CAPD PERITONITIS
advertisement

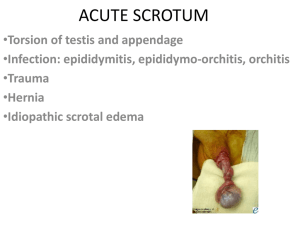
CAPD peritonitis Renal colic Scrotal pain CAPD PERITONITIS DIAGNOSIS Clinical Cloudy dialysate effluent + abdominal pain + fever Microbiological Send bag for: urgent gram stain WCC and differential - WCC >100 x 106/L + > 50% PMN’s fungal and bacterial culture and sensitivity If WCC less than this discuss with Renal Medical staff Differential Diagnosis Other causes of peritonitis TREATMENT Contact the PDU or renal nurse on 8B to make up PD bag Tell them: Therapy required Usual bag and dwell time Therapy A No previous MRSA colonisation / infection No allergy to penicillin or cephalosporin Cephazolin 1.5g intraperitoneal + Gentamicin 0.6mg/kg intraperitoneal (rounded to nearest 10mg and not greater than 60mg) Added to same bag to dwelled for a minimum of 6 hours + Cephradine 250mg PO QID (before each bag exchange) If unable to tolerate oral cephradine will need to continue cephazolin 125mg/L in each bag exchange and daily gentamicin Therapy B Previous MRSA colonisation / infection Penicillin or cephalosporin allergy Vancomycin 30mg/kg intraperitoneal rounded to nearest 500mg (not greater than 3g) + Gentamicin 0.6mg/kg intraperitoneal rounded to nearest 10mg (no greater than 60mg) Added to same bag to dwell for a minimum of 6 hours Patients on intraperitoneal insulin should have their intraperitoneal doses changed to SC (usually half the intraperitoneal dose) for the dose due with any antibiotics. DISPOSITION Admit if too unwell Arrange review the following day – in PDU, Monday to Friday or Renal Ward on the weekend. Further treatment will be per the Peritonitis Standing Order. RENAL COLIC DIFFERENTIAL DIAGNOSIS Must be excluded in anyone with suspected renal colic, especially the elderly. Aortic and iliac aneurysms Pyelonephritis Peritonitis, including appendicitis and diverticulitis Biliary colic Renovascular compromise, including renal artery or vein thrombosis Cancer esp renal Endometriosis Ovarian torsion INVESTIGATIONS MSU sent for microscopy and culture. Haematuria is present 85% of the time. !5 % of patients with renal colic will not have haematuria. If there are white cells or bacteria in the urine, consider infected stone. FBC if there is a high fever T > 38 deg C with or without significant renal tenderness, infection maybe present. The WCC is often raised even when there is no infection therefore is not indicated in uncomplicated renal colic. UREA / ELECTROLYTES & CREATININE is done in the elderly, impaired renal function, diabetes, and in those who are hypovolaemic. The young and previously healthy do not need renal function tests. MANAGEMENT Analgesia Morphine as per protocol for significant pain Metoclopromide 10mg IV for nausea and vomiting. Diclofenac sodium (voltaren) orally or rectally for moderate pain or with morphine for severe pain Intravenous fluids. Hydrate intravenously with 0.9 % saline. Antibiotics: Gentamicin 5 – 7mg/kg IV if co-existing urosepis is suspected. FURTHER INVESTIGATION In the young healthy patient in whom the diagnosis of renal colic is clinically not in question, and the pain has completely settled and there is no suspicion of any complication there is no need to obtain an immediate IVU. If pain is severe and ongoing , if the diagnosis is in doubt, if another condition is suspected, or if the patient is elderly, some diagnostic imaging is essential. Noncontrast helical CT Becoming the first line of imaging. Discuss with the radiologist on duty. Advantages Sensitivity 95 -97 % in detection of renal stones Specificity 96-98 % in detection of renal stones Faster than IVU Avoids intravenous contrast Limitations : Will diagnose other conditions such as AAA and GIT disease but is not as sensitive or as specific as CT with contrast Intravenous Urogram Comparable to CT in sensitivity and specificity for stones, but also shows renal function. Takes too long and exposes patient to contrast. Contraindications Serum creatinine > 0.2 History of adverse (allergic) reaction to contrast. Contrast can be nephrotoxic in the following conditions Preexisting renal insufficiency Diabetics Dehydrated patients Hypotension Age> 60 Multiple myeloma Hypertension Hyperuricemia Use of diuretics for cardiovascular system History of IV radiocontrast media within 72 hours Ultrasound When IVU or CT is contraindicated, or when there is no haematuria. Will detect larger > 5 mm stones , particularly in the proximal and distal ureter but only poorly visualizes midureteric stones. Very sensitive for hydronephrosis (98%) but 22 % of hydronephroses detected on ultrasound do not represent obstruction. Advantages: noninvasive, no contrast, no radiation, no side effects. Can give clues to other pathology, such as AAA. Obesity may reduce accuracy. Plain X-ray KUB Limited use, but required by radiology prior to CT. 90 % of renal stones are radio-opaque but the sensitivity is only up to 22 to 58 % and the specificity 69 to 74 %. Negative predictive value is only 23 %. In patients in whom the diagnosis is already established, plain Xray is useful in following the passage of a radioopaque stone. DISPOSITION OF PATIENT Admit 1. Fever > 38 degrees, or septic as may require a nephrostomy. 2. Severe ongoing pain that does not settle with IV narcotic and NSAIDS. 3. Recurrent attacks of colic with repeated visits to the emergency department. 4. 5. 