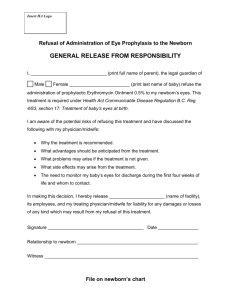
ANTENATAL CARE
advertisement

INTRODUCTION TO POGS MDG COUNTDOWN Too many mothers and newborns are dying. o 600,000 women die from preventable deaths worldwide (WHO 1996) o 162 women die for every 100,000 live births (Philippines FPS 2006) o Many of maternal deaths occur at home and are never recorded Most maternal deaths occur during labor, delivery and the immediate postpartum period indicating that proper care during labor and delivery are critical. The five major direct causes of maternal mortality: 1. Hemorrhage. Bleeding in a pregnant woman can happen at any time during pregnancy. However, it is the hemorrhage that occurs after childbirth that is a main cause of maternal death. Postpartum bleeding is most often due to failure of the uterus to contract effectively (uterine atony). Lacerations and tear in the birth canal and retained placental tissues are other causes of postpartum hemorrhage. 2. Hypertension. Women can develop hypertension during pregnancy and if uncontrolled and untreated may develop convulsion that can lead to death. 3. Infection. Failure to observe clean birth protocols can result to infections that adversely affect the health of the mother and baby. 4. Obstructed labor. This is often due to mismanaged labor and cephalopelvic disproportion. Women who have prolonged or obstructed labor can develop vesicovaginal or rectovaginal fistulas. They are also likely to develop postpartum bleeding. 5. Complications of abortion. Women with unplanned pregnancies may often resort to induced abortion. This can be prevented if women have access to family planning information and services and safe post abortion care. As to child health, The Philippines is one of the 42 countries that account for 90% of global under-five mortality. Neonatal deaths account for almost 40% of all child mortality. The leading causes of neonatal deaths are prematurity, sepsis or pneumonia, and asphyxia. Reasons for high maternal and neonatal mortality: 1. Young age at marriage & first pregnancy 2. Domestic violence and gender inequality 3. Poor maternal health 4. Poor hygiene during and after delivery 5. Lack of/poor newborn care 6. The three delays POGS MDG COUNTDOWN: Capacity Enhancement Program for Midwives 2010 1 THE THREE DELAYS: Barriers in accessing care on time 1. Delay in deciding to seek medical care a. Failure to recognize danger signs b. Lack of money c. Unplanned/unwanted pregnancy d. Lack of companion in going to health facility e. No person to take care of children/home. f. Fear of being ill treated in health facility 2. Delay in identifying and reaching the appropriate facility a. Distance from a woman’s home to health facility/provider b. Lack of/poor condition of roads c. Lack of emergency transportation d. Lack of awareness of existing services e. Lack of community support 3. Delay in receiving appropriate and adequate care at the health facility a. Lack of health care providers b. Shortage of supplies c. Lack of equipments d. Lack of competence of health providers e. Weak referral system MILLENIUM DEVELOPMENT GOALS In December 2000, 189 Heads of States or Governments jointly endorsed the Millennium Declaration which committed signatories to achieving, by 2015, 8 millenium development goals. The Philippines is one of the signatories to this declaration. Of the 8 goals, Goals 4 and 5 relate to reduction of child mortality and improvement of maternal health. 1. Eradicate extreme poverty and hunger 2. Achieve universal primary education 3. Promote gender equality and empower women 4. Reduce child mortality 5. Improve maternal health 6. Combat HIV/AIDS, malaria and other diseases 7. Ensure environmental sustainability 8. Develop a global partnership for development MDG 4 REDUCE CHILD MORTALITY 1. Reduce Under 5-mortality rate from 80.0 to 26.7 (per 1,000 LB) 2. Reduce Infant mortality rate from 57.0 to 19.0 (per 1,000 LB) MDG 5 IMPROVE MATERNAL HEALTH Reduce maternal mortality by 75% by 2015 (for the Philippines the target is to reduce MMR from 209 to 52 deaths per 100,000 live births). The current maternal mortality rate is 162 per 100,000 livebirths (2006 FHS) How will we make it happen? 1. A skilled health care professional attends every childbirth 2. Every woman has access to Emergency Obstetric and Newborn Care (EmONC) 3. Family planning services to help women space their pregnancies POGS MDG COUNTDOWN: Capacity Enhancement Program for Midwives 2010 2 A SKILLED ATTENDANT is an accredited health professional (a midwife, nurse or doctor) who has been educated and trained to proficiency in the skills needed to manage normal pregnancies, childbirth and the immediate postnatal period, and in the identification, management and referral of complications in women and newborns. EMERGENCY OBSTETRIC AND NEWBORN CARE refers to the elements of obstetric & newborn care needed for the management of normal and complicated pregnancy, delivery, postpartum periods and the newborn. 1. Early detection and treatment of problem pregnancies to prevent progression to an emergency. 2. Management of emergency complications (for the mother – hemorrhage, obstructed labor, pre-eclampsia/eclampsia, infection. For the newborn – infection, asphyxia, hypothermia.) There are 2 levels: Basic (BEMONC) and Comprehensive (CEMONC) Basic emergency obstetric and newborn care – signal functions 1. Parenteral (IV or IM) administration of Antibiotics 2. Oxytocin 3. Anticonvulsants 4. Manual Removal of Placenta 5. Removal of Retained Products of conception 6. Assisted Vaginal Delivery 7. Administration of corticosteroids in preterm labor 8. Essential Newborn Care Comprehensive emergency obstetric care signal functions – all of BEMONC + 1. Surgery (Cesarean Section) 2. Blood Transfusion Philippine midwifery practice is guided by the Midwifery Act of 1992 (R.A.7392). Aside from providing care to the woman during normal pregnancy and childbirth, the law has provided added skills that the midwife must learn to do her task competently. These include: 1. Repair of first and second degree perineal lacerations to control bleeding 2. Internal examination except when the woman has antepartum bleeding 3. Intravenous fluid infusion during obstetric emergencies 4. Giving oxytocic drugs after delivery of placenta 5. Giving vitamin K to the newborn The midwife must adhere to her scope of work and training to protect the safety of those who seek her care. As a health professional, she is duty bound to improve and continuously update and enhance her knowledge, skills and practice by attending and participating in continuing professional education (midwifery) activities. POGS MDG COUNTDOWN: Capacity Enhancement Program for Midwives 2010 3 ANTENATAL CARE Focused antenatal care is based on the premise that every pregnancy is at risk for complications. All women should receive the same basic care including identifying complications. This model of antenatal care involves a minimum of 4 visits in normal or uncomplicated pregnancies. It stresses quality rather than number of visits and has essential goal-directed elements including screening for diseases that complicate pregnancy like pre-eclampsia and anemia. It also reduces cost, lessens workload and provides more time to interact with patients thereby improving quality of care. Focused Antenatal Care components: 1. General Assessment of the Pregnant Woman 2. Screening for diseases that complicate pregnancy: hypertension, anemia, syphilis 3. Preventive measures: tetanus immunization, iron and folic acid supplementation 4. Health Education: Self Care, Nutrition and Danger Signs during Pregnancy 5. Birth Plan Objectives of Prenatal Care 1. Detection of diseases which may complicate pregnancy 2. Education of women on danger and emergency signs & symptoms 3. Preparation of the woman and her family for childbirth Steps to follow in Prenatal Care 1. IMMEDIATE ASSESSMENT for emergency signs: (QUICK CHECK) Unconscious/Convulsing Vaginal bleeding Severe abdominal pain Looks very ill Severe headache with visual disturbance Severe difficulty in breathing Fever Severe vomiting *Attend to sick woman quickly, 2. Make the woman comfortable. Greet her, make sure she is comfortable and ask how she is feeling. If first visit, register the woman and issue a Mother and Child Book/Home Based Maternal Record 3. Assess the pregnant woman FIRST visit: How old is patient? Past Medical History Obstetric History: Gravidity? LMP? AOG? Ask about or check record for prior pregnancies: o Convulsions o Stillbirth or death in the first day o Heavy bleeding during or after delivery o Prior cesarean section, forceps or abortion POGS MDG COUNTDOWN: Capacity Enhancement Program for Midwives 2010 4 ON ALL VISITS: Check duration of pregnancy (AOG) Ask for bleeding/danger signs during this pregnancy Check record for previous treatments received during this pregnancy Prepare birth and emergency plan Ask patient if she has other concerns Give education and counseling on family planning THIRD TRIMESTER Leopold’s exam, fetal heart beat Give education & counseling on family planning Do not perform vaginal exam as a routine prenatal care procedure. Always record findings. All pregnancies are at risk. Encourage all pregnant women to deliver in the health facility. Refer patients with abnormal findings to doctor or to higher facility. 4. Get baseline laboratory information of the woman on the first or following the first visit. Hemoglobin, blood type Urinalysis If not available, refer to the nearest RHU or hospital for the tests. 5. Screen for diseases that may complicate pregnancy: Check for pallor or anemia Ask about getting tired easily or shortness of breath during routine work, drowsiness, palpitations, headaches – these may indicate anemia. On 1st visit, check hemoglobin & blood type. The normal hemoglobin (Hb) cut-off level for a pregnant woman is 11g/dl. If Hb is <8 g/dl, refer to doctor for work-up and treatment of anemia. On subsequent visits; 1) Look for conjunctival pallor. 2) Look for palmar pallor. If pallor: Is it severe pallor? Some pallor? 3) Count number of breaths in one minute. 6. Check for hypertension/pre-eclampsia Measure BP in sitting position. If blood pressure is above 140/90 early in pregnancy, she is suffering from chronic hypertension and should be referred to a doctor. If diastolic BP is 90 mm Hg or higher repeat measurement after 1 hour rest. If diastolic BP is still 90 mm Hg or higher ask the woman if she has: 1) Severe headache 2) Blurred vision 3) epigastric pain Check urine for protein. Diastolic BP>90 mm Hg, especially if with severe headache, blurred vision and epigastric pain and ++ urine protein are signs of severe pre-eclampsia – REFER immediately! POGS MDG COUNTDOWN: Capacity Enhancement Program for Midwives 2010 5 7. Screen for diseases that may complicate pregnancy: Check for gestational diabetes ASK ABOUT – Family history (first degree) of diabetes & history of obesity. – Past pregnancy for difficult labor, large babies, congenital malformations and previous unexplained fetal death. LOOK FOR Refer for glucose test: – signs of maternal overweight or obesity at 24-28 wks for low risk or – Polyhydramnios immediately if high risk – Signs of large baby or fetal abnormality – Vaginal infection. 8. Check for fever, burning sensation on urination and abnormal vaginal discharge. • Ask about episodes of fever or chills and take temperature. • Ask about pain or burning sensation on urination. • Ask about presence of abnormal vaginal discharge, itching at the vulva or if partner has a urinary problem. 9. Give preventive measures: Immunize against tetanus. Tetanus Toxoid Immunization Schedule Vaccine Minimum Interval Duration of Protection TT1 at first contact with woman NIL – no protection 15-49 yrs or at first antenatal care visit TT2 at least 4 weeks after TT1 • Infants born to the mother will be protected from neonatal tetanus • 3 years of protection for the mother TT3 At least 6 weeks after TT2 • Infants born to the mother will be protected from neonatal tetanus • 5 years of protection for the mother TT4 At least 1 year after TT3 • Infants born to the mother will be protected from neonatal tetanus • 10 years of protection for the mother TT5 At least 1 year after TT4 • Infants born to the mother will be protected from neonatal tetanus • Lifetime protection for the mother To be protected, a pregnant mother must receive at least 2 doses of tetanus toxoid. The last dose should be at least two weeks before delivery. 