Gram Staining Lab
advertisement

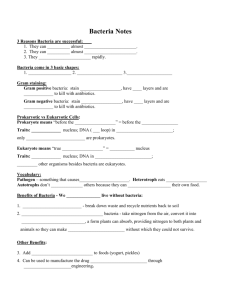
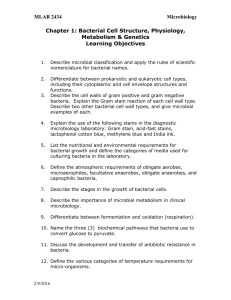
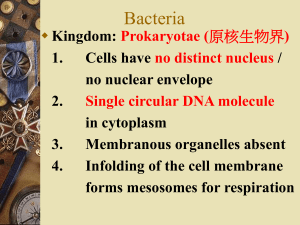
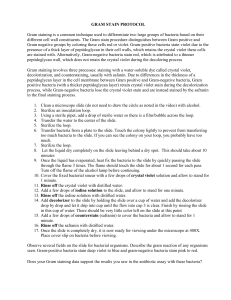
Gram Staining Lab Pre-Lab Document Background Information: Gram staining (or Gram's method) is a method of differentiating bacterial species into two large groups; Gram-Positive, and GramNegative. The chemical and physical properties of their cell walls are what determines their ability to become gram-stained using this method. The Gram stain is almost always the first step in the identification of a bacterial organism. While Gram staining is a valuable diagnostic tool in both clinical and research settings, not all bacteria can be definitively classified by this technique, thus forming Gram variable, and Gram indeterminate groups as well. Gram-positive bacteria are those that are stained dark blue or violet by Gram staining. This is in contrast to Gram-negative bacteria, which cannot retain the crystal violet stain, instead taking up the counterstain, which in this lab is safranin. Gram negative bacteria appear red or pink. Gram-positive organisms are able to retain the crystal violet stain because of the high amount of peptidoglycan in their cell wall. Gram-positive cell walls typically lack the outer membrane found in Gram-negative bacteria. Gram-negative bacteria are those bacteria that do not retain crystal violet dye in the Gram staining protocol.[1] In a Gram stain test, a counterstain is added (safranin) after the crystal violet, coloring all Gram-negative bacteria with a red or pink color. The test itself is useful in classifying two distinct types of bacteria based on the structural differences of their cell walls. On the other hand, Gram-postivie bacteria will retain the crystal violet dye when washed in a decolorizing solution. The pathogenic capability of Gram-negative bacteria is often associated with certain components of Gram-negative cell walls, in particular, the lipopolysaccharide also known as LPS or endotoxin layer.[1] In humans, LPS triggers an innate immune response characterized by cytokine production and immune system activation. Inflammation is a common result of cytokine (from the Greek cyto, cell and kinesis, movement) production, which can also produce host toxicity. The word Gram is always spelled with a capital letter, referring to Hans Christian Gram, the inventor of Gram staining. While this is an unofficial lab, (not one of the “big” 12) I still want it to go in your quadrille. Please do the following for pre-lab, and make sure you are ready by the due date! Procedure: Setting up your Petri-dishes: 1. Set up your luria broth agar Petri dishes, and refrigerate until ready to use. Record the proper way to fill and prepare a Petri dish in your quadrilles, so as to expose it to as few atmospheric bacteria as possible. Put this procedure in a FLOW MAP as you do it. 2. Allow your agar to cool and gel. Label your Petri dish (the outside of the bottom half of the Petri dish…or the side that has the luria agar in it) with a grease pencil by drawing a diagonal line across dividing the Petri dish in half. Write your name on one side, and your partner’s on the other side. 3. Record the procedures for collecting bacteria (Petri dish) in a FLOW MAP. a. Wash hands thoroughly. Touch any surface (except oral or nasal membranes) and gently touch surface of agar in the portion of the dish designated to you. b. Close Petri dish quickly, and allow partner to do the same. c. Keeping Petri dish upside down (agar on top) place in the incubator at 40° C. 4. Leave Petri dish in incubator for two days, and then check periodically to see if there is any bacterial growth. Wait to do the gram staining for a time when you have a nice colony growing (48-72 hours) 5. Record the procedures for gram staining in your quadrille, in a FLOW MAP. (see next page). 6. Proceed to Gram Stain your bacteria. 7. Observe bacteria under low, medium, and high power (as directed at end of gram-staining procedure). 8. 