Immunity refers to the ability of the human body to resist disease
advertisement

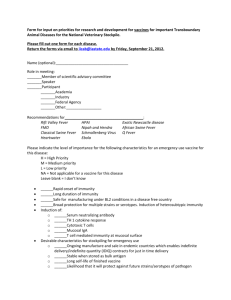
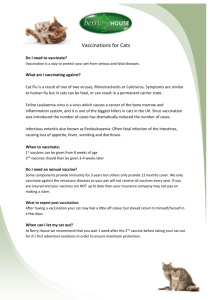
Immunity refers to the ability of the human body to resist disease agents and their toxins through possession of antibodies. When an antigen (Ag) is introduced into the human body, it stimulates the production of antibodies (Ab). Micro-organisms (and their toxins) and vaccines are antigens which evoke an immune response. The immune response is two types:1) The primary response: when an Ag is introduced into the body for the first time, there is a latent period of 3-10 days before Abs appear in the blood. A peak is quickly reached and the level of Abs gradually falls over a period of weeks or months. 2) The secondary (booster) response: the response to a booster dose of the same Ag differs in a number of ways from the primary response: has a shorter latent period and more rapid production of Abs. Abs are produced in abundance and a high level is maintained for a longer period. the Abs produced tend to have a greater capacity to bind to the Ags. The accelerated response is attributed to the immunological memory. A. Humoral Immunity: This type of immunity is due to circulating Abs (Gamma - globulin's also called immunoglobulins). It is a major defense against bacterial infections. On stimulation, B-lymphocytes divide and its daughter cells are transformed into plasmacells. The latter secrete the Abs into the circulation. The types of immunoglobulins are: IgG: Most Abs to infection belong to this class. It is widely distributed in the tissue fluids and are equally available in the intra and extravascular spaces. It can cross the placenta, and so it provides passive immunity to the newborn. IgM: This is the first type produced by the maturing foetus, and it is the main type responsible for the primary immune response. It is mainly intravascular but it does not cross the placenta. (iii) IgA: Found in high concentration in the external secretions: Colostrum, Saliva, tears and intestinal and bronchial secretions. Because of this, IgA is part of the first line of defence against infectious agents. (iv) IgE: Very low in serum and tissue fluids. It has a particular affinity to fix to tissues and so it is able to sensitize mast cells so that upon contact with Ags, the biologically active material present in mast cells is released. Because of this it is called a "reagin". v) Igd: Ab-activity has rarely been demonstrated, and the biologic function is uncertain. B. CELLULAR IMMUNITY: Another way of establishing host resistance is through T-lymphocytes. These cells synthesize and release pharmacologically active substances ("lymphokines") which can kill cells carrying foreign Ags. T-lymphocytes also act against the invader by stimulation of macrophages. This activity of the immune system is known as cell mediated immunity. The peak of activity occurs around the tenth day. Rechallenge by a subsequent infection evokes a secondary response more rapid and of greater intensity. This type of immunity is responsible for intracellular infection (due to viruses and some bacteria e.g. Tubercle bacilli) and fungal infection. Besides infection, cellular immunity is responsible for delayed hypersensitivity reactions, lysis of tumor cells and rejection of tissue or organ transplants. All vertebrates possess in their serum certain proteins and other factors which participate in the immune response. Complements facilitate the Ağ-AB reactions. which serve to control clotting, laying down of fibrin and dilatation of local capillaries to facilitate passage of WBCs. When functioning efficiently, the body is usually well protected by its immune defenses. There are situations in which production of immunity is depressed. Examples are:Congenital and acquired immune-deficiencies. Certain infections like mumps and measles. Presence of passive immunity (maternal Abs). Treatment with immuno suppressive drugs (e.g. steroids) Malnutrition Diabetes mellitus Old age Vaccination and Immunization These terms are often used interchangeably. Vaccination and vaccine derive from vaccinia, the virus once used as smallpox vaccine. Thus, vaccination originally meant inoculation with vaccinia virus to render a person immune to smallpox. Although some persons still prefer that vaccination be restricted to this use, most use it to denote the administration of any vaccine or toxoid. Immunization is more inclusive term denoting the process of inducing or providing immunity artificially. Immunization can be active or passive. Infectious diseases can be prevented by stimulating the individual to develop an active immunologic defence in preparation for meeting the challenge of future natural exposure (active immunization) or by supplying preformed human or animal antibody to individuals already exposed or about to be exposed, to certain infectious agents (passive immunization). In 1979G/1399H the vaccination against certain childhood diseases became obligatory secondary to the issue of a Royal Decree which dictated the sustain of birth certificates until the completion of the primary series of vaccination against: T.B., Diphtheria, Tetanus neonatorum, whooping cough, measles, and poliomyelitis. Latter on the list included coverage against mumps, rubella , hepatitis B viral infections and hib. . In 1991G/1411H a change in the schedule of vaccine administration was implemented (table 1), and continued until the a subsequent schedule of vaccination was approved and implemented in Shawal 17th 1422H/January 1st 2002. The most recent schedule is applied starting Jan. 2008. The changes included in the new