Evaluation of Scrotal Pain 1.4.11 Case Conference

Case Conference
Vincent Patrick Tiu Uy
PGY-1
January 4, 2011
General Data
17 year old male with scrotal pain
History of Present Illness
(+) Testicular pain, bilateral, with no radiation to the inguinal area, graded 3-4/10, more pronounced when standing, relieved by sitting
(+) Difficulty in walking
(-) Dysuria, penile discharge, hematuria
No medications taken
Denies history of trauma to the groin
No prior history of testicular pain
Consult to Emergency Department
History
Review of Systems
Unremarkable. Most mentioned in the HPI
Past Medical
History
Family History
Social History
Insomnia (?) taking Seroquel, no previous hospitalizations, no previous surgeries, NKDA
Denies any medical/surgical problems among immediate family members
Child lives in an apartment with parents and siblings. No pets at home. No recent travel.
Denies any introduction of new foods. Child feels safe at home. Admits to prior sexual activity with 1 female partner. Denies smoking, alcohol and illicit drug use.
Physical Examination
General Appearance Alert and awake, prefers to sit
Vital Signs
Head, Eyes, Ears, Nose Throat,
Neck
T 98 HR 102 RR 20 BP 122/79 SO2 98% RA
NCAT, pinkish conjunctivae, anicteric sclerae, nasal septum midline, TM’s intact, dry oral mucosa, nonhyperemic OP, supple neck, no CLAD
Chest and Cardiovascular
Abdominal Exam
GU/Rectal
Extremities
CTAB, +S1/S2, no murmurs
Flat abdomen, hypoactive bowel sounds, no tenderness, no palpable masses, (-) rebound, (-)
Rovsing’s sign, (-) Psoas sign, (-) Obturator sign, (-)
Murphy’s sign
Tanner V, no penile discharge nor erythema of the tip.
Uncircumcised. B/L descended testes. No obvious discoloration of the scrotum. (+) tenderness to palpation of both testes. No Phren’s sign, no blue dot sign and no “bag of worms”. Transillumination negative for fluid.
No edema, no cyanosis, brisk capillary refill
Differentials?
Management in the ED
STAT Scrotal Ultrasound
Urinalysis – normal
Urine sent for culture – normal
Urine GC/Chlamydia sent - negative
Scrotal Ultrasound
Scrotal Ultrasound
Scrotal Ultrasound
Scrotal Ultrasound
Impression/Disposition
Signed off as a case of Epididymitis + Small Varicocoele
Pain relief + Prophylactic antibiotics
Evaluation & Management of Children with Testicular Pain or Swelling
Anatomy of the Testis
Key Questions in the History
Characteristic of the pain Recurrent pain suggests torsion
History of trauma
History of change in the size of the testicle
Changes during Valsalva suggests communicating hydrocoele or varicocele
Sexual history
Difficulty voiding urine
STD’s can cause epididymitis
Suggests intraabdominal mass (hernia), UTI, neurologic problems or spinal cord disease
Flank pain or Hematuria Suggests kidney stone with referred pain to the scrotum
Suggests testicular torsion Abdominal pain with diminished appetite, nausea and vomiting
Focused Exam
Inspection
Palpation
Cremasteric Reflex
Phren’s sign
Blue dot sign
Inspection
Inspect while the patient is standing – check the penis, pubic hair and inguinal areas.
Inspect for ulcers, papules, pubic hair infestations or lymphadenopathy
Does the patient have any tattoo? Piercings?
Inspection
The left testicle is slighlty lower than the right
Palpation
Roll the testicle between thumb and forefingers to look for masses
Palpate for the epididymis and go up towards the spermatic cord.
Transilluminate the scrotum if swelling is suspected.
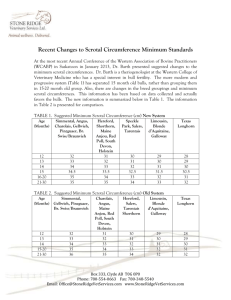
Predicting Testicular Size
Cremasteric Reflex
Stroking the upper thigh results in elevation of the ipsilateral testicle.
