Aplastic Anemia
advertisement

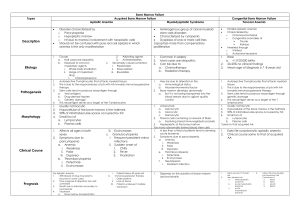
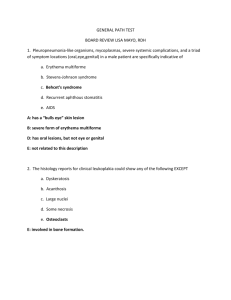
Aplastic Anemia The term “a2plastic anemia” be reserved for cases in which pancytopenia exists, in which there is evidence of decreased production of all the elements of the blood formed in the marrow, including severe hypoplasia or aplasia of the marrow. 1 . Etiology (l). Acquired Aplastic Anemia 1). Drug and chemical agents: It can be divided into two main categories: A. Agents that regularly produce marrow hypoplasia and aplasia if a sufficient dose is given. B . Agents occasionally associated with hypoplasia or aplasia. The pathogenesis of chloramphenicol-associated blood dyscrasias is obscure. Although not all investigators agree, most believe that two types of reactions occur, a reversible suppression of erythropoiesis and irreversible aplasia. Reversible bone marrow suppression primarily involving erythropoiesis occurs in about 50% of patients to whom chloramphenicol is given in large doses. Mitochondrial protein synthesis and mitochondrial ultrastructure of both erythroid and myeloid cell precursors are adversely affected by the usual clinical levels (10 to 16 μg/ ml) of chloramphenicol. Severe and often irreversible bone marrow aplasia, frequently resulting in death, is the second type of reaction to chloramphenicol. In most instances, aplastic anemia becomes evident only after use of the drug has been discontinued. Damage to a high percentage of stem cells has been postulated. Damage to the chromosomes of human blood leukocytes cultured in vitro in the presence of chloramphenicol in usual therapeutic concentrations (10 to 40 μg / ml) provides support for this concept. 2). IONIZING RADIATION. The acute destructive is well known, as is the fact that excessive exposure may result in severe and even fatal aplastic anemia, lower grades of exposure lead to less serious or no detectable changes in the blood. 3 ). infections Pancytopenia with a plastic or hypoplastic marrow has been reported occasionally in association with such conditions as mycobacterial infection and, with increasing frequency of infectious hepatitis. 4). Other cause. Some cases were reported in association with pregnancy, most of the subjects improving after delivery or abortion. (2). "Idiopathic" Aplastic Anemia Although one may search carefully for a possible etiologic agent in cases of pancytopenia, there remain approximately 50% of cases in which no cause is found or suspected. 2. Pathophysiology The basic defect in aplastic anemia appears to be a failure of blood cell production that involves erythrocytes, platelets, and leukocytes. (1). Stem cell deficiency Stem cell population has been decimated or rendered incapable of repopulating the marrow cell mass. The success of marrow transplants in some identical twins and the increased incidence of nuclear abnormalities in some patients with idiopathic marrow aplasia and of chromosome abnormalities in those with Fanconi’s anemia, as well as the fact that defects have been found in all three cell lines in patients with paroxysmal nocturnal hemoglobinuria and marrow hypoplasia, suggest a defect in stem cells. In addition, the marrow content of stem cells capable of forming colonies on in vitro culture is reduced in patients with aplastic anemia. (2). Micro-environment deficiency The failure of marrow infusions to repopulate areas of heavily irradiated marrow (4,000 R) in animals, failure of marrow to regenerate in man after more than 2500 to 3500 Rads have been delivered, and the marrow hypoplasia observed in starvation and in graft-versus-host rejection suggest that the marrow environment is important and in some instances may to unable to support marrow cell growth. (3). Immunological theory The pathogenesis of some patients of aplastic anemia is related to the immunologic mechanism. The marrow and peripheral blood lymphocytes of aplastic anemia can inhibit the colonies formation of normal marrow culture in vitro. The patient of aplastic anemia who received large doses of immunosuppressive drug during transplantation, if the graft was rejected but the marrow function was recovered dramatically. Some patients was treated by ATG or CTX or large doses of steroid alone, will get remission. These evidence can support the immunological mechanism of pathogenesis. 3. Symptoms and Signs In the majority of patients the initial symptoms of acquired aplastic anemia are manifestations of anemia and/or bleeding, but fever or infection are not uncommon. The onset is insidious. The symptoms and signs depend on the rapidity with which the anemia progresses and whether or not complicating infections and hemorrhage develop. Infection and hemorrhage, in turn, depend in part on the degree of granulocytopenia and thrombocytopenia. 