10. Give preventive measures Give MEBENDAZOLE to treat for intestinal parasites. 500 mg single dose once in six months (after 1st trimester) 11. Give iron and folate supplementation to prevent anemia and neural tube defects: Ferrous sulfate 320 mg (60 mg elemental iron) & 250 mcg Folate POGS MDG COUNTDOWN: Capacity Enhancement Program for Midwives 2010 6 If Hgb <80 gm/dl→ double the dose of iron. Refer to doctor for work-up of anemia. 12. Give preventive intermittent treatment for falcifarum malaria (if area is endemic) 13. Provide health information, advice. Counsel on danger signals HEALTH INFORMATION Nutrition Self-care during pregnancy Effect of tobacco, alcohol & drugs Breastfeeding Birth & Emergency situations Schedule of appointment DANGER SIGNS Vaginal bleeding Convulsions Severe headache Severe abdominal pain Fast or difficult breathing Fever or burning urination 14. Encourage the woman to come back for return visits. At least 4 routine antenatal visits 1st visit: before 4 months 2nd visit: 6 months 3rd visit: 8 months 4th visit: 9 months – return if undelivered within 2 weeks after the EDC. Pregnant women who do not come for prenatal care should be visited at home. THE BIRTH AND EMERGENCY PLAN What is a birth plan? • A written document prepared during the first prenatal consultation. Plan may change anytime during pregnancy if an abnormality develops. • Discussed by the patient with the skilled birth attendant. • Contains information on: – the woman’s condition during pregnancy – preferences for her place of delivery and choice of birth attendant. Discuss why facility delivery vs home delivery with skilled attendant is recommended – available resources (transportation, companion, money) for her childbirth and newborn baby – preparations needed (blood donor, referral center) should an emergency situation arise during pregnancy, childbirth and postpartum. Emergency Plan • Discuss how to prepare for an emergency in pregnancy Advise on danger signs, signs of labor Where to go? How to go? What to bring? With whom will you go? How much will it cost? Who will pay? How will you pay? Start saving for these possible costs now. Who will care for your home and other children when you are away? POGS MDG COUNTDOWN: Capacity Enhancement Program for Midwives 2010 7 Birth and Emergency Plan I know that any complication can develop during delivery. I know that I should delivery in a health facility. I will be attended at delivery by ___________________________________ I plan to deliver at _____________________________________________ This is a Philhealth accredited facility _____ Yes ____ No The estimated cost of the maternity package in this facility is P___________ (inclusive of newborn care) The mode of payment is ________________________________________ The available transport is _______________________________________ I have contacted ____________________________________ to bring me to the hospital/health center. I will be accompanied by ________________________________________ _____________________________ will take care of my children/home while I am in the health facility. In case of a need for blood transfusion, my possible donors are; ____________________________________________________________ _____________________________________________________________ In case of complications, I will be referred right away to: ______________________________________ Contact Person _______________________________________________ Address: ____________________________________________________ Tel No.: ____________________________________________________________ POGS MDG COUNTDOWN: Capacity Enhancement Program for Midwives 2010 8 PROVIDING CARE DURING LABOR, CHILDBIRTH AND IMMEDIATE POSTPARTUM STEPS TO FOLLOW IN INTRAPARTAL CARE 1. Examine the woman for emergency signs. • Unconscious, Convulsing • Vomiting • Severe headache with blurring of vision • Vaginal bleeding • Severe abdominal pain • Looks very ill • Fever • Severe breathing difficulty ** Do NOT make a very sick woman wait, attend to her quickly! 2. Greet the woman and make her comfortable. Ask for informed consent before examination or any procedure Respect her privacy Inform her of results of examination Reassure 3. Assess the woman in labor. o Take the history of labor and record on the labor form. o Review Home Based Maternal Record (HBMR)/ Mother and Child Book When is delivery expected? Preterm or term? Prior pregnancies Birth plan o Assess uterine contractions: intensity, duration, and interval o Observe the woman’s response to contractions. o Perform abdominal exam: (Leopold’s maneuver, FHT) between contractions 4. Determine the stage of labor. Explain to the woman that you will perform a vaginal examination and ask for her consent. Respect her privacy Observe standard precautions (wash hands, wear gloves, ..) Inspect the vulva for: o Bulging perineum o Any visible fetal parts o Vaginal bleeding o Leaking amniotic fluid; if yes, is it meconium stained, foul smelling? o Warts, keloid tissue or scars that may interfere with delivery Perform gentle vaginal examination (do not start during contraction). Explain findings to the woman. Reassure her. Record findings in labor record or partograph. POGS MDG COUNTDOWN: Capacity Enhancement Program for Midwives 2010 9 SIGNS Bulging thin perineum Vagina gaping and head visible • Full cervical dilation Cervical dilatation - Multigravida >5 cm - Primigravida >6 cm CLASSIFY Imminent Delivery Cervical dilatation at >4cm • • Cervical dilatation at 0-3 cm Contractions weak and <2 in 10 minutes • MANAGE Manage 2nd stage of labor Record in partograph Late Active Labor • • • Manage 1st stage of labor Record in partograph Record in labor record Early Active Labor • • • • Manage 1st stage of labor Record in partograph Record in labor record Record in labor record Not in Labor • 5. Decide if the woman can safely deliver. If there is indication for referral … • in early labor & the referral hospital can be timely reached: → Refer urgently • in late active labor: Monitor progress of labor and deliver the baby Prepare for immediate referral if still necessary • If the woman or her family refuses referral Explain the possible consequences Continue to take care of her 6. Give supportive care throughout the labor. Explain procedures, seek permission and discuss findings with the woman and her family. Examine the woman in a place where she is not exposed to people other than the examining person and her choice of companion NEVER LEAVE a woman in labor alone. Encourage woman to: wash from her waist down or take a bath at the onset of labor. empty her bladder and bowels. Remind her to empty her bladder every 2 hours. (A full bladder may prolong the labor) move freely (if BOW is not ruptured). Respect and support her choice of a birthing position drink as she wishes. Contractions will make her thirsty and the sugar will give her energy for her labor. Do not give solid foods – this may make her vomit. 7. Monitor and manage labor. First stage: not yet in active labor, cervix is dilated 0-3 cm., contractions are weak, <2 in 10 minutes Every hour: check for emergency signs, frequency, intensity & duration of contractions, FHR, mood and behavior. Every 4 hours: check vital signs and cervical dilatation. Record findings in Labor record Assess progress of labor: After 8 hrs, if contractions are stronger & more frequent but no progress in cervical dilatation: REFER POGS MDG COUNTDOWN: Capacity Enhancement Program for Midwives 2010 10 First stage: in active labor, cervix is dilated at 4 cm or more Check every 30 mins for emergency signs, frequency and duration of contractions, FHR, mood and behavior. Check every 4 hours: fever, PR, BP, cervical dilatation. Record time of rupture of membranes and color of the amniotic fluid. Record findings in partograph. RELIEF OF PAIN AND DISCOMFORT 1. Suggest change of position 2. Encourage mobility as comfortable for her 3. Encourage proper breathing: breath more slowly, make a sighing noise, make 2 short breaths followed by a long breath out. 4. Massage her lower back if she finds it helpful CAUTION 1. DO NOT do IE more frequently than every 4 hours. 2. DO NOT allow the woman to push unless delivery is imminent → pushing does not speed up labor, mother will become tired, cervix will swell. 3. DO NOT give medications to speed up labor → DANGEROUS: may cause trauma to the mother and baby. 4. Do not do fundal pressure may cause uterine rupture, fetal death Second stage: from full dilatation (10cm) of the cervix until birth of baby. How to tell if a woman is in the 2nd stage of laor On IE, cervix is fully dilated Woman wants to bear down Strong uterine contractions every 2-3 minutes Bulging thin perineum, fetal head visible during contractions. BOW will rupture MONITORING THE SECOND STAGE Check uterine contractions, fetal heart rate, mood and behavior Continue recording in the partograph REMINDERS: Massaging or stretching the perineum have not been shown to be beneficial. DO NOT apply fundal pressure to help deliver the baby → may harm mother and baby. 8. DELIVER THE BABY Implement the 3 CLEANS 1. Clean hands. Wear double gloves. 2. Clean delivery surface 3. Clean cutting and care of the cord Stay with the woman and encourage her. Make her comfortable. Encourage the mother to bear down when the baby’s head is coming down. When the birth opening is stretching, support the perineum and anus with a clean swab to prevent lacerations POGS MDG COUNTDOWN: Capacity Enhancement Program for Midwives 2010 11 Ensure controlled delivery of the head . 9. Keep one hand on the head as it advances during contractions. Keep the head from coming out too quickly Support the perineum with other hand. Discard pad and replace when soiled to prevent infection During delivery of the head, encourage woman to stop pushing and breathe rapidly with mouth open. Gently feel if the cord is around the neck o If it is loosely around the neck, slip it over the shoulders or head o If it is tight, place a finger under the cord, clamp and cut the cord, and unwind it from around the neck. Gently wipe the baby’s nose and mouth with a clean gauze or cloth. Wait for external rotation (within 1-2 min), head will turn sideways bringing one shoulder just below the symphysis pubis and other facing the perineum Apply gentle downward pressure to deliver top shoulder then lift baby up to deliver lower shoulder. Gently deliver the rest of the baby. Note the time baby is delivered. Put baby on mother’s abdomen in prone position. Cover with dry towel. Thoroughly dry the baby immediately. Wipe eyes. Discard wet cloth. Put baby prone on mother’s abdomen, in skin-to-skin contact. Keep the baby warm. Exclude 2nd baby by palpating mother’s abdomen. Give 10 units oxytocin IM to the mother. (Active management of the 3rd stage of labor). *May be done by midwife under supervision of doctor. Watch for vaginal bleeding. Remove first set of gloves. CLAMP AND CUT THE CORD Feel the cord. When no more cord pulsation is felt on the cord (usually within 3 mins.), clamp the cord 2cm from the base using sterile plastic cord clamp Sweep the cord and apply a Kelly forceps 5cm from the base and then cut in-between. Observe stump for blood oozing. Do not bandage or bind the stump. Leave it open POGS MDG COUNTDOWN: Capacity Enhancement Program for Midwives 2010 12 THIRD STAGE: between birth of the baby and delivery of the placenta. o Deliver the placenta by controlled cord traction (with counter traction on the uterus above the symphysis pubis). o Massage the uterus over the fundus. o Inject oxytocin.10 U IM (if not yet given as part of active management) o Encourage initiation of breastfeeding. Keep the baby on mother’s abdomen for 60-90 min. o Check that the placenta and membranes are complete. Put the placenta into a container for disposal. ACTIVE MANAGEMENT of the third stage of labor (under supervision of doctor) o Cord is clamped after cord pulsations have stopped. o Oxytocin is given within 2 minutes of delivery of the baby. o Placenta is delivered by controlled cord traction with countertraction on the uterus above the symphysis pubis. o Massage fundus. 