Usually present in boys
30 months to 12 years
Less reliable in teenagers and infants
Phren’s Sign
Elevation of the scrotal contents relieves pain in patients with epididymitis and not with testicular torsion.
POSITIVE SIGN – Relief of pain with elevation =
EPIDIDYMITIS
Not a reliable exam in most situations.
Blue Dot Sign
Almost always suggestive of torsion of the appendix testis.
Additional Tests
Test
Complete Blood Count
Urinalysis and Culture
Purpose
Elevated WBC count in torsion
Test usually obtained for pre-operative purposes
R/o UTI
Pyuria may be seen in Epididymitis
R/o sexually transmitted diseases Gram stain, culture, rapid molecular amplification testing of urethral discharge
-or-
Nucleic amplification test of urine
Color Doppler Ultrasound of the
Scrotum
Check perfusion
R/o torsion if cannot be excluded on clinical grounds
Differential Diagnosis
Testicular Torsion
Torsion of Appendix
Testis
Epididymitis/Orchitis
Trauma
Incarcerated Inguinal
Hernia
Henoch-Schoenlein
Purpura
Referred Pain
Non-specific
Differential Diagnosis
Hydrocoele
Varicocoele
Spermatocoele
Testicular Cancer
Torsion of the Testicle
Inadequate fixation of the testis to the tunica vaginalis through the gubernaculum
“Bell-clapper” deformity
Twisting of the spermatic cord
Venous compression and edema
Ischemia
Torsion of the Testicle
Peak incidence in the neonatal period and the pubertal period
~65% occur during the 12-18 year old range due to increasing weight of the testicles
Torsion of the Testicle
Abrupt onset of severe testicular or scrotal pain
<12 hours of duration
90% have associated nausea and vomiting
Pain can be constant unless the testicle is torsing and detorsing
Most boys report a previous episode in the past
Torsion of the Testicle
Diagnosis is made clinically. Impression is stronger if there are previous episodes
Doppler ultrasound should be done if there are uncertainty in diagnosis
False positive scans (diminished blood flow)
Large hydrocoeles
Abscess
Hematoma
Scrotal hernia
False negative scans
Spontaneous detorsion or Intermittent torsion-detorsion
Torsion of the Testicles
Timing of operation
4-6 hours (100%)
>12 hours (20%)
>24 hours (0%)
The contralateral testis should also be explored;
“bell-clapper deformity” is usually bilateral
Surgical Detorsion +
Orchiopexy
Orchiectomy if non-viable
Torsion of the Appendix
Testis/Epididymis
Pedunculated shapes of these structures predispose them to torsion
Occurs most commonly in 7-12 year old boys
Torsion of the Appendix
Testis/Epididymis
Pain is of sudden onset, similar to testicular torsion
The testicle is non-tender, but there is a tender localized mass usually at the superior or inferior pole
(+) Blue dot sign – gangrenous appendix
Doppler ultrasound may be necessary to rule out testicular torsion – will show a lesion of low echogenicity. Blood flow to the affected area may be increased
Radionuclide scan may show the “hot dog” sign of the torsed appendage.
Torsion of the Appendix
Testis/Epididymis
Management
Bed rest, Analgesia, Scrotal Support
Resolution
5-10 days out patient
No follow-up necessary
Surgery
Removal of the appendage; exploration of contralateral testis not necessary
Epididymitis
Inflammation of the epididymis
Occur more frequently in late adolescent boys and even in younger males who deny sexual activity.
