ • Analysis Examples Analysis Examples I believe the patient has developed a respiratory tract infection. The patient’s COPD symptoms may have exacerbated because of today’s air quality alert. The patient’s COPD seems to have exacerbated but there are no signs of respiratory infection. Recommendation: “We may be able to avoid hospitalization…” “We may be able to catch this early…” Antibiotic: Indicated for increase in dyspnea/sputum volume/sputum purulence Systemic corticosteroid: Prednisolone, oral, 30‐40 mg, daily for 10‐14 days. Short‐acting bronchodilators: change route to via nebulizer change frequency to every 4 hours change/add beta‐agonist or anticholinergic to Home oxygen therapy: Titrate to liters/minute to reach oxygen saturation of _______ (88‐92%) Increase visit frequency to ___________ (every day x 2‐3 days) to monitor treatment plan effectiveness. Additional Interventions: No exposure to smoke/air pollution Institute coughing/deep breathing/postural drainage. Force fluids to (2 to 2 ½ quarts). Teach relaxation and energy conservation techniques SBAR Communication about Exacerbation of Heart Failure SBAR about Heart Failure Exacerbation Situation: • Dr. (name), this is (your name, discipline) from (name of your home health agency). • I am calling about (patient’s name), who is showing signs of fluid overload. Background: (Review medical record, Medication Profile, last visit notes, labs, etc.) • Patient’s age ______ • Primary diagnoses: Stage __ (if known) heart failure; other primary/pertinent diagnoses (if any) • Recent important events. Examples include: o Admitted to home care on (date) for (reason for home care) o Discharged from the hospital on (date) after being treated for (reason for hospitalization) o Non‐adherence to medication therapy or low‐sodium diet due to confusion and no caregiver. o Patient has been hospitalized for HF 3 times in past 2 months. • DNR status if applicable DNR if li bl Assessment: (Only report primary/abnormal/pertinent data) • Patient’s current symptoms: SOB DOE Orthopnea Confusion Fatigue Other pertinent symptoms ____________________________________________________ When did symptoms develop? __________ How severe are symptoms? ______________ • Physical assessment: Vital signs: Pulse ____ RR _____ BP _________ O2 sat _____ Current weight _______ Weight gain _____ lbs in ______ days. Extra heart sounds (S3, S4) Lung sounds: Crackles (rales) Location: _____________________________________ Jugular vein distension Peripheral edema: 1+ 2+ 3+ 4+ Abdominal girth ______ in/cm which is an increase of _______ in/cm since ___________ Urine color/output: _____________________________________________ • Patient’s diuretic medication(s): __________________ [Loop diuretics (e.g. Lasix) preferred for HF] • Have available: Medication Profile, allergies and phone number of pharmacy • Analysis: Examples include: I believe patient is having an exacerbation of heart failure. Patient states he won’t go back to hospital and he wants to be treated at home or die. Patient’s fluid overload seems to be related to non‐adherence due to forgetfulness and confusion. Recommendation: Examples include: • To avoid rehospitalization, should the diuretic be increased to try to resolve the problem? • Would you like to order oral (or IV push) Lasix to see if we can avoid a hospitalization? • Should I follow up diuretic therapy with labs in a couple of days? Electrolytes? BUN? Creatinine? • Could I have orders for a dietician referral to review the low sodium diet? • Could we refer to MSW to assist family determine caregiving options related to diet and med administration needs? • Since patient has end‐stage HF and patient does not want to go back to hospital, could we have orders for a DNR and refer to palliative/hospice care? 15 8/20/2013 Physician Responds Appropriately Repeat orders Call back when/under what circumstances? Inappropriately -> C.U.S.S. I am concerned… d I am uncomfortable… The safety (of my patient) is at risk… Stop and listen to me… We have a problem. Other Barriers & Bulldozers Know doctor doctor’ss preference: best number number, time time, way Fax Office nurse Leave message: Secure e-mail Give time frame & reachable number Develop relationship with office staff Policy/procedure on elevating issue to next level If MD rude, be professional, remind yourself: it’s not you. 16 8/20/2013 When Else to Think “SBAR” “Transitions” Transitions & “handoffs” handoffs Coordination of Care Referral to homecare Transfer to hospital Discharge to physician Report to team members Teach the patient/caregiver SBAR Communication… Evidence-based Evidence based communication strategy Structured method for clearly communicating key information comprehensively yet concisely Empowers clinicians to provide input and make recommendations Encourages inter-professional dialogue about assessment and recommendations Enhances safety & quality of care 17 8/20/2013 References & Resources Arizona Hospital and Healthcare Association. (2007). SBAR Communication Standardization Toolkit. Phoenix: Author. Beckett, C. & Kipnis, G. (2009). Collaborative communication: Integrating SBAR to improve quality/patient safety. outcomes. Journal of Healthcare Quality, 31(5), 19-28. Collaboration for Homecare Advances in Management & Practice (CHAMP, n.d.) http://www.champ-program.org/ static/Review SBAR pdf static/Review_SBAR.pdf Home Health Quality Initiative (2007) SBAR: A Home Health Package Haig, K. M., Sutton, S., & Whittington, J. (2006). SBAR: A shared mental model for improving communication between clinicians. Journal on Quality and Patient Safety, 32(3), 167-175. References & Resources Kogan, g , et al. (2010). ( ) Performance Improvement p in Managed g Long-Term g Care: Physician Communication in managing community-dwelling older adults. Home Healthcare Nurse, 28(2):105-114. Leonard, et al. (2006). Using SBAR to improve communication between care providers. Institute for Healthcare Improvement. http://www.njha.com/qualityinstitute/pdf/630200633410PM63.pdf Narayan, M. (2013). Using SBAR Communications in Efforts to Prevent R h Rehospitalizations. it li ti H Home H Healthcare lth N Nurse, 31(9). 9) Maison, D. (2006). Effective communications are more important than ever: A physician’s perspective. Home Healthcare Nurse, 24(3), 172-178. Riesenberg, L. Leitzsch, J. , Cunningham, J. (2010). Nursing handoffs: A systematic review. AJN, 110(4), 24-34. 18 8/20/2013 References & Resources VNAA (2012) Procedure 23:03 Clinical Procedure Manual 19