Chapter 16 - Cengage Learning
advertisement
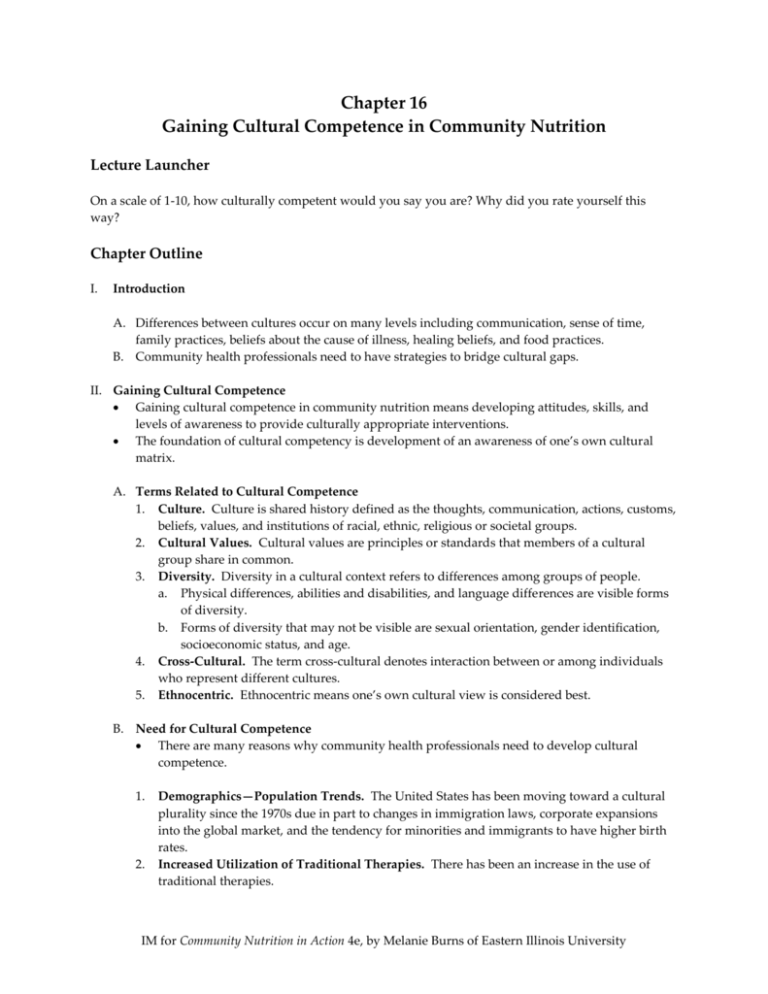
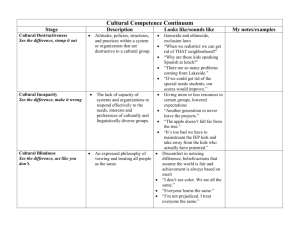
Chapter 16 Gaining Cultural Competence in Community Nutrition Lecture Launcher On a scale of 1-10, how culturally competent would you say you are? Why did you rate yourself this way? Chapter Outline I. Introduction A. Differences between cultures occur on many levels including communication, sense of time, family practices, beliefs about the cause of illness, healing beliefs, and food practices. B. Community health professionals need to have strategies to bridge cultural gaps. II. Gaining Cultural Competence Gaining cultural competence in community nutrition means developing attitudes, skills, and levels of awareness to provide culturally appropriate interventions. The foundation of cultural competency is development of an awareness of one’s own cultural matrix. A. Terms Related to Cultural Competence 1. Culture. Culture is shared history defined as the thoughts, communication, actions, customs, beliefs, values, and institutions of racial, ethnic, religious or societal groups. 2. Cultural Values. Cultural values are principles or standards that members of a cultural group share in common. 3. Diversity. Diversity in a cultural context refers to differences among groups of people. a. Physical differences, abilities and disabilities, and language differences are visible forms of diversity. b. Forms of diversity that may not be visible are sexual orientation, gender identification, socioeconomic status, and age. 4. Cross-Cultural. The term cross-cultural denotes interaction between or among individuals who represent different cultures. 5. Ethnocentric. Ethnocentric means one’s own cultural view is considered best. B. Need for Cultural Competence There are many reasons why community health professionals need to develop cultural competence. 1. 2. Demographics—Population Trends. The United States has been moving toward a cultural plurality since the 1970s due in part to changes in immigration laws, corporate expansions into the global market, and the tendency for minorities and immigrants to have higher birth rates. Increased Utilization of Traditional Therapies. There has been an increase in the use of traditional therapies. IM for Community Nutrition in Action 4e, by Melanie Burns of Eastern Illinois University a. 3. 4. 5. 6. Developing an understanding of the health practices of various cultures can help health practitioners develop and implement meaningful interventions. b. There has been a substantial increase in utilization of practices such as acupuncture, meditation, and ayurveda. Health Disparities Causes of Health Disparities. Health disparities exist between different ethnic groups for a variety of reasons. a. Socioeconomic status. Many minorities have lower socioeconomic status, and many are uninsured. b. Lack of insurance. Minorities are more likely than whites to be uninsured. c. Culture. Some cultural beliefs and health practices of minorities may contribute to health risks. d. Access to and utilization of quality health care services. Many minorities do not have access to and utilization of quality health care services. e. Discrimination/racism/stereotyping. Some minorities may experience discrimination or racism and experience psychological distress, substance use, and health problems as a result. f. Environment. Minorities are more likely to live in polluted environments and work in hazardous occupations. Under-Representation of Health Care Providers from Culturally and Linguistically Diverse Groups. Community nutrition professionals are frequently challenged to provide services for cultural groups they have never encountered; therefore, ideally, the health care workforce should be as diverse as the population it serves. Legislative, Regulatory, and Accreditation Mandates. Recognizing the need to develop cultural competency skills, many organizations and agencies have set educational standards and core curriculum guidelines for developing cultural competence and providing culturally competent services. C. Cultural Competence Models Two models have significance for community nutrition professionals. 1. 2. 3. 4. Cultural Competence Continuum Model. The Cultural Competence Continuum model structures the act of gaining cultural competence through a succession of stages. The Campinha-Bacote Cultural Competence Model a. The Campinha-Bacote Cultural Competency Model for Health Care Professionals views cultural competence as a process rather than an end result. b. Five interdependent constructs of this model include cultural awareness, cultural knowledge, cultural skills, cultural encounters, and cultural desire. Cultural Awareness a. Awareness of your own beliefs, values, and attitudes and an understanding that these are biased provides the foundation of cultural competence. b. Our worldviews, or how we believe the world should function, have been reinforced over our lifetimes and may lead to culture shock. Cultural Knowledge a. Valuing diversity and having the ability to view the world through multiple cultural lenses are the heart of cultural competence. IM for Community Nutrition in Action 4e, by Melanie Burns of Eastern Illinois University b. 5. There are many advantages of gaining knowledge and understanding of cultural groups, but you should always remember that characteristics of a group are simply generalities and you should try to avoid stereotyping. c. An understanding of generalities allows community nutritionists to develop relevant programming that builds on strengths and respects cultural differences. Cultural Encounters a. Areas to explore about cultural groups you encounter in your work include: 1. Socioeconomic and environmental factors. 