Risk factors
Sexual activity
Heavy physical exertion
Direct trauma
Bacterial epididymitis – think of anatomical abnormalities
Epididymitis
(+) Sexual activity
Chlamydia
N. gonorrhea
E. coli
Viruses
Ureaplasma
Mycobacterium
CMV
Cryptococcus (HIV)
(-) Sexual Activity
Mycoplasma
Enteroviruses
Adenovirus
Epididymitis
Acute or subacute onset of testicular pain
History of urinary frequency, dysuria, and fever
Normal vertical lie on exam, scrotal erythema, (+) scrotal edema, inflammatory nodule
Normal cremasteric reflex, with negative Prehn’s sign
Epididymitis
Doppler ultrasound may be necessary to rule out testicular torsion
All patients should get a urinalysis and urine culture
CDC guidelines in sexually active boys
Gram-stained smear if urethral exudates or intrautheral swab specimen or Nucleic amplification test
Urine culture of a first void urine
RPR and HIV testing
Epididymitis
ADMSSION
CRITERIA
Doubt diagnosis
(?Torsion)
Severe pain
CHILDREN
(+) Leukocytes in urine
Empiric antibiotics –
Bactrim*/Keflex*
Immunocompromised (-) Leukocytes in urine
Unreliable patient
Supportive treatment
[NON-BACTERIAL]
Non-compliance
SEXUALLY ACTIVE
Ceftriaxone x 1 +
Doxycycline x 10 days
Ofloxacin
Levofloxacin
• It is equally important to treat sexual partners if an STD is the likely cause.
• Supportive therapy: Scrotal support, bed rest and NSAIDS
Other Causes & Clues
CAUSES
Trauma
CLUES & MANAGEMENT
• Rarely – compression of the testis against the pubic bone from straddle injury Testicular rupture
• Hematocoele Intratesticular hematoma
• Color doppler may diagnose the abnormality
• Audible bowel sounds in the scrotum Incarcerated Inguinal
Hernia
Henoch-Schonlein
Purpura
Orchitis
• Nonthrombocytopenic purpura, arthralgia, renal problems, abdominal pain, GI bleeding
• Treatment is supportive bleeding in the GIT is more priority in management
• Usually viral (Mumps, Rubella, Coxsackie,
Echovirus)
• Brucellosis
• Pain and tenderness of the testis with peculiar shininess of the scrotal surface
• Symptomatic treatment rest and ice packs,
NSAIDS
Other Causes & Clues
CAUSES
Referred Pain
Nonspecific Scrotal
Pain
CLUES & MANAGEMENT
• Other signs and symptoms may be apparent
• Examples include:
• Urolithiasis
• Nerve root impingement
• Retrocecal appendicitis
• Tumor
• Mild scrotal pain in the light of a normal exam
• Imaging is not necessary
• Treatment is not necessary
Scrotal Swelling
Scrotal Swelling History & PE
Hydrocele
Varicocele
Spermatocele
Testicular CA
• (+) Transillumination
• Increase in size during the day or with Valsalva
• If non-communicating, no change in size.
• The spermatic cord has a “bag of worms” feeling secondary to vessel dilation
• The varicoceles may be more palpable with standing or with Valsalva
• (-) Transilluminate
• Painless, fluid filled cyst on the head of the epididymis
• (+) Transillumination localized to the head of the testis
• Firm, painless mass that does not transilluminate
• (+) Reactive hydrocele
Brain Teaser
An 18 year old male was seen in the ED for scrotal pain of 1 day.
He denied previous episodes before. He recently recovered from a febrile
“infection” about a week ago.
Patient is sexually active with female partners. On exam, the testes were not enlarged, (+) tender to palpation B/L,
Prehn’s sign was negative, no blue dot sign noted. Urinalysis showed leukocyte esterase and nitrites with pyuria. The ED attending asks you : “What’s the plan?”
A. No additional test is needed – treat empirically with Ceftriaxone and
Doxycycline
B. Test for STD’s like
Chlamydia and Gonorrhea
C. Send the urine for culture and sensitivity
D. Scrotal ultrasound to immediately rule out torsion.
E. Admit the patient and annoy the floor team
Brain Cruncher
A 16 year old male was seen in the ED for acute onset of scrotal pain.
On further questioning, he has had prior episodes of scrotal pain which lasted for only 2 minutes on the average.
The astute ER attending got a urinalysis and scrotal ultrasound.
The final diagnosis was testicular torsion.
To alleviate the patient’s anxiety as to benefit of immediate surgery, what should the ED attending ask the patient at this point?
A. “Where exactly is the pain?”
B. “What is the quality of the pain?”
C. “Was there any trauma to the groin?”
D. “What time did the pain happen?”
E. “Did you take any pain reliever and did it help with the pain somehow?”