10. Monitor closely within 1-hour after delivery (Immediate postpartum period) and give supportive care. Check for vaginal tears and bleeding. Clean the woman and make her comfortable. Check BP, PR, emergency signs & uterine contraction every 15 minutes. Initiate breastfeeding within 1-hour when the baby is ready. 11. Continue care after 1 hour postpartum. Keep watch closely for at least 2 hours. Temperature, BP and pulse every 30 minutes Check at 2, 3 and 4 hours, then every 4 hours: o emergency signs o hardness of the uterus Check for bladder distension if unable to void. Advise clean cloth/napkin to collect vaginal blood. Eat and drink high-energy foods that are easily digestible. ** Companion: to watch her and to call you for bleeding or pain, dizzy or for any other problem For the baby Keep the baby in the room with the mother, in her bed or within easy reach. Support exclusive breastfeeding on demand, day and night, as often and as long as the baby wants. Immunize according to the EPI schedule. Mother and companion to watch the baby: breastfeeding difficulty difficulty of breathing cold feet bleeding from the cord POGS MDG COUNTDOWN: Capacity Enhancement Program for Midwives 2010 13 Check baby at around 4 and 8 hours and then daily: cold feet, breastfeeding and breathing difficulty. 12. Educate and counsel on family planning and provide the family planning method if available. Ask what are the couple’s plans regarding having more children. Give relevant information and advice. Advice that exclusive breastfeeding is the best contraceptive in the 1st six months. Help her to choose the most appropriate method for her and her partner. 13. Inform, teach and counsel the woman on important MCH messages. Talk to the woman when she is rested and comfortable. Also give important information and advice to her companion. Take time to explain, use visual aids, and demonstrate important lessons. Encourage them to participate actively in discussions and to ask questions. 13. Discharge the woman and her baby. The woman and her baby may be discharged 24 hours after delivery. Ensure that the woman is able to breastfeed successfully before discharge. Repeat important health information. Check understanding and arrange follow-up. POGS MDG COUNTDOWN: Capacity Enhancement Program for Midwives 2010 14 THE PARTOGRAPH The partograph is a useful tool for monitoring the progress of labor. Use it to avoid unnecessary interventions so maternal and neonatal morbidity are not needlessly increased, to intervene in a timely manner to avoid maternal and neonatal morbidity or mortality and to ensure close monitoring of the woman in labor. USES OF THE PARTOGRAPH ► Assessment of progress of labor Cervical dilatation Contractions Alert and action lines ► Assessment of maternal well being Pulse, temperature, blood pressure Urine voided ► Assessment of fetal well being Fetal heart rate and pattern Color of amniotic fluid Parts of the Partograph The upper colored portion is where progress of labor.is plotted. Progress of Labor The lower portion is where observations of the maternal and fetal well-being are written. Maternal & Fetal well being ALERT LINE ACTION LINE This is an enlarged picture of upper portion of the partograph. It is divided evenly into small boxes by gridlines vertically and horizontally. Each horizontal gridline corresponds to the cervical dilatation in centimeter from 4 to 10. While the vertical gridlines indicate the time, in hours, the patient is in active labor. The upper portion is also divided into 3 colors – green, yellow, and red.. The boundary between the green and yellow parts forms a diagonal line called the alert line which starts at 4 cm. up to 10 cm At the alert line, the onset of the active phase of labor (4 cm), the patient is expected to reach full dilation at the rate of 1 cm/hour. POGS MDG COUNTDOWN: Capacity Enhancement Program for Midwives 2010 15 Parallel and 4 hours to the right of the alert line is another line formed by the boundary between the yellow and red part which is again highlighted here. This is the action line. Note that it too starts at 4 cm and ends in 10 cm. The following are examples of risk factors which may have been identified during prenatal and before the start of labor where the use of the partograph is not recommended. These patients should be referred to higher facility. Very short stature Anemia, severe Antepartum hemorrhage Multiple pregnancy Severe pre-eclampsia and eclampsia Malpresentation Fetal distress Very premature labor Previous cesarean section Obvious obstructed labor PARTOGRAPH AND CRITERIA FOR ACTIVE LABOR Start the partograph only when the woman is in ACTIVE labor (4 cm or more) and is contracting enough (3-4 contractions in 10 min) Label with patient identifying information THE PROGRESS OF LABOR Plot CERVICAL DILATATION - This is plotted or recorded using “X” - Perform the internal examination (IE) every 4 hours, or more frequently if necessary. If the woman is admitted in labor in the latent phase (less than 4 cm dilated ) – use the LABOR RECORD to record your findings (BP, FHT etc). If she remains in the latent phase for the next 8 hours, labor is prolonged and she must be transferred to the hospital. PLOTTING CERVICAL DILATATION WHEN LABOR IS IN THE ACTIVE PHASE Plot or record cervical dilatation on the alert line whenever woman is admitted in the active phase of labor. The plotting of the cervical dilatation will remain on or to the left of the alert line when there is a satisfactory progress in labor MONITOR EVERY 4 HOURS (or more frequently if necessary): Vital signs: BP, Temperature, PR and cervical dilatation. MONITOR EVERY HOUR: FHT, frequency, intensity and duration of contractions, woman’s mood and behavior. OTHER FINDINGS TO RECORD Vaginal bleeding (0, +, ++, +++) Time membranes ruptured “ I ” if membranes are intact Color of amniotic fluid “ C ” membranes are ruptured and amniotic fluid is clear “ M ” amniotic fluid is stained “ A ” Amniotic fluid is absent “B” Amniotic fluid is bloody Urine voided (yes, no) POGS MDG COUNTDOWN: Capacity Enhancement Program for Midwives 2010 16 IF PARTOGRAPH PASSES THE ALERT LINE: Reassess woman and consider criteria for referral. Alert transport services. Empty bladder. Ensure adequate hydration but omit solid foods. Encourage upright position and walking if woman wishes. Monitor intensively. If referral long, reassess in 2 hours and refer if no progress. If partograph passes action line… refer urgently to an EmOC facility unless delivery is imminent. ABDOMINAL EXAMINATION DURING PREGNANCY 1. Inspection • Check if there are any scars. If the scar was from CS → REFER • Is abdomen normal shape and size? → twins → transverse lie → breech 2. Palpation • Checking the fundic height • Estimation of fetal weight • Leopold’s maneuver Why measure the fundic height? 1) To determine if the uterine size is compatible with the age of gestation Fundic height coincides with the age of gestation from 18-30 weeks 2) To aid in the estimation of fetal weight POGS MDG COUNTDOWN: Capacity Enhancement Program for Midwives 2010 17 HOW TO MEASURE THE FUNDIC HEIGHT 1. Bladder must be empty 2. Apply the tape with the calibration hidden to avoid bias 3. Measure from upper edge of symphysis pubis to top of the fundus (do not push the fundus down) POSSIBLE PROBLEMS WITH FUNDIC HEIGHT Fundic height is too large Fundic height is too small • Computed AOG is wrong • Computed AOG is wrong • Multiple pregnancy • Baby is not growing well (IUGR) • Polyhydramnios ↓ • Molar Pregnancy → REFER! • Pregnancy with Myoma or Ovarian Tumor LEOPOLD’S MANEUVER First Maneuver: WHAT OCCUPIES THE FUNDUS? • Face the woman’s head with both hands, feel the height of the fundus. • Which part of the fetus do you feel? 2nd Maneuver: • Feel the sides of the uterus to find the position of the baby’s back and extremities. – Back feels smooth – Extremeties feel irregular 3rd Maneuver: IDENTIFY PRESENTING PART • Grasp area immediately above the symphysis between thumb and fingers – HEAD: hard and round, movable if not engaged – BREECH: feels softer and irregular 4th Maneuver • Face the woman’s feet. Place fingers on both sides of the lower abdomen and press downwards and inwards • Determine fetal occipital prominence • Helps to identify the presenting part and whether it is engaged POGS MDG COUNTDOWN: Capacity Enhancement Program for Midwives 2010 18 INTERNAL EXAMINATION DURING LABOR WHEN TO DO AN INTERNAL EXAMINATION • ONLY DURING LABOR • When the BOW ruptures (to rule out cord prolapse) • If malpresentation is suspected on abdominal examination • Before transferring a woman to another facility to ensure she is not likely to deliver on the journey. • In the 3rd stage, if there is postpartum hemorrhage, caused by retained placenta or suspected laceration. If the woman has had vaginal bleeding after 5th month of pregnancy: DO NOT PROCEED. NEVER do an I.E. unless you have a good indication for doing so. Every I.E. may bring INFECTION to the woman and her baby. PROCEDURE FOR INTERNAL EXAMINATION 1. Explain to the woman what you are going to do. 2. Take full aseptic precautions 3. Rinse the vulva with clean water. 4. Wear clean gloves 5. INSPECT THE VULVA: a. Is there amniotic fluid? Is it clear or meconium stained? b. Is there any abnormal discharge, blood or pus? 6. Feel inside the vagina with the middle and index fingers. WHAT TO NOTE DURING INTERNAL EXAMINATION 1. Cervical Dilatation 2. Bag of waters 3. Presenting part 4. Pelvis (architecture, adequacy of diameters) WHAT IS CERVICAL DILATATION • • • • Gradual opening of the cervix Measured in centimeters Feel with your 2 fingers The fully dilated cervix is 10 cm open. Assessing Cervical Dilatation Insert the middle and index finger into the open cervix and gently open them to the cervical rim. The distance between the outer rim of both fingers is the cervical dilatation 1 finger = 1.25 cm 2 fingers = 3 cm 3 fingers = 4.5 cm 4 fingers = 5.5 cm 5 fingers = 7 cm 6 fingers = 8.5 cm 7 fingers = 9.5 cm POGS MDG COUNTDOWN: Capacity Enhancement Program for Midwives 2010 19 DETERMINE STATUS OF BAG OF WATERS (BOW) • Is BOW intact or ruptured? • Is there amniotic fluid leaking? Clear or meconium stained? • Is BOW intact or ruptured? **BE CAREFUL NOT TO RUPTURE THE BAG OF WATER IF THE PRESENTING PART IS FLOATING OR NOT ACCESSIBLE DETERMINE THE PRESENTING PART • What is the presentation? – Cephalic: Feels hard. Sutures and fontanelles of the baby’s head are felt – Malpresentation: Hardness of the baby’s head is not felt but soft buttocks or extremeties (foot or hand). • Is the cord palpable? • What is the level of the presenting part? PELVIC ARCHITECTURE Assess the following: 1. Sacral curvature : hollow (deep), average (normal), or flat (shallow) 2. Sacrosciatic notch – wide or narrow 3. Ischial spines – sharp/prominent 4. Pubic arch – estimate the angle of the rami at the pubis: narrow ( <), medium (about 90°) or wide (>90°) POGS MDG COUNTDOWN: Capacity Enhancement Program for Midwives 2010 20 5. The diagonal conjugate (from the lower border of the symphysis pubis to the promontory of the sacrum) The pelvis in UNLIKELY to be contracted when: • The diagonal conjugate is ≥ 11.5 – 12 • The sacrum is not flat cm. • The subpubic angle is not narrow • The pelvic sidewalls are parallel • The ischial spines are not prominent INTRAVENOUS FLUID (IVF) INSERTION 1. PREPARE MATERIALS TO BE USED a. Bottle or bag of IV fluid: D5LR or NSS b. IV needle/cannula/catheter: Gauge 18 or G20 c. IV tubing or administration set d. Tourniquet e. Cotton balls with alcohol f. Tape g. Disposable gloves 2. PREPARE FOR IVF INSERTION a. Check the patient identification b. Explain in simple terms the procedure to the patient and make her comfortable c. Organize correct and adequate lighting d. Wash hands to prevent infection or cross-contamination e. Wear protective gloves f. Place yourself in a comfortable position; sitting, if possible 3. PREPARE IV ADMINISTRATION SET a. Check the type, clarity, and expiration of fluid. b. Remove the plug or protective covering from the bottom of the bag/bottle. Close the flow regulator, remove protective covering from the spike of tubing set, and insert the spike into the port of fluid bag or bottle. POGS MDG COUNTDOWN: Capacity Enhancement Program for Midwives 2010 21 c. Place the fluid bag or bottle higher, squeeze the drip chamber to fill 1/3 of it, open the flow regulator to flush the air (and bubbles) from the rest of the tubing, and close the flow regulator. d. Hang the bag on an IV pole. Care should be taken not to contaminate the end of the tubing. 