2. Language and communication styles. 2. Cultural food practices. 3. Common health problems. 4. Health care values, beliefs, and practices. 5. Attitudes toward seeking help from health care providers. 6. Religious behaviors and beliefs. b. There are many different strategies for learning about different cultural practices including exploring the media, arranging cultural encounters, and walking or driving through communities. III. Cross-Cultural Communication A. Communication Styles 1. Barriers to Cross-Cultural Communication. Cross-cultural communication barriers include the nutritionist and client not speaking the same language, individuals using the same word but with different meanings, and not interpreting nonverbal behavior correctly. 2. Practical Guidelines for Cross-Cultural Communication. Many differences in communication styles occur among cultures but there are ways to enhance cross-cultural communication. a. Create a comfortable cross-cultural interaction by being friendly, attempting to learn and use key words, articulating clearly, and asking clients to identify their ethnicity. b. Suggestions for Communicating Information. Use a less direct approach for communicating information, use visual aids, ask the same question a different way, consider alternatives to written communications, and write numbers down. c. Ways in Which Discussions about Food Can Open Dialogue. Use discussions about food to open dialogue by asking about favorite foods and foods used for celebrations and telling food stories. B. Working with Interpreters. Community nutritionists should use professional interpreters or translators, as needed, rather than relying on friends or relatives of clients. IV. Culturally Appropriate Intervention Strategies The fundamental requirement for utilizing intervention strategies effectively is to have an inherent caring, appreciation, and respect for clients and be able to display warmth, empathy, and genuineness. A. Explanatory Models 1. Anthropologists have developed explanatory models as a culturally sensitive way to investigate a client’s perception of illness and they explore five major concerns about an illness episode: a. Etiology. IM for Community Nutrition in Action 4e, by Melanie Burns of Eastern Illinois University b. Time and mode of onset of symptoms. c. Pathophysiology. d. Course of sickness. e. Treatment. 2. Open-ended questions can be used in a respondent-driven interview approach to aid in understanding illness and food issues from a client’s perspective. B. LEARN Intervention Guidelines. LEARN guidelines provide a framework for negotiating a culturally sensitive treatment plan to address a given illness episode: 1. Listen. 2. Explain. 3. Acknowledge. 4. Recommend. 5. Negotiate. C. Practical Considerations for Interventions. Use practical considerations for planning interventions, taking into consideration the physical environment and resources, community participation, and special considerations for new immigrants. V. Organizational Cultural Competence Health care agencies must scrutinize all aspects of their organizational structure to infuse cultural competency at every level: Mission statements. Structures to assure consumer and community participation. Policies and procedures for recruitment, hiring, retention, and training. Fiscal resources for translation and interpretation services. A. Essential Organizational Elements of Cultural Competence. There are five essential elements necessary for an organization to provide culturally competent programming: 1. Valuing diversity. 2. Having the capacity for cultural self-assessment. 3. Being conscious of the dynamics inherent when cultures interact. 4. Having institutionalized cultural knowledge. 5. Adapting service delivery based on understanding of cultural diversity. B. Organizations can influence cultural competence of health care delivery at three levels of intervention: 1. At the macro level health care providers can develop culturally sensitive laws, policies, and regulations. 2. The mezzo level addresses the design and delivery of culturally appropriate and effective community programs. 3. Organizations function on the micro level by providing resources and training programs to help professionals develop and utilize cultural competence skills. IM for Community Nutrition in Action 4e, by Melanie Burns of Eastern Illinois University