Acute Scrotal Pathology
Acute Scrotal Pathology
Henry Yao
Pre-SET Urology Trainee
Royal Melbourne Hospital
Case History
• You are working in ED at night
• It is 4am and you are tired + hungry
• As you are about to go to get a snack
• 12 year old male presents with 2 hour history of pain in right side of scrotum
Question
• What are your differential diagnoses?
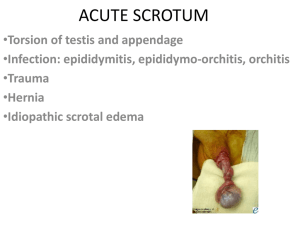
Differential diganoses
• Hydatid of Mortgagni (60%)
• Testicular Torsion (30%)
• Epididymo-orchitis (<5%)
• Idiopathic scrotal oedema (<5%)
Question
• What history questions would you ask?
Case History
• Scrotal pain came on over an hour
• Steadily getting worse
• Vomited once
• Some vague lower abdominal and back pain
• No trauma to testicles
• Two years ago had an STI rx with antibiotics
• Stable girlfriend for 12 months
Question
• What would you look for on examination?
Cresmateric Reflex
Testicular Torsion
• Intravaginal vs Extravaginal
Testis Anatomy
• Paired solid viscera
• Oval shaped
• Left lies slightly lower than right
• Epididymis posteriorly
• Vas deferens postero-medially
• Tunica albuginea covering
• Tunica vaginalis antero-laterally
• Appendix of testis located in upper pole
Testis Anatomy
• Arterial supply
– Testicular artery
• Venous drainage
– Pampiniform plexus
• Lymphatic supply
– Para-aortic nodes at origin of testicular artery (L2)
• Nervous supply
– T10 sympathetic supply (sensory follows this)
Presentation
• Most commonly age 12-18
• Acute onset of severe testicular pain +/- swelling
• On examination
– Tender firm testicle
– High riding testicle
– Horizontal lie of testicle
– Absent cremasteric reflex
– No pain relief with elevation of testis
– Thick or knotted spematic cord
– Epididymis not posterior to the testis
Diagnosis
• Clinical suspicion
– More likely when the onset of pain is acute and extremely intense
– C.f. epididymitis more likely when onset of pain is gradual and progresses from mild to more intense
– DO NOT WAIT FOR IMAGING if suspect torsion
Management
• IMMEDIATE SURGICAL EXPLORATION if suspected testicular torsion
• Most testicles remain viable if detorsed within
6 hours
• Few testicles remain viable after > 24 hours of torsion
Surgical Exploration
• Median raphe incision
• Cut through all layers to get to testis
• Detorse the testis
• Three point fixation to
Dartos
• Do the contralateral side
Imaging
• Doppler USS
– Torsion: decrease blood flow
– Epididymitis: increased blood flow
• Nuclear testicular scan
– Torsion: decrease uptake
– Epididymitis: increased uptake of radiotracer activity
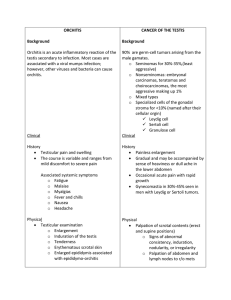
Hydatid of Mortgani
• Torsion of appendage
• Acute pain
• Blue dot in upper pole
• If in doubt explore
Epididymo-orchitis
• Rare in childhood
• Virtually never between 6 months and puberty
• LUTS
• Tender epididymis
• Prehn’s sign
• Dipstick and urine MCS
• Rest, antibiotics, high fluid intake, alkalinisation of urine
Idiopathic Scrotal Oedema
• Causes unknown: ?allergy, ?insect bites
• Scrotum symmetrically swollen, pink and less painful c.f. other causes
• Erythema spread beyond the scrotum
• Scrotal skin hard but testis and epididymis not painful
Case 2
• 36 year old male
• Day 2 post vasectomy
• Presents with painful scrotum
• What do you do?
Question
Case History
Case History
• Vital signs
– Tachycardia 110
– Blood pressure 100/60
• Very tender scrotum
• Hardened scrotal skin
• Spreading beyond scrotum
Question
• What do you think is going on?
Fournier’s Gangrene
• Necrotizing fascitiis of male genitalia and perineum
• 30% mortality
• Rapidly progressive
• Sources of bug from perianal region
• Most common bug is E. coli but must also consider GPC and anaerobes
Fournier’s Gangrene
• Risk factors
– T2DM
– Alcohol
– Other immunosuppressed patients
• Spread across superficial fascial planes
– Colles
– Scarpa
– Buck’s
Presentation
• Painful swelling and induration of the penis, scrotum or perineum
• Oedema spread beyond area of erythema
• Eschar, necrosis, ecchymosis, crepitus are later signs
• Foul odour
• Fever
• Diagnosis is clinical don’t wait for imaging
Management
• Broad spectrum IV antibiotics – consult VIDS
– Cover GP, GN and anaerobes
• Immediate aggressive tissue debridement cut down to normal tissue
• Send tissue for MCS
• May require flaps
• (Consider hyperbaric oxygen therapy)
TGA Antibiotics
Questions
Acknowledgement
• Dr. Kevin O’Connor (Urology Fellow)
Thank You for Your Attention