vaccination schedule reflect the efforts of continuous monitoring and evaluation of the previous system. It depended largely on the incidence of certain diseases and their impact. It also followed the most recent developments in the manufacturing and industry of vaccines internationally employed. National and local studies and continuous research in the field of immunizable childhood diseases had a great influence and impact. The scientific recommendation of including: - the haemophilus influenza – b vaccine (Hib) to the previous schedule was supported by a Royal approval. [The use of adjuvant vaccines for the first time in Saudi Arabia was a real achievement in this field (DPT + Hib)]. - IPV has been recommended for the first time since ever. - Hepatitis A ,and Varicella vaccines have been recently added. - Measles (mono) vaccine has been indicated at an earlier age. -The two MMR doses are partially considered as boosters to measles vaccine. (see the attached schedule). The routine schedules for active immunization of normal infants and children, and of children not immunized in early infancy have recently been revised by the immunization Practices Advisory Committee, Ministry of Health. The birth certificate will not be issued until the child has completed the recommended primary immunization of infancy period including ( MMR, Varicella and OPV ) at 12 months of age. Active immunization involves administration of all or part of a microorganism or a modified product of that microorganism (e.g. toxoid) to evoke an immunologic response that provides partial or complete protection to the recipient. Vaccines incorporating an intact agent may be either live (usually attenuated) or killed (inactivated). The current available routine schedule for active immunization in Saudi Arabia has been revised and implemented starting January 2008 (Table 3). The types and routes of administration of various vaccines are shown in (Table 4). Schedule for Immunization Several factors influence recommendations concerning the age at which vaccines are administered. a. They are age-specific risks of diseases. b. They are age-specific risks of complications. c. Ability of persons of a given age to respond to the vaccine(s). d. Potential interference with the immune response by maternal antibodies (measles). Modification of the recommended schedule may be necessary because of missed appointment or intercurrent illness. Interruption of a recommended series does not require starting the series over again or adding extra doses, regardless of the interval elapsed. If a dose of DPT or OPV is missed, immunization should occur on the next visit as if the usual interval had elapsed. In contrast, giving doses of a vaccine or toxoid at less than recommended intervals may lessen the antibody response and therefore should be avoided. Doses given at less than recommended intervals should not be counted as part of a primary series. Some vaccines produce local or systemic symptoms in certain recipients when given too frequently (e.g., Td, DT, and rabies). Such reactions are thought to result from the formation of antigen-antibody complexes. * Td = Adult tetanus toxoid (full dose) and diphtheria toxoid (reduced dose) for adult use. * DT = Diphtheria and tetanus toxoids for use in children aged < 7 years old. Table 1: Routine immunization schedule for normal infants and children in Saudi Arabia applied 1991. Table (2): Recent schedule for Vaccination of Newborns in Saudi Arabia.( Jan. 2002Jan.2008) Table (3): Recent schedule for Vaccination of Newborns in Saudi Arabia. Starting January 2008. Table 4: Certain available vaccines and their routes of administration. The Cold Chain Failure of a vaccine to protect an individual child may be due to a number of reasons. * The vaccine may no longer be "antigenic" so that it does not stimulate the body to produce antibodies. * With "live vaccines", which can occur if the vaccine is no longer alive. * Most live vaccines are killed easily by changes of temperature, such as might occur if they are left out of the refrigerator for a long time. (This is particularly true of measles vaccine). ** Vaccines must be kept constantly cold throughout the chain of storage and transport which they have to pass through before reaching the child. Breaks in this "cold chain", as it has come to be called, may be due to a batch of vaccine delivery to a Ministry of Health depot or to a hospital or health centre. It can happen as a result of the breakdown of the refrigerating system. Great care must be taken to try to avoid this happening, and it is always better to have a refrigerator which can run on two different sources of power. Live vaccines are also damaged by sunlight, which is especially likely to happen after they have been prepared (reconstituted) for injection in the clinic or at the school. Vaccines should always be kept in the shade. They can also be affected by detergents or antiseptics in syringes which have not been properly cleaned or rinsed. Even in the best circumstances, vaccines eventually lose their power and it is very important to look at the date of expiry on the container. (This is the date after which the manufactures cannot guarantee the power of the vaccine). The chances that such expired vaccines will fail to protect increase the longer the interval after the expiry date. Live vaccines for injection should be used on the same day that they are reconstituted for injection, that is, after the water (diluent) has been added. Oral poliomyelitis vaccine can be used after opening until the vial is all used up, so long as it is returned to the refrigerator after clinic and kept in the shade. The End