4. Laboratory findings (l). Blood changes 1). Hemoglobin and RBC were decreased. The anemia was normochromic normocytic type. 2). Leukocytopenia----The leukocytes formed in the bone marrow are affected chiefly and thus the differential count may contain as many as 70-90% lymphocyte. 3). Thrombocytopenia. The bleeding time is usually moderately prolonged and the blood clot retracts poorly when thrombocytopenia is present. (2). Bone Marrow The majority, even 60 to 100%, of the nucleated cells are lymphocytes. In marrow biopsy specimens from patients with typical aplastic anemia, only yellowish white material, consisting chiefly of fat, fibrous tissue, and lymphocytes, is seen. 1. Acute and chronic type of aplastic anemia Onset Infection Bleeding WBC Platelet Reticulocyte Anemia Hb Bone marrow Prognosis Acute type Sudden Almost every cases Frequently and heavy 1.0x109/L 10 x109/L 0 or 0.1-0.2% No or mild Normal or mild decrease Severe aplasia Poor Chronic type Insidious Rare and mild Mild 9 2.0 x10 /L -3.0 x109/L 20 x109/L -30 x109/L 0.5%± Moderate to severe Decrease Hypoplasia or aplasia Better than acute type 6. Differential diagnosis (l). Other diseases with pancytopenia----acute leukemia (subleukemic or aleukemic type), megaloblastic anemia, histiocytosis, carcinoma metastasis to the marrow (leukoerythroblastic reaction or anemia) (2). Paroxysmal nocturnal hemoglobinuria----Ham’s test and Rous test will positive in PNG. Peripheral blood was pancytopenia in PNH. The bone marrow in PNH was hyperplasia, but in the late stage of PNH the bone marrow will hypoplasia. (3). Thrombocytopenic purpura and aganulocyrosis----Occasionally only anemia or leukopenia, thrombocytopenia or “bicytopenia” may be the first presenting sign in aplastic anemia. 7. Treatment Treatment involves 1). a thorough search for a possible cause and prohibition of further exposure to a suspected drug or other toxic agent even if the evidence is not very impressive. 2). maintenance of hemoglobin levels by blood transfusion. 3). Prevention and management of hemorrhage and infection. 4). attempts to stimulate hematopoiesis and marrow regeneration. 5). evaluation of the possible role of the spleen in the destruction of transfused red cells or platelets, and the removal of this organ if the evidence suggests that this may be wise and the patient can tolerate the procedure. 6). Possible marrow transplantation in carefully selected patients. (l). Avoidance of Further Exposure Although it is obvious that the first requirement is the avoidance of further exposure to an etiologic noxious agent, this is sometimes overlooked or the cause is not recognized. Exposure to infections should be avoided if possible. This may involve the restriction of visitors, reverse isolation, or the use of plastic isolators or laminar air-flow units. The use of absorbable prophylactic antibiotics is not recommended since this encourages the development of resistant strains and atypical infections. (2). Management of hemorrhage When hemorrhage is a problem, administer of fresh blood, platelet-rich plasma, or platelet concentrates in amounts is sufficient to maintain the platelet concentration. (3). Relief of Anemia The mainstay of treatment has been the transfusion of whole blood for the relief of anemia. Currently specific blood components (leukocytepoor packed red cells, platelet-rich plasma or concentrates, and less often leukocyte concentrates) are being used in many centers. The available blood supplies were effectively utilized with mininal side effects such as isoimmunization and undesirable blood volume expansion. (4). Stimulation of Hematopoiesis and Marrow Regeneration The measures most widely employed to improve marrow function has been administration of anabolic steroids (testosterone, oxymetholone, etc). Adrenal corticosteroids have been used extensively in the treatment of patients with aplastic anemia. Phytohemagglutinin has been used in an attempt to stimulate mitosis and marrow regeneration with apparent good response in some subjects. (5). Immunosuppressive agents If the pathogenesis of aplastic anemia is due to immuno-mechanism, immunosuppressive agents such as cyclophosphamide, anti-lymphocyte globulin (ALG), antithymal globulin (ATG) and Cyclosporin A can be used. (6). Chinese traditional medicine (7). Splenectomy (8). Heamtopoietic Grafts There has been great interest in the use of hematopoietic grafts in humans and many attempts to transplant bone marrow have been made in patients with leukemia and marrow aplasia. Zhonglu