4. CHOOSE THE SITE OF INSERTION Alternate: Forearm veins Preferred: Hand veins AVOID o Areas of joint flexion o Veins close to arteries and deep lying vessels o Small, visible but impalpable superficial veins o Veins irritated by previous use Use distal veins first Use vein on opposite side to the site of intended procedure 5. PERFORM THE VENIPUNCTURE a. Apply a tourniquet above the chosen site to create an adequate venous filling. b. Ask patient to make a fist to maximize vein engorgement. c. Palpate the vein or tap it to help it dilate. d. Clean the entry site with alcohol and allow it to dry. e. Do not repalpate f. Insert the IV catheter into the skin at 3045º angle with the bevel up and in the direction of the vein. g. Advance the catheter to enter the vein until blood is seen in the “flash chamber” of the catheter POGS MDG COUNTDOWN: Capacity Enhancement Program for Midwives 2010 22 h. Advance the plastic catheter on into the vein while leaving the needle stationary. i. Apply gentle pressure over the vein just proximal to the entry site to prevent blood flow and remove the needle from the plastic catheter. j. Connect the plastic catheter to the previously-prepared IV tubing set and open the flow regulator k. Tape the catheter in place and adjust the flow rate. 6. COMPLICATIONS OF IV THERAPY a. Hematoma b. Infiltration (pain, swelling, pallor of site, IV flow rate decreases or stops, absence of backflow of blood into the tubing) c. Thromboembolism d. Air embolism e. Phlebitis and septicemia f. Fluid overload g. Hematoma h. Infiltration (pain, swelling, pallor of site, IV flow rate decreases or stops, absence of backflow of blood into the tubing) i. Thromboembolism j. Air embolism k. Phlebitis and septicemia l. Fluid overload POGS MDG COUNTDOWN: Capacity Enhancement Program for Midwives 2010 23 PERINEAL REPAIR Perineal tears or lacerations are injuries or tears in the vaginal canal and the outlet that occurs during delivery of the baby. The areas affected by perineal tears are the perineum, lateral vaginal walls, areas adjacent to the clitoris, lateral sulcus tear and others. Basic Instruments and supplies 1. Needle holder 2. Tissue forcep 3. Scissors 4. Hemostat 5. Gloves 6. Suture material with needle 7. Lidocaine 1 or 2 % 8. Syringe with needle 9. Gauze sponge 10. Antiseptics Basic Principles in Repairing Lacerations 1. Adequate hemostasis 3. Use minimum suture material 2. Anatomical restoration 4. Adequate anesthesia Classification of Lacerations 1st degree – involving the fourchette, perineal skin and vaginal mucous membrane 2nd degree laceration fourchette, perineal skin and vaginal mucous membrane PLUS the fascia and muscles of the perineal body POGS MDG COUNTDOWN: Capacity Enhancement Program for Midwives 2010 24 3rd degree laceration - fourchette, perineal skin and vaginal mucous membrane, the fascia and muscles of the perineal body PLUS the anal sphincter 4th degree laceration extends through the rectal mucosa exposing the lumen of the rectum Different Techniques of Suturing 1. Continuous suture technique – to repair subcutaneous fascia 2. Interrupted suture – to repair fascia and muscle 3. Lock suture – to repair vaginal wall Choice of Suture Material • Must be absorbable: Chromic 2-0, Polyglocolic derivative (Vicryl, Dexon) • Preferably with needle attached to it (atraumatic) Choice of Needle 1. Round – soft tissues like mucosa and muscles 2. Cutting – tougher tissues like fascia and skin POGS MDG COUNTDOWN: Capacity Enhancement Program for Midwives 2010 25 Steps in Perineal Repair 1. Provide emotional support and encouragement. 2. Ask an assistant to massage the uterus and provide fundal pressure. 3. Carefully examine the vagina, perineum and cervix 4. If the tear is long and deep through the perineum, inspect to be sure there is no third or fourth degree tear: a. Place a gloved finger in the anus; b. Gently lift the finger and identify the sphincter; c. Feel for the tone or tightness of the sphincter. d. Change to clean, high-level disinfected gloves. e. If the sphincter is injured → REFER f. If the sphincter is not injured, proceed with repair 5. Clean area with antiseptic solution. 6. Apply firm pressure on bleeding areas. Clamp and ligate bleeders 7. Infiltrate site with local anesthetic. Technique of Infiltration with Local Anesthetic Make sure there are no known allergies to lidocaine or related drugs. Use 10 or 20cc syringe with gauge 22, 3 cm needle Fill with lidocaine 2% Insert the whole length of the needle below the skin Aspirate (pull back on the plunger) to be sure that no vessel has been penetrated. If blood is returned in the syringe with aspiration, remove the needle. Recheck the position carefully and try again. Never inject if blood is aspirated. The woman can suffer convulsions and death if IV injection of lidoocaine occurs. Inject evenly as you withdraw the syringe. Infiltrate beneath the vaginal mucosa, beneath the skin of the perineum and deeply into the perineal muscle using about 10 mL 2% lidocaine solution. Note: At the conclusion of the set of injections, wait 2 minutes and then pinch the area with forceps. If the woman feels the pinch, wait 2 more minutes and then retest 8. Close the vaginal mucosa using continuous interlocking or simple interrupted 2-0 suture (Fig A): Start the repair about 1 cm above the apex (top) of the laceration. Place each stitch about 1 to 1.5 cm from the last. Dark purple lines are blood vessels, avoid these! Continue the suture to the level of the vaginal opening; At the opening of the vagina, bring together the cut edges of the vaginal opening; Bring the needle under the vaginal opening and out through the incision and tie. POGS MDG COUNTDOWN: Capacity Enhancement Program for Midwives 2010 26 Stitches should include the same amount of tissue from each side. If the edges roll, this means that too much tissue has been taken into that stitch or that the stitch is being pulled too tight. This can lead to a gaping scar if not corrected. 9. Close the perineal muscle using interrupted 2-0 sutures (Fig B). The perineal muscles may be differentiated from the skin layers by feel. The muscles are tougher and more resistant to touch. The color of muscles are reddish hue. Place the first muscular stitch close to the top of the vagina. At the level of the hymenal ring, the separated ends of the bulbocavernousus muscle are reunited. This muscle is rarely torn. It is almost always cut in giving an episiotomy. The "figure of eight" suture may also be used to repair. If not done properly, the mouth of the vagina will gape. If it is sewn tight, intercourse may be painful. Check to be sure the plane of the needle is at right angles to the plane of the holder. The needle holder must be held parallel with the wound edges, otherwise a puncture of the rectum may occur. 10. Close the skin using interrupted (or subcuticular) 2-0 sutures (Fig C) starting at the vaginal opening. If the tear was deep, perform a rectal examination. Make sure no stitches are in the rectum. Technique and Tips in Perineal Repair 1. Repair lacerations in layer. 2. Close the deeper perineal tissues with interrupted sutures. 3. Use small caliber sutures (Chromic 2-0) 4. Avoid tying the sutures too tight. 5. Check the rectal lumen after repair. A rectal exam should be performed to check if any of these stitches have been accidently put through into the rectum. If so, they must be removed. Removal will help prevent infection as well as a formation of an open sinus tract from perineum to rectum. 6. Remove the gauze when finished. 7. Clean the area before and after repair. POGS MDG COUNTDOWN: Capacity Enhancement Program for Midwives 2010 27 After Perineal Repair: Wash the perineal area with antiseptic solution, pat dry the area, clean away all soiled linen and position a sterile sanitary pad over the vulva and perineum. Dispose of all bloody linens in a closed or closeable container for transport to laundry Gently lay the woman’s legs down together at the same time, and make her comfortable. Make sure she is not wet or cold. Always maintain privacy and modesty. Postpartum Care of Wound 1. Advise the woman to clean the genital area including the suture line, with clean water twice daily, and always after defecation. Change perineal pads/cloths frequently enough to prevent unpleasant odor. 2. Provide pain relief: Give analgesics, Warm compress to lessen the edema, Hot sitz bath, Medicinal / Herbal wash 3. If a woman has excessive pain in the days after a repair, she should be examined immediately because pain is a frequent sign of infection in the perineal area At the Postpartum Visit 4. Examine the sutured perineum for healing and any signs of infection, e.g. marked inflammation, excessive swelling, pus. 5. If the wound becomes infected: REFER POGS MDG COUNTDOWN: Capacity Enhancement Program for Midwives 2010 28 POSTPARTUM CARE STEPS TO FOLLOW IN POSTPARTUM CARE 1. Assess for emergency signs. – Vaginal bleeding - Pallor – Fever - Looks very ill * Do not make a very sick woman wait, attend to her immediately. 2. Make the woman comfortable. Assess: When, where delivered How are you feeling? Pain, fever, bleeding since delivery? Hard to void urine? Family Planning? Other concerns? Check records: complications, treatment during delivery? HIV Status Examine BP, T°, Pulse rate Check breast Feel uterus: Is it hard, round? Look at vulva & perineum for: tear, swelling, pus Look at pad for bleeding and lochia: does it smell? Profuse? Look for pallor 3. Assess breastfeeding Is there any difficulty breastfeeding? Observe how mother breastfeeds for at least 4 minutes. - Is baby positioned well? - Is baby able to attach to the nipples well? - Is baby sucking effectively? ROUTINE POSTPARTUM CARE Mother feels well BP, pulse & temperature normal No breast problems, breastfeeding well Uterus well contracted No problem with urination No pain or other concern Give any treatment or prophylaxis due Iron Vitamin A Tetanus Advise and Counsel Health education Schedule return visit ABNORMALITIES IN THE POSTPARTUM PERIOD Elevated BP Pallor Vaginal Bleeding Foul smelling lochia Dribbling Urine REFER! Pus or perineal pain Feeling unhappy Vaginal discharge Breast Problem Infection/ Breast abscess Sore or cracked nipple Engorgement Insufficient milk Cough or breathing difficulty POGS MDG COUNTDOWN: Capacity Enhancement Program for Midwives 2010 29 TREATMENT AND PROPHYLAXIS 1. Prevent anemia with iron/folate supplementation. 2 tablets of iron/folate daily for 2 months (or more if mother is pale) 2. Give one capsule Vitamin A (200,000 IU) if none was given postpartum --- to protect the baby from nutritional blindness and infections. ADVISE AND COUNSEL 1. Postpartum care and hygiene – Wash hands before handling baby – Wash perineum daily – Have enough rest and sleep – Avoid sexual intercourse until perineal wound heals. 2. Nutrition – Eat a greater amount and variety of healthy foods – Spend more time on nutrition counseling with thin women and adolescents. ENCOURAGE BREASTFEEDING – Importance, benefits and management of breastfeeding – Teach correct positioning and attachment for breastfeeding – Support exclusive breastfeeding for the first 6 months of life – Encourage breastfeeding on demand. Avoid supplementary feeds BIRTHSPACING AND FAMILY PLANNING Counsel on importance of family planning Inform about all contraceptive choices in postpartum period Facilitate free informed choice for all women Reinforce that non-hormonal methods (LAM, barrier methods, IUD and sterilization) are best options for lactating mothers Discuss other method options for the breastfeeding & non-breastfeeding woman IMPORTANCE OF FAMILY PLANNING A woman who is not exclusively breastfeeding can become pregnant as soon as 4 weeks after delivery if she has sex. Method options for non-breastfeeding woman Immediately postpartum: Condoms, IUD, BTL Progestogen only OCP and injectables Delay 3 weeks: Combined OCP/injectables Natural family planning Method options for breastfeeding woman Immediately postpartum: LAM, Condom, BTL, IUD Delay 6 weeks: Progestogen only oral contraceptives and injectables (DMPA) Delay 6 months: combined OCP, Natural family planning SCHEDULE RETURN VISITS All postpartum women should have at least 2 routine postpartum visits. 