6. Ureteric stone more than 6 mm in diameter. These are unlikely to pass. Any stone in a solitary kidney. Creatinine > 0.2 Discharge Everyone else. Send a referral to the urology outpatients clinic. The patient will be seen in 4 weeks with an updated KUB film unless the stone is radiolucent when a limited IVU will be done. Advice patient to strain urine. Give the patient a script for voltaren unless there is a contraindication to the drug. The patient should return promptly if they develop a fever. BEWARE DRUG SEEKERS SCROTAL PAIN COMMONEST CAUSES 1. Torsion of testicular appendage 2. Epididymitis 3. Testicular torsion Testicular torsion occurs in less than 1/3 of the cases but is the presumptive diagnosis until proven otherwise. Testicular function unlikely to be recoverable after 12 hours. HISTORY Take a good history. There are no pathognomonic distinguishing features and presentations may be misleading. Testicular Torsion Testicular Appendage Torsion Epididymitis Age First few days, 13 – 15 Previous similar episodes with pain free episodes Strongly suggestive or intermittent or recurrent torsion Usually severe 30 – 80% Sudden onset Usually within 6 hours Often nocturnal 10 – 20% No Younger – STD Older – UTI organisms Not self resolving Rare Often a few days Rare Often later >24 hours Insidious onset No No 50% Pain Nausea, vomiting, anorexia Time of presentation History of trauma or physical exertion Dysuria, frequency or urethral discharge THOROUGH PHYSICAL EXAMINATION Generally the patient with torsion of the testis will appear uncomfortable whereas the patient with appendicular torsion and epididymitis will appear relatively comfortable. Examine the parotids for mumps. Local inspection should rule out a hernia. The penis is inspected for discharge. Inspect the scrotum for swelling, redness and tenderness. Swelling to the entire scrotum is common to all three conditions. With torsion swelling comes on typically later, usually after 12 hours. Try and elicit the cremasteric reflex. If present testicular torsion is very unlikely. Examine the testis for abnormal elevation and lie. Palpate the testis for tenderness Transilluminate for hydrocoele Abdomen for pathology causing referred pain Testicular torsion is suggested by 1. 2. 3. 4. An abnormal elevation (high-riding testis) with a palpable twist in the spermatic cord. Abnormal axis with the patient standing up. Abnormal position of the epididymis within the scrotum. An abnormal axis in the contralateral testis. Horizontal lie -- bell clapper deformity. Or the epididymis is palpated at the inferior pole. Torsion of a testicular appendage 1. 2. Palpable 3 to 5 mm tender nodule or mass in the groove between the testis and the epididymis. The blue dot sign - where a blue dot is present in the superior portion of the scrotum through stretched scrotal skin, is not as common. Epididymitis Superior pole is tender. 10 % of cases of torsion will initially present with tenderness in a similar position. Scrotal elevation to relieve pain is unreliable as a differentiating feature from torsion of the testis. DIFFERENTIAL DIAGNOSIS Emergencies Torsion of the testis Traumatic testicular rupture Fournier's gangrene Peritonitis with patent processus vaginalis Abdominal aortic aneurysm Non-emergencies Torsion of appendix testis or epididymis Acute epididymo-orchitis Idiopathic scrotal oedema Traumatic haematoma Scrotal abscess Acute haemorrhage into testicular neoplasm Renal colic Hydrocoele Varicocoele Henoch-Schonlein Purpura Insect bite INVESTIGATIONS Urinalysis: Pyuria is defined as greater than or equal to 10 WBC/HPF About 50 % of patients with epididymitis will have pyuria but its absence does not confirm epididymitis or nor does its presence rule out torsion. Urethral swab: Gram stain, chlamydia immunofluorescence, N gonorrhoea culture. Serum WBC count is not useful on its own, as it is raised in 30 to 50 % of patients with either condition, epididymitis or testicular torsion. Colour Doppler Ultrasonography: Can differentiate between epididymitis and torsion by patterns of blood flow. Can detect and differentiate between testicular haematoma and rupture. Indications Unclear clinical picture. But do not wait for ultrasound if this is going to be delayed; obtain an urgent urological consultation while waiting. MANAGEMENT 1. Suspected torsion of testis Analgesia Refer to the urology registrar. Obtain an urgent ultrasound. 2. Epididymo-orchitis The aetiology depends on age. In the young male it is most commonly an STD, the organisms being Chlamydia, Neisseria gonorrhoea and Ureaplasma urealyticum. In the older male it is most commonly a gram negative rod, such as E.coli and Klebsiella and rarely Pseudomonas. Patient febrile and toxic: admit for IV antibiotics and studies to rule out abscess. Patient non toxic: Discharge on antibiotics, bed rest, scrotal elevation with folded towel, ice for 10 minutes 3 to 4 times a day and advise to ambulate when pain free. Prescribe NSAID and paracetamol Antibiotics Suspected STD: Appropriate swabs Ciprofloxacin 500 mg po stat only (alternatively ceftriaxone 250 mg im stat only), followed by Doxycycline 100mg bd for 10 days (alternatively erythromycin ) STD not suspected: IV gentamycin 5 7mg/kg daily or Trimethoprim 300mg daily 10 days or Nitrofurantoin 50mg QD for 10 days At discharge refer all patients to their general practitioner for follow up. If concerned refer to urology clinic 3. Torsion of testicular appendage Bed rest, NSAIDS, analgesia, and ice. The affected appendage will necrose in 14 days and become asymptomatic. Refer to urology clinic.