9. Make six circles in your quadrilles. Two indicating low, medium, and high power…and determine the number of times each is being magnified. (hopefully there will be at least two types of bacteria to identify) Also leave a space for the identification of that bacteria based on shape and arrangement, and whether it is gram positive, or negative. The Gram-Stain Method Procedure: Gram Positive 1. A small sample of a bacterial culture is removed from a culture using a sterile inoculating loop. 2. Follow sterile technique: Heat loop end of inoculating loop in a Bunsen burner flame until red hot. Remove from flame and allow to cool to room temperature (about a minute) DO NOT set loop down, as you will re-expose to bacteria on any surface it may touch. Keeping Petri dish UPSIDE down, use inoculating loop to remove some of the bacterial culture from the agar surface. DO NOT scrape into the agar. Simply rub loop gently over surface. 3. Rub the bacterial suspension onto a clean glass microscope slide. Mix with a drop of bacteria-free saline solution to moisten sample. 4. Using a long handled tongs to hold the glass slide, the bacterial smear is then dried over a Bunsen Burner flame slowly at first and then, when dry, heated for a few seconds to the point when the glass slide is too hot to handle. This fixes (ie kills) the bacteria making the slide safe to handle. Care must be taken not to overheat which will char the cells, and perhaps break the slide. DO NOT TOUCH slide for several minutes. 5. Once cool, the slide is transferred to a support over a sink and flooded with a stain called Crystal Violet Stain. The stain is left on the slide for about 1 minute. This stains all the bacteria on the slide a dark purple color. Note, this stain will not penetrate the waxy cell walls of some bacteria. The following procedures should be accomplished OVER THE SINK: 6. Using a large squirt bottle with distilled H2O, gently wash off the slide with running water 7. The bacterial smear is then treated with Gram's solution which consists of 1 part iodine, 2 parts potassium iodide, and 300 parts water. This iodine solution reacts with the Crystal Violet Stain turning it a very dark shade of blue. It also causes it to be retained by certain types of bacteria in a way which is not really understood. 8. After about 30 seconds the slide is gently rinsed with ethyl alcohol which causes the dye-iodine complex to be washed out of some bacteria but not others. This is called decolorization. If we now looked at the smear through a microscope, the bacteria which had retained the Violet-iodine complex will appear blue-black. These are called Gram-positive. However we would not be able to see those which had lost the dye-iodine complex which are called Gram-negative. The final step in the Gram stain method is, therefore, to stain the Gram-negative cells so they can be seen. Procedure: Counterstaining Gram Negative 9. Next you will treat the smear with a compound which stains the Gram-negative cells a color which contrasts markedly with the blue-black color of the Gram-positive cells. The stain commonly used for this is Safranin red. This is the counterstain we will use. Bacteria in the smear which are Gram-positive are unaffected by the counterstain. 10. The counter stain is left on the smear for about 30-60 seconds and then gently rinsed away with the squirt bottle. 11. After the counterstain has been rinsed off, the slide is placed between some absorbent paper and the excess water gently blotted off. Care must be taken not to rub the slide with the blotting paper because this would remove the adhering bacteria. Viewing and Using Immersion Oil 12. The slide is then placed on a microscope stage, focusing first under low and then medium power. You will not see bacteria at these magnifications, but you may see structures well enough to focus the microscope. It is important to follow this procedure as written. 13. The slide is then prepared with immersion oil. Without removing the slide from the stage, place a tiny drop of immersion oil on the center of the bacterial smear. You will then rotate the high powered objective into the oil. This helps transmit light through the specimen directly to the high-powered microscope lens. Since the light travels through oil, and not the atmosphere, the resolution is increased greatly. Highpowered lenses are required because bacteria are very small. Lab Analysis Questions: 1. Where did you find your bacteria, and why did you choose that location? 2. How is the bacterial cell wall different from the plasma membrane? 3. How is the bacterial cell wall different from the cell walls of other organisms? 4. Why did some bacteria retain the crystal violet, while others retained the safranin? 5. Why would the knowledge of whether a bacterium was gram positive or negative be useful to medical doctors, or microbiologists?