1st visit: 1st week postpartum, preferably within 48 -72 hours. 2nd visit 6 weeks postpartum Women who do not return for postpartum visits should be visited at home. POGS MDG COUNTDOWN: Capacity Enhancement Program for Midwives 2010 30 COMPLICATIONS OF PREGNANCY OBSTETRIC EMERGENCIES I. PRE-ECLAMPSIA Diagnostic criteria 1. Hypertension after 20 weeks (Diastolic BP more than 90 mm Hg) 2. Proteinuria 1+ 1. Risk factors for pre-eclampsia 1. Primigravid 6. Women with 2. Young teens Diabetes 3. Women > 35 years H Mole 4. Obese Essential or renal HPN 5. Multiple Pregnancy Family hx of HPN 2. Danger signals 1. Massive pitting pedal edema (generalized swelling) 2. Severe headache 3. Epigastric pain 4. Vomiting 5. Visual disturbance or blurring of vision 3. Complications of severe pre-eclampsia 1. Small baby (IUGR) 2. Stillbirth 3. Abruptio Placenta 4. HELLP syndrome 5. Eclampsia ECLAMPSIA Convulsions in a woman with pre-eclampsia Convulsions may occur • in pregnancy after 20 weeks AOG, • in labor • during the first 48 hours postpartum. Effects on Mother • Respiratory – pulmonary edema • Heart Failure • Cerebral vascular accidents • Acute kidney failure • Liver necrosis • HELLP syndrome • Visual disturbance • Injuries during convulsion Effects on fetus Small babay Stillbirth POGS MDG COUNTDOWN: Capacity Enhancement Program for Midwives 2010 31 Reducing the Risk of Eclampsia • Pregnant women should come for ANC early – take baseline BP • Regular antenatal visits especially in the 3rd trimester • Measure BP at each ANC visit and check urine for protein if diastolic BP>90 mm Hg. • REFER if proteinuria develops • Counsel woman and family about danger signals of severe preeclampsia What to do when seizures occur • Call for medical help • As soon as possible, clear airway and or give oxygen at 4–6 L/min. • Position the woman on her left side to reduce the risk of aspiration of secretions, vomit and blood • Stay with woman and protect her from injury but do not restrain her Immediately after the convulsion • Set up IVF – run at slow rate • Monitor BP, pulse, respiration, level of consciousness. Record. • Insert urinary catheter to monitor urine output and test for protein. • Arrange for referral During the transport • Put mother in any flat or low surface to prevent from falling during ambulation. • Observe proper maternal positioning and least stimulation during transport. • Never leave alone II. VAGINAL BLEEDING IN DURING PREGNANCY Assess the PREGNANCY STATUS i. EARLY PREGNANCY – uterus is below the umbilicus ii. LATE PREGNANCY – uterus above umbilicus Assess the AMOUNT OF BLEEDING i. HEAVY – pad or cloth is soaked in less than 5 minutes ii. LIGHT Assess for alert signs and symptoms REFER! 1. Fainting 2. History of expulsion of tissues 3. Cramping/lower abdominal pain 4. Tender uterus 5. Tender mass 6. Uterus soft and larger than expected for AOG POGS MDG COUNTDOWN: Capacity Enhancement Program for Midwives 2010 32 Provide initial treatment Pregnancy Status Amount of Bleeding Early pregnancy – uterus below umbilicus HEAVY (pad soaked in 5 minutes or less), or with alert signs This may be abortion, ectopic pregnancy or molar pregnancy. LIGHT, no alert signs Late – uterus above the umbilicus This may be placenta previa or abruptio placenta Any bleeding is dangerous! Assess for alert symptoms: Treatment • • • • • • Reassure the woman Insert IV line IV fluids Monitor vital signs REFER If the woman is bleeding HEAVILY and referral center is far, give 0.2 mg ergometrine IM • • • • Reassure Give iron/folate Review emergency plan Follow up after 2 weeks • • • • DO NOT perform IE! Insert IV line Monitor vital signs Reassure the woman, make her comfortable REFER • PLACENTA PREVIA Abnormal implantation of the placenta at the lower uterine segment Classic Sign: Painless vaginal bleeding Uterus is soft, non-tender, with or without contractions, fetus is palpable. RISK FACTORS 1. Maternal age > 35 years old 2. Previous cesarean section 3. Multiparity 4. Previous placenta previa 5. History of uterine surgery, multiple abortions, D&C 6. Cigarette smoking 7. Large placenta in multiple gestation ABRUPTIO PLACENTA Separation of a normally implanted placenta from the uterus before childbirth. UTERUS is HYPERTONIC or TENSE and TENDER on PALPATION ABDOMEN – “BOARD-LIKE RIGIDITY“ 1. Maternal Hypertension, Pre-eclampsia, Chronic hypertension 2. Maternal age 3. Multiparity 4. Cigarette smoking. 5. Maternal trauma 6. Polyhydramnios 7. Poor nutrition POGS MDG COUNTDOWN: Capacity Enhancement Program for Midwives 2010 33 III. PRE-LABOR RUPTURE OF MEMBRANES Rupture of the bag of water prior to the onset of labor a. PROM when fetus is > 37 weeks b. Preterm PROM (PPROM) when fetus is less than 37 weeks • • • • Diagnosis: ASK when did membranes rupture? LOOK at pad for evidence of amniotic fluid or foul smelling vaginal discharge. • If no evidence, ask her to wear a pad and check again in one hour. Measure temperature Routine vaginal examination is NOT recommended – increase risk of infection WHAT TO DO If (+) fever >38°C Foul smelling vaginal discharge No labor Rupture membranes at <8 months of pregnancy IV. Rupture of membranes at >8 months pregnancy Manage as woman in childbirth Give antibiotic (Ampicillin 2 grams) REFER to hospital PRETERM LABOR Definition Labor before 8 completed months of pregnancy ; more than 1 month before estimated date of birth between 24 – 34 weeks gestation Signs and symptoms 1. Contractions 2. Watery vaginal discharge 3. Vaginal bleeding 4. Low dull backache What to do 1. Establish AOG 2. Evaluate contractions 3. Assess cervix Sterile speculum examination Digital examination* 4. Stabilize woman and fetus 5. If woman is lying, encourage her to lie on her left side 6. Check vital signs especially BP 7. If BP is normal and no heart problem: Give Nifedipine 10mg tablet orally (not under the tongue) every 6 hours until she reaches a CEmONC facility Give Dexamethasone 6mg intramuscularly every 12 hours until she reaches a CemONC facility ( up to a total of 4 doses) 8. Facilitate transfer the hospital with neonatal and obstetrical care POGS MDG COUNTDOWN: Capacity Enhancement Program for Midwives 2010 34 V. PROLONGED LABOR Causes of prolonged labor 1. Cephalopelvic disproportion: small or contracted pelvis or large fetus 2. Abnormal presentations (e.g. brow, shoulder associated with transverse lie) 3. Malposition of the fetus 4. Fetal abnormalities, e.g. hydrocephalus, encephalocele, locked twins 5. Abnormalities of the reproductive tract Effects of Prolonged Labor Maternal Infection Uterine rupture Genital fistulas Maternal Death Fetal Infection Asphyxia and traumatic injury to the baby Stillbirth Neonatal death Prolonged Latent Phase o Diagnosis is made retrospectively If contractions cease, the woman is in FALSE LABOR o If cervix dilated less than 4 cm for more than 8 hours, reassess If no sign of infection: may be observed further provided maternal and fetal status are good. If with sign of infection: give antibiotics Ampicillin 2 grams p.o. and refer Prolonged Active Phase o Cervix does not dilate 1 cm per hour o Recognize slow progress of labor with a partograph: cervical dilatation to the right of the alert line. o May be due to 1. Poor uterine contractions 2. Malposition or malpresentation 3. Disproportion between fetal size and pelvic size o Reassess uterine contractions o If less than 3 contractions in 10 minutes, each lasting less than 40 seconds, suspect inadequate uterine activity and refer to higher level care o If contractions are efficient (3 contractions in 10 minutes, each lasting more than 40 seconds), suspect cephalopelvic disproportion, obstruction, malposition or malpresentation o REFER to higher level care. Before Transfer o Start IV infusion to rehydrate o Give antibiotics o Give supportive care* o Monitor maternal and fetal condition o Ensure referral letter is completed and make transportation arrangements. Contact the referral center to advise them of transfer. POGS MDG COUNTDOWN: Capacity Enhancement Program for Midwives 2010 35 Supportive Care o Make the patient comfortable. o Encourage companion to rub the woman’s back, wipe her face and brow with a wet cloth, assist her to move about o Explain all procedures to the woman, seek permission and discuss findings with her o Encourage her to empty her bladder regularly o Encourage breathing techniques. VI. SHOULDER DYSTOCIA Predisposing Factor Maternal Abnormal Pelvic Anatomy Gestational Diabetes Post-term pregnancy Previous shoulder dystocia Maternal obesity Short stature FETAL o Suspected macrosomia LABOR RELATED o Assisted vaginal delivery o Protracted active phase of 1st stage labor o Protracted second stage labor Diagnosis: TURTLE SIGN o Fetal head is delivered but remains tightly applied to the vulva o Chin retracts and depresses the perineum Avoid 4Ps o Pull o Push o Panic o Pivot Management of Shoulder Dystocia o A – Ask for help (from the woman’s husband or labor companion, other healthcare providers. Prepare for resuscitation of the baby.) o L– lift/hyperflex legs o A – anterior shoulder disimpaction o R – rotation of posterior shoulder o M – manual removal of posterior arm o E – episiotomy o R – roll over onto “all fours” POGS MDG COUNTDOWN: Capacity Enhancement Program for Midwives 2010 36 McRobert’s Maneuver – Flex woman’s legs sharply on her abdomen Suprapubic pressure is applied with the heel of clasped hands from the posterior aspect of the anterior shoulder to dislodge it. ROTATION OF THE POSTERIOR SHOULDER • Place the hand behind the posterior shoulder of the fetus. • Rotate the posterior shoulder 180 degrees in a corkscrew manner so that the impacted anterior shoulder is released. MANUAL REMOVAL OF THE POSTERIOR ARM Arm is flexed at the elbow. Hand is grasped and swept across the chest and delivered. POGS MDG COUNTDOWN: Capacity Enhancement Program for Midwives 2010 37 ROLL OVER ON ALL FOURS After shoulder dystocia 1. Remember the SIGNIFICANT risk of maternal injury (tears) and postpartum hemorrhage 2. Actively manage the third stage 3. Inspect for and repair 1st or 2nd degree tear or lacerations 4. Resuscitate the baby, examine for evidence of trauma 5. Explain to the woman and all those involved in the delivery exactly what occurred and what were done 6. Record Duration of attempts to resolve dystocia Maneuvers performed Condition of baby at delivery, description of injuries, bruises Time from delivery of fetal head to delivery of the body Documentation of the discussion with woman/relatives VII. UMBILICAL CORD PROLAPSE Umbilical cord lies in the birth canal below the presenting part Cord is visible at the vagina following rupture of membranes General management: o Give oxygen at 4-6 liters per minute by mask or nasal cannula If Cord is pulsating – fetus is alive o Diagnose stage of labor o Wear high level disinfected gloves. Insert hand into the vagina and push presenting part up to decrease pressure on the cord dislodge presenting part from the pelvis. o Place other hand on the abdomen in the suprapubic region to keep the presenting part out of the pelvis o REFER If cord is not pulsating – baby is dead o Give supportive care to the woman o Attempt vaginal delivery POGS MDG COUNTDOWN: Capacity Enhancement Program for Midwives 2010 38 VIII. POSTPARTUM HEMORRHAGE • Recognizing postpartum hemorrhage o Bleeding >500 ml after childbirth o Pad or cloth soaked in less than 5 minutes o Constant trickling of blood OR o Delivered outside health center and still bleeding • What to do: o Call for extra help o Massage uterus until it is hard and give OXYTOCIN 10 units IM o Give IV fluids with 20 units oxytocin at 60 drops per minute o Empty the bladder: catheterize if necessary o Check and record BP and pulse every 15 minutes o Establish cause of bleeding • Causes of postpartum hemorrhage o Uterine atony o Tears of the cervix, vagina, or perineum o Retained placenta o Retained placental fragments o Inverted uterus o Ruptured uterus • Check if placenta is delivered. Placenta is not delivered o When uterus is hard, deliver placenta by controlled cord traction o If unsuccessful and bleeding continues – remove placenta manually and check placenta o Give appropriate IM/IV antibiotics o If unable to remove placenta – REFER urgently to hospital o During transfer, continue IV fluids with 20 units oxytocin at 30 drops/minute Placenta is delivered o Check placenta o If placenta complete Massage uterus to express any clot If uterus remains soft, give OXYTOCIN 10 units IM Continue IV fluids with 20 units Oxytocin at 30 drops/min Continue uterine massage until it is hard o If placenta is incomplete or not available for inspection: Refer woman urgently to hospital o Placenta is complete and vaginal bleeding continuous: o POGS MDG COUNTDOWN: Capacity Enhancement Program for Midwives 2010 39 HOW TO MAKE PROPER REFERRALS Referral must be TIMELY STEPS TO FOLLOW: 1. Give emergency treatment. 2. Discuss decision with woman, partner/spouse and relatives. Explain why patient is advised to transfer. 3. Help arrange transport of patient. 4. Inform the referral center by mobile phone, landline or radio. 5. Ensure support. 6. Always send a referral letter with the patient. The referral must state the following: Date and time; Emergency or Non-emergency Problems identified Findings and action taken. 7. If the hospital is far away (> 1 hour trip), Give appropriate treatment on the way. Continue to monitor patient Record all findings & treatment given. 8. A relative or friend should accompany the patient → help look after the woman during the journey. 9. Do not delay. Go straight to the hospital. POGS MDG COUNTDOWN: Capacity Enhancement Program for Midwives 2010 40 References: POGS CLINICAL PRACTICE GUIDELINES ON NORMAL LABOR AND DELIVERY, 2nd edition, November 2009 POGS CLINICAL PRACTICE GUIDELINES ON THIRD TRIMESTER BLEEDING AND POSTPARTUM HEMORRHAGE ALARM INTERNATIONAL (A Program to Reduce Maternal and Neonatal Mortality and Morbidity), The Society of Obstetricians and Gynecologists of Canada, 4th edition. Integrated Management of Pregnancy and Childbirth. Pregnancy, Childbirth, Postpartum and Newborn Care: A guide for essential practice in Philippine Setting. Adapted from the World Health Organization by the Department of Health. Community-Managed Maternal and Newborn Care: A Guide for Primary health Care Professionals. Department of Health, San Lazaro Manila, 2006 Barbara Kinzie and Patricia Gomez, Basic Maternal and Newborn Care: A Guide for Skilled Providers, JHPIEGO, 2004 Midwives Manual on Maternal Care. Maternal and Child Health Service, Department of Health, San Lazaro Manila. 2000 Newborn Care Until the First Week of Life: Clinical Practice Pocket Guide WHO 2009 WHO Pregnancy Child Birth, Postpartum, Newborn care: A Guide for Essential Practice in Philippine Setting, Manila 2003 Prepared by the POGS MDG COUNTDOWN TASK FORCE 2010 POGS MDG COUNTDOWN: Capacity Enhancement Program for Midwives 2010 41 CARE OF THE NEWBORN MDG 4: Reduce child mortality Target: Reduce by two thirds, between 1990 and 2015, the under-five mortality rate More than 10 million children under five die every year. Almost 90% of all child deaths are attributable to just six conditions (WHO) 1. neonatal causes 2. Pneumonia 3. Diarrhea 4. Malaria 5.Measles 6. HIV/AIDS. MDG to reduce child mortality requires: •Universal coverage with key effective, affordable interventions: 1. care for newborns and their mothers 2. infant and young child feeding 3. Vaccines 4. prevention and case management of diarrhoea 5. pneumonia and sepsis 6. malaria control 7. Prevention and care of HIV/AIDS In countries with high mortality, these interventions could reduce the number of deaths by more than half. WHO promotes three main strategies: 1. integrated management of childhood illness 2. expanded programme on immunization 3. infant and young child feeding. •Attention to newborn health is being increasingly incorporated into each of these delivery strategies, complemented by interventions aimed at making pregnancy safer. Newborn Mortality Health statistics show that worldwide: »About 4 million babies die each year. »Another 4 million babies each year are stillborn; most die in late pregnancy or labor. »Most newborn deaths occur in developing countries. The “Two Thirds” Rule •Two thirds of infant deaths occur in the first month of life •Of those, two thirds die in the first week of life •Of those, two thirds die in the first 24 hours of life Newborn Survival “Most newborn deaths are entirely preventable, which are attributed to a number of simple, low-cost actions that can be taken by health care workers, mothers, and families.” POGS MDG COUNTDOWN: Capacity Enhancement Program for Midwives 2010 42 Immediate Essential Newborn Care Objectives •To describe and carry out the evidence based routine care of a newborn baby at the time of birth and prevent complications. Basic needs of a baby at birth •To breathe normally •To be warm •To be protected •To be fed Preparing to Meet the Baby’s Needs “Good care of the newborn begins with good preparation” Preparing to Meet the Baby’s Needs at birth 1. Warm delivery room 25-28C, draft free 2. Two clean and warm towels or cloth 3. Newborn size self inflating bag and masks in two sizes: normal and small newborn 4. Suction device 100 mmHg pressure 5. Rolled up piece of cloth 6. Clean dry warm surface STANDARD PRECAUTIONS Always remember the importance of observing precautions to help protect the mother and baby and ourselves from infections with bacteria, viruses including HIV Wear 2 sets of sterile gloves Steps : Immediate Essential Newborn Care • Call out time of birth. • Deliver the baby prone on the mother’s abdomen. • Dry the newborn thoroughly for a full 30 seconds.* Remove wet cloth. • Check breathing while drying. • Position newborn prone on the mother’s abdomen in skin-to-skin contact. Cover the back with a dry blanket. – If this is not possible, place newborn in a warm, safe place close to the mother. • Exclude second baby • Wait for cord pulsation to stop (approx 1-3min) • Remove first set of gloves • Clamp cord at 2cm away from newborn skin using sterile plastic cord clamp and apply sterile forceps 5cm away from the skin then cut the cord • Maintain skin-to-skin contact; do not separate baby from the mother until a full breastfeed; watch for feeding cues. • Place identification band on ankle. • Give eye prophylaxis within the first hour .Delay Vit K and immunization until after 90min of uninterrupted skin to skin contact POGS MDG COUNTDOWN: Capacity Enhancement Program for Midwives 2010 43 •Drying the newborn – Stimulates the newborn to breathe normally – Minimizes heat loss When drying the newborn, Dry the body and the head well Remove wet cloth Wrap the baby in clean dry cloth covering the head Do not remove the vernix!!! WHO emphasizes thermal care of the newborn as an essential intervention Thermal care is a priority behavior in the Mother-Infant Package of interventions in developing countries. Skin-to-Skin Contact (SSC) Provides warmth Improves bonding Provides protection from infection by exposure of the baby to good bacteria of the mother Increases the blood sugar of the baby Non-immediate clamping of the umbilical cord Allows the newborn to get a free blood transfusion from the placenta Reduces the risk of anemia in both term and preterm babies Reduces the risk of transfusions and intraventricular hemorrhage in preterms Initial Cord care Do not apply any substance to the stump Do not bind or bandage the stump Leave the stump uncovered Assessing the baby During the first hour after complete delivery of the placenta the baby (and the mother) should be monitored every 15 minutes. After the cord is cut, assess the baby for any signs of illness, eg. chest indrawing If the baby is doing well, continue skin-to-skin contact and provision of warmth Monitor the mother and baby Never leave the woman and newborn alone Keep the mother and baby in the delivery room Record findings, treatments and procedures in the labor record Monitor every 15 minutes: o Breathing: listen for grunting, look for chest in-drawing and fast breathing. o Warmth: check to see if feet are cold to touch. POGS MDG COUNTDOWN: Capacity Enhancement Program for Midwives 2010 44 Washing should be delayed until after 6 hours • Washing exposes to hypothermia • The vernix is a protective barrier to bacteria such as E. coli and Group B Strep • Washing removes the crawling reflex Initiation of breastfeeding To begin with the baby will want to rest. Every baby is different and the rest period may take from a few minutes to 30 or 40 minutes before the baby shows signs of wanting to breastfeed. Help the mother and baby into a comfortable position Only once the newborn shows feeding cues (e.g. opening of mouth, tonguing, licking, rooting), make verbal suggestions to the mother to encourage her newborn to move toward the breast e.g. nudging. Health workers should not touch the newborn unless there is a medical indication. Do not give sugar water, formula or other prelacteals. Do not give bottles or pacifiers. Do not throw away colostrum. If the mother is HIV-positive, counsel the mother on breastfeeding SKIN TO SKIN CONTACT & BREASTFEEDING Initiate breastfeeding within the first hour after birth To help a baby successfully breastfeed after birth, we should: –Give the baby to the mother for skin-to-skin contact –Let the baby feed when he is ready: Signs of readiness to breastfeed: –Baby looking around –Mouth open –searching Counsel on positioning and attachment When the baby is ready, tell the mother to: Make sure the newborn’s neck is not flexed nor twisted. Make sure the newborn is facing the breast, with the newborn's nose opposite her nipple and chin touching the breast. Hold the newborn's body close to her body. Support the newborn’s whole body, not just the neck and shoulders. Wait until her newborn’s mouth is opened wide. Move her newborn quickly onto her breast, aiming the infant's lower lip well below the nipple Signs of good attachment and suckling: Mouth wide open Lower lip turned outwards Baby's chin touching breast More areola is visible above the baby’s mouth Sucking is slow, deep with some pauses *If the attachment or suckling is not good, try again and reassess. POGS MDG COUNTDOWN: Capacity Enhancement Program for Midwives 2010 45 The first breast feed –Check attachment and positioning when the baby is feeding –Let the baby feed for as long as he wants on both breasts –Keep the mother and baby together for as long as possible after delivery –Delay tasks such as weighing, washing, eye care, injections, etc. until after the first feed If the baby does not feed in 1 hour, examine the baby. If healthy, leave the baby with the mother to try later. Assess in 3 hours, or earlier if the baby is small If the mother is ill and unable to breastfeed, help her to express breast milk and feed the baby by cup If unable to initiate breastfeeding, plan for alternative feeding method If mother HIV+ and chooses replacement feeding, feed accordingly Eye Care Wipe the eyes Apply an eye antimicrobial within 1 hour of birth: o 1% silver nitrate drops or 2.5% povidone iodine drops or 1% tetracycline ointment or erythromycin eye drops Do not wash away the eye antimicrobial Administer: Vitamin K - IM upper outer quadrant (vastus lateralis) of the thigh. - 0.5 mg preterm baby - 1.0 mg term baby Hepatitis B Vaccine. 0.5 ml IM on the upper outer quadrant (vastus lateralis) of the thigh BCG 0.05 ml Intradermal on the deltoid area Summary: WHO emphasizes thermal care of the newborn as an essential intervention “Warm Chain” a draft-free, warm room (at least 25 o C); immediate drying of the newborn; skin-to-skin contact on the mother’s abdomen/chest for all care, covered, for at least 2 hours after birth; helping the mother to breastfeed within one hour of birth; postponement of bathing for at least 6, but preferably 24 hours; dressing in warm clothing. POGS MDG COUNTDOWN: Capacity Enhancement Program for Midwives 2010 46 HIV and Newborn care at birth If the mother has HIV/AIDS: Universal precautions must be followed as with any other delivery and after care. Her baby can have immediate skin-to-skin contact Breastfeeding can begin when the baby is ready after delivery Do not give the baby any other food or drink Good attachment and positioning are vital If replacement feeding, prepare formula for the mother for the first few feeds In the first two hours after birth, do the following after skin-to-skin and initiation of breastfeeding: 1. Weigh or measure the baby 2. Bath the baby 3. Dress the baby 4. Eye care, Vit. K and Immunization Summary Make sure that the delivery area is ready for the mother and baby Observe universal precautions at all times (Protection) Keep the delivery room warm (warmth, protection) Have resuscitation equipment near the delivery bed (breathing) Have clean warm towels/cloths ready for the baby (protection, warmth) Have a sterile kit to tie/clamp and cut the cord. Apply antimicrobial to the eyes. Give Vit. K, Hepatitis B and BCG(protection) Keeping the mother and baby in skin-to-skin contact encourages early breastfeeding (warmth, feeding) NEWBORN RESUSCITATION INTERVENTION: See Algorithm on Resuscitation (p 21). ACTION: Start resuscitation if the newborn is not breathing or is gasping after 30 seconds of drying or before 30 seconds of drying if the baby is completely floppy and not breathing. Clamp and cut the cord immediately. If necessary, transfer the newborn to a dry, clean and warm surface. Keep the newborn wrapped or under a heat source if available. Inform the mother that the newborn needs help to breathe. INTERVENTION ACTION: Open airway Position the head so it is slightly extended. Introduce the suction tube: – First, into the newborn’s mouth 5 cm from the lips and suck while withdrawing. – Second, 3 cm into each nostril and suck while withdrawing. – Repeat once, if necessary taking no more than a total of 20 secs. POGS MDG COUNTDOWN: Capacity Enhancement Program for Midwives 2010 47 Notes: - Do not suction mouth and nose prior to delivery of the shoulders of babies with meconium stained amniotic fluid. K11 INTERVENTION ACTION: Ventilate, if still not breathing 1. Place mask to cover chin, mouth and nose to achieve a seal. Squeeze bag attached to the mask with 2 fingers or whole hand, according to bag size, 2 or 3 times. Observe rise of chest. If chest is not rising, reposition baby’s head If baby’s chest is still not rising, check for adequate mask seal If chest is still not rising, squeeze bag harder. If chest is rising, ventilate at 40 breaths per minute until newborn starts crying or breathing. 2. Reassess at 30-second intervals. If baby still fails to improve, check the following: Failure To Improve Checklist Face-mask seal tight? Airway clear of secretions? Head positioned properly? Is contact with the soft tissue of the infant’s anterior neck being avoided? Resuscitator working properly? Adequate pressure being used? Air distending the stomach? Air leak (pneumothorax)? 3. If baby starts crying or breathing >30 per minute and has no chest-in-drawing, stop ventilating: 4. Put the newborn in skin-to-skin contact on mother’s chest and continue care while monitoring breathing and warmth. 5. Explain the baby’s condition to the mother. If after 30 sec of effective bag/mask ventilation, the newborn is gasping/breathing < 30/min or >30/min but has severe chest in-drawing: Continue bag/mask ventilation Continue assessing at 30 sec intervals while transporting or Proceed to intubation per advanced resuscitation guidelines, if skilled personnel and equipment are available If after 20 minutes of effective ventilation, the newborn does not start to breathe or gasp at all, stop ventilating. Explain to the mother that the baby is dead, give supportive care and record the event. POGS MDG COUNTDOWN: Capacity Enhancement Program for Midwives 2010 48 Notes: While ventilating, refer and explain to the mother what happened, what you are doing and why. Ventilate, if needed, during transport Record the event on the referral form and labor record. K111DITIONAL CARE Resuscitation With Bag & Mask Self-inflating Bag: Basic Parts Bag and Mask: Equipment Masks –Rims: Cushioned or non-cushioned –Shape: Round or anatomic shape –Anatomic shape –Size: small or large Position Bag and Mask on Face. Mask should cover tip of chin, mouth and nose. Do not jam the mask down on the face Do not allow your fingers or parts of the hands to rest on the newborn’s eyes Do not put pressure on the throat (trachea) Airtight seal is essential to achieve positive pressure. Tight seal required for flow-inflating bag to inflate Tight seal required to inflate lungs when bag is squeezed How Hard to Squeeze the Bag Noticeable rise and fall of chest Bilateral breath sounds Improvement of color and heart rate Frequency of Ventilation: 40 to 60 breaths per minute If the Chest is Not Expanding Adequately: Possible causes Seal inadequate Airway blocked Not enough pressure given Signs of Improvement after Positive pressure ventilation Improving color Spontaneous breathing Increasing heart rate Post-resuscitation Care Baby requires Close monitoring Anticipatory care Laboratory studies POGS MDG COUNTDOWN: Capacity Enhancement Program for Midwives 2010 49 EXAMINATION OF THE NEWBORN BABY When should a newborn baby be examined? After birth: • At around an hour • before discharge from hospital (no discharge before 12 hours of age) • If there is maternal concern about the baby’s condition • If a danger sign observed during monitoring After leaving the hospital: • during the first week of life at a routine visit • follow-up • sick newborn visit. Why do we examine the baby at birth and again at discharge? At the time of birth: • Overall assessment of the baby’s condition • An initial set of observations • To provide appropriate care and treatment Before discharge and thereafter: • To re-assess and monitor the baby’s condition • To provide appropriate treatment if the baby’s condition changed from a previous examination • To give the mother guidance on continuing care Universal precautions: remember to wash your hands before and after examining the baby DANGER SIGNS? • History of convulsion • Difficulty feeding • Temperature of 37.5ºC and above • Temperature <35.5ºC • Movement only when stimulated • Respiratory rate of 60 breaths per minute or more • Severe chest in-drawing TREAT AND ADVISE: • Refer baby urgently to hospital • After emergency treatment, explain the need for referral to the mother/father. • Organize safe transportation. • Always send the mother with the baby, if possible. • Send referral note with the baby • Inform the referral center if possible by phone or radio. POGS MDG COUNTDOWN: Capacity Enhancement Program for Midwives 2010 50 Normal findings A baby: • passes urine six or more times a day after day 2. • May pass six to eight watery stools a day. • May have some vaginal bleeding for a few days during the first week after birth. It is not a sign of a problem. Assess Breathing • Count number of breaths taken for one full minute. • If not sure of breaths per minute, repeat count. • Look for chest in-drawing • Listen for grunting • Normal respiratory rate of a newborn baby - 30 to 60 breaths per minute. • No chest indrawing • No grunting on breathing out • Babies may breathe irregularly (up to 80 breaths per minute) for short periods of time. • Small babies (less than 2.5 kg at birth or born before 37 weeks gestation) may: –have some mild chest in-drawing –periodically stop breathing for a few seconds. Color : • Face, chest, tongue and lips are pink • Hands and feet may be bluish during the first 48 hours • Jaundice occurring on the second day lasting for about 14 days Posture and tone: •Arms and legs are well bent (flexed) •Loosely clenched fists •Flexed arms, hips and knees •Preterm babies have less flexion •Babies who were in breech position may have fully flexed hips and knees; the feet may be near the mouth; or the legs and feet are at the side of the baby Activity : •Moves both arms and legs equally •+ rooting, moro, grasp, sucking reflex Warmth: Baby’s abdomen or back or feet feels warm Heart Rate: Count the baby’s heartbeat for 1 full minute • 100 – 160 beats/min POGS MDG COUNTDOWN: Capacity Enhancement Program for Midwives 2010 51 Skin : •Milia •Mongolian spots •Peeling/desquamation •Erythema toxicum (red spots with tiny white centers) seen on the face, trunk and back on day 2 and later Head : • Molding ( usually disappears in 2-3 days after birth) • Caput succedaneum(soft swelling over the presenting part of the head (disappears after 48 hours) • Anterior fontanelle is flat and may swell when the baby cries • Anterior fontanelle is flat and may swell when the baby cries Eyes: no discharge Mouth: Lips, gums and palate are intact • Baby sucks vigorously on your finger Chest : • Moves equally with breathing • Abdomen pushes out with each breath • Breast nodules maybe enlarged (boys and girls) Abdomen : • Rounded, soft • Umbilical cord is dry, no bleeding • Small umbilical hernia is normal during the 1st year Back and spine: • Skin over the back has no openings • No defects Anus : • Patent • Baby passes stool by 24 hours Female Genitalia : • white vaginal discharge • A bloody vaginal discharge that starts on day 2-3 and continues up to day 7 Male Genitalia: • Foreskin retracted easily • Urethra opens at the end of the penis • Testes are felt in the scrotum POGS MDG COUNTDOWN: Capacity Enhancement Program for Midwives 2010 52 Temperature : • 36 - 37ºC axillary • If no thermometer, feel the chest or back with the back of your hand Weight : • 2.5 up to 3.99 kg • Weight loss of 5-10% of their birth weight in the first few days of life. Regains birthweight by 10 – 14 days of life. Weigh the Baby Why do we weigh the baby? 1. Assess weight gain 2. Provides a baseline and is part of growth monitoring 3. Indicates whether the baby is receiving adequate nutrition 4. Identifies a low birth weight baby who are at risk and needs monitoring and special care 5. For drug calculation 6. Identifies babies who have an underlying condition and needs examination and treatment How to weigh a baby : 1. Take the scales to the baby 2. Prepare the scales. Cover pan with a clean cloth 3. Preparing and weighing the baby Remove all clothing including the diaper Weigh baby naked WAIT till baby stops moving Read and record the weight Wrap the baby Return baby to the mother Scale maintenance Clean the scale pan between each weighing Calibrate daily In postnatal clinics: Weigh a baby on THE SAME SCALES at each visit Assess Breastfeeding • If the baby is breastfeeding at the time of examination, observe and assess the feed. • If the mother is not breastfeeding, ask the mother to call the health worker when the baby next wants to feed so that feeding can be observed. • Observe breastfeeding for at least five (5) minutes. POGS MDG COUNTDOWN: Capacity Enhancement Program for Midwives 2010 53 Normal findings: • Baby should breastfeed at least 8X in 24 hours (at least every 3 hours) • A low birthweight baby needs to breastfeed more often, at least every 2 to 21/2 hours. • Suckling should be vigorous and suckling well Make a plan and care for the needs and problems of the newborn • Education and counseling • Medical treatment • Referral and follow up. Abnormal findings and plan of action CHECK Color Breathing Posture and tone Skin Head ABNORMAL FINDINGS < 24 hours old with yellow skin on face >24 hours old with yellow p[alms and soles (possible infection, blood group incompatibility) Pallor (bleeding, poor circulation, cold, low blood sugar) Noisy breathing (grunting) Flaring nostrils Indrawing of the chest between ribs (Obstruction of airway, infection) RR < 30 or >60/min Apnea or gasping Limp, floppy (prematurity, birth injury, asphyxia Rigid, stiffness or arching of the back Rhythmic movements of one or both limbs (tetanus, birth injury meningitis) Pustules, blisters, red or purple spots (localized infection but may lead to sepsis if untreated Cephalhematoma (swelling on one side of the head) ACTION Refer Make sure cord tie is tight Warm the baby Check respiration Ensure breastfeeding Refer Refer Newborn resuscitation Refer Keep baby warm Give initial dose of antibiotics prior to referral Treat skin pustules: Wash hands Wash off pus and crusts with boiled and cooled water and soap Dry with a clean cloth Paint with gential violet None. the blood is slowly absorbed and disappears by 1-2 months POGS MDG COUNTDOWN: Capacity Enhancement Program for Midwives 2010 54 Eyes Discharging pus Sticky eyes Swollen eyelids ( eye infection – gonorrhea or chlamydia) Mouth Cleft lip / palate (congenital abnormality Abdomen Distended and hard ( possible intestinal obstruction) Open tissue on the abdomen ( omphalocele, gastroschisis) Abdomen Bleeding from the umbilical cord Red umbilicus or skin around it (local umbilical infection) Back and spine Open tissue on the back ( neural tube defects) External genital organs Unable to define gender Boys external genitalia No urine or wet diaper by 24 hours Urethra does not open at the end of penis but under the penis; foreskin not retractable Scrotum is empty ( no testes felt) Temp. Weight Axillary temp <36ºC or >37ºC, or Baby’s back or chest feels cooler or hotter than the skin of a normal person Weight less than 2500 grams (preterm or SGA) Refer Wash hands Wet clean cloth with cooled boiled water Use wet cloth to gently was off pus from the baby’s eyes Apply antimicrobial to eyes 4x a day Re-assess in 2 days Re-assure the mother Encourage mother to breastfeed/ feed the baby expressed breast milk by cup Refer to specialist Refer Refer Cover with sterile tissue soaked with sterile saline solution Retie the cord tightly Treat umbilical infection -wash hands -wash off pus and crusts with cooled boiled water -dry with clean cloth -paint with gentian violet Refer Cover with sterile tissues soaked with saline solution Refer Refer Explain to parents that the testes may descend Examine the baby again at 6 months Refer if the testes has not come down Refer Give first dose of antibiotics Keep the temperature normal Special care POGS MDG COUNTDOWN: Capacity Enhancement Program for Midwives 2010 55 Weight > 4000 grams (infant of diabetic mother, risk of low blood sugar Feed as soon as possible after birth Care of the newborn until Discharge Teach and counsel a mother and her family about newborn care ; What care to give Why to give the care Warmth Keep the room warm ( 25 - 28ºC) Skin-to-skin contact Dress the baby or cover with dry, clean cloth Cover the head with a cap especially if the baby is small Assess warmth - touch feet, abdomen or back Sleep At night let the baby sleep with the mother or within easy reach to facilitate breastfeeding Let the mother and baby sleep under a bed net to protect them from malaria A baby who is hard to wake up or sleeps too much may be sick Support breastfeeding Counsel on the importance of exclusive breastfeeding Encourage breastfeeding on demand day and night Do not give any other feeds or water Do not use artificial teats and pacifiers Breastfeeding Ask the mother if there is a breastfeeding problem/difficulty. If mother has breastfeeding difficulty, assess breastfeeding Teach correct positioning and attachment Key points to good attachment The baby’s mouth is widely open The tongue is far forward in the mouth, and may be seen over the bottom gum The lower lip is turned outwards The chin is touching the breast More areola is visible above the baby’s mouth than below it Problems that may arise if the baby is not well attached to the breast The baby: May cry a lot and be unhappy May be slow to gain weight, or may even lose weight POGS MDG COUNTDOWN: Capacity Enhancement Program for Midwives 2010 56 The mother: May get sore/cracked nipples May get very full breasts which feel hard, sometimes they may feel hot and may look red Key points to good positioning •The baby’s head and body are in a straight line •The baby’s face is opposite the nipple and breast •The baby’s upper lip or nose is opposite the mother’s nipple •The baby is held as close to the mother’s body as possible •The baby’s whole body is supported if the mother is in a sitting position. Breastfeeding Care Before a baby is discharged assess if the baby is breastfeeding well. Do not discharge if breastfeeding is not yet established or if the baby is not feeding well Protection from infection Importance of washing her hands before and after handling the baby Cord care Keeping her baby clean Immunizations Hygiene ( Washing, Bathing) Wash the face, neck and underarms daily Look for signs of infection while washing the baby –Skin infection: spread the skin folds to look for pustules –Cord infection: redness of skin, discharge, foul odor –Eye infection: redness, swelling of eyelids, discharge Wash the buttocks when soiled. Dry thoroughly Hygiene ( Washing, Bathing) • Bath when necessary: – Ensure the room is warm –Use warm water for bathing –Thoroughly dry the baby, dress and cover after bath • Never use soap on a newborn’s face, only clean water • Do not clean inside the NB’s ear canal or nose, only the outside • Do not use baby powder Cord care • Wash hands before and after cord care - Put nothing on the stump - Fold diaper below the stump - Keep stump loosely covered with clean clothes - If the stump is wet, wash with clean water and soap, dry with clean cloth. POGS MDG COUNTDOWN: Capacity Enhancement Program for Midwives 2010 57 •DO NOT bandage the stump or abdomen •DO NOT apply substances or medicines to stump •Avoid touching the stump unnecessarily •If umbilicus is red or draining pus or blood, see the health worker Eye care •Do not apply anything on the baby’s eyes except an antimicrobial at birth! Immunizations •BCG and Hepatitis B MONITORING THE BABY • Watch the baby for any danger signs: –Breathing difficulty –Noisy breathing (grunting) –Fast of slow breathing –Chest in-drawing –Feels cold –Fever –Red swollen eyelids and with pus –Redness of skin around the umbilicus with pus discharge –Convulsions –Jaundice/yellow skin •Bleeding from the cord: –Check if the tie is loose and retie the cord –Press to stop bleeding –Examine and assess the baby immediately Check for special treatment needs •Give prescribed treatments according to the schedule o treatment for infections o TB o Congenital Syphilis o Maternal illness: risk of bacterial infection o Eye/cord infection Advise the mother to seek care for the baby • Return or go to the hospital immediately if the baby has: - Difficulty breathing - convulsions - Fever or feels cold - Bleeding - Has diarrhea - not feeding at all POGS MDG COUNTDOWN: Capacity Enhancement Program for Midwives 2010 58 • Go to the health center as quickly as possible if the baby has: - Difficulty feeding - Pus from eyes - Skin pustules - Yellow skin - A cord stump which is red and draining pus - Feed less than 5 times in 24 hours - Other concern NEWBORN RESUSCITATION INTERVENTION: See Algorithm on Resuscitation (p 21). ACTION: Start resuscitation if the newborn is not breathing or is gasping after 30 seconds of drying or before 30 seconds of drying if the baby is completely floppy and not breathing. Clamp and cut the cord immediately, if necessary. Transfer the newborn to a dry, clean and warm surface.Keep the newborn wrapped or under a heat source if available.Inform the mother that the newborn needs help to breathe. INTERVENTION ACTION: Open airway Position the head so it is slightly extended. Introduce the suction tube: – First, into the newborn’s mouth 5 cm from the lips and suck while withdrawing. – Second, 3 cm into each nostril and suck while withdrawing. – Repeat once, if necessary taking no more than a total of 20 seconds. Notes: - Do not suction mouth and nose prior to delivery of the shoulders of babies with meconium stained amniotic fluid. K11 INTERVENTION ACTION: Ventilate, if still not breathing 1. Place mask to cover chin, mouth and nose to achieve a seal. 2. Squeeze bag attached to the mask with 2 fingers or whole hand, according to bag size, 2 or 3 times. Observe rise of chest. If chest is not rising:, reposition baby’s head If baby’s chest is still not rising check for adequate mask sealIf chest is still not rising, squeeze bag harder. If chest is rising, ventilate at 40 breaths per minute until newborn starts crying or breathing. POGS MDG COUNTDOWN: Capacity Enhancement Program for Midwives 2010 59 3. Reassess at 30-second intervals. If baby still fails to improve, check the following: Failure To Improve Checklist – Face-mask seal tight? – Airway clear of secretions? – Head positioned properly? – Is contact with the soft tissue of the infant’s anterior neck being avoided? – Resuscitator working properly? – Adequate pressure being used? – Air distending the stomach? – Air leak (pneumothorax)? – If baby starts crying or breathing >30 per minute and has no chest-in-drawing, stop ventilating: – Put the newborn in skin-to-skin contact on mother’s chest and continue care while monitoring breathing and warmth. Explain the baby’s condition to the mother. If after 30 sec of effective bag/mask ventilation,the newborn is gasping/ breathing <30 per min or > 30 per min but has severe chest in-drawing: – Continue bag/mask ventilation – Continue assessing at 30 sec intervals while transporting or – Proceed to intubation per advanced resuscitation guidelines, if skilled personnel and equipment are available – If after 20 minutes of effective ventilation, the newborn does not start to breathe or gasp at all, stop ventilating. – Explain to the mother that the baby is dead, give supportive care and record the event. Notes: – While ventilating, refer and explain to the mother what happened, what you are doing and why. – Ventilate, if needed, during transport – Record the event on the referral form and labor record. K11 K11D19K11 ADDITIONAL CARE Resuscitation With Bag & Mask Self-inflating Bag: Basic Parts Bag and Mask: Equipment Masks Rims –Cushioned –Non-cushioned Shape –Round –Anatomic shape POGS MDG COUNTDOWN: Capacity Enhancement Program for Midwives 2010 60 Size –Small –Large Position Bag and Mask on Face Mask should cover Tip of chin Mouth Nose •Do not jam the mask down on the face •Do not allow your fingers or parts of the hands to rest on the newborn’s eyes •Do not put pressure on the throat (trachea) •Airtight seal is essential to achieve positive pressure. Tight seal required for flow-inflating bag to inflate Tight seal required to inflate lungs when bag is squeezed How Hard to Squeeze the Bag Noticeable rise and fall of chest Bilateral breath sounds Improvement of color and heart rate Frequency of Ventilation: 40 to 60 breaths per minute If the Chest is Not Expanding Adequately Possible causes Seal inadequate Airway blocked Not enough pressure given Signs of Improvement after Positive pressure ventilation Improving color Spontaneous breathing Increasing heart rate Post-resuscitation Care Baby requires Close monitoring Anticipatory care Laboratory studies POGS MDG COUNTDOWN: Capacity Enhancement Program for Midwives 2010 61 Examination of the newborn baby OBJECTIVES: •To describe and carry out an examination of a baby soon after birth; before discharge from hospital; during the first week of life at routine, follow-up or sick newborn visit and identify any conditions which need specific care treatment or follow up. •To assess, classify and treat a newborn baby using the ‘Examine the Newborn’ chart J2-J8 When should a newborn baby be examined? After birth: •At around an hour •before discharge from hospital (no discharge before 12 hours of age) •If there is maternal concern about the baby’s condition •If a danger sign observed during monitoring After leaving the hospital: •during the first week of life at a routine visit •follow-up •sick newborn visit. ACCORDING TO NATIONAL GUIDELINES Why do we examine the baby at birth and again at discharge? At the time of birth: •Overall assessment of the baby’s condition •An initial set of observations •To provide appropriate care and treatment Before discharge and thereafter: •To re-assess and monitor the baby’s condition •To provide appropriate treatment if the baby’s condition changed from a previous examination •To give the mother guidance on continuing care Universal precautions: remember to was your hands before and after examining the baby Examination Format •Assess –Ask, Check, Record –Look, Listen, Feel •Classify •Treat or advise •Record POGS MDG COUNTDOWN: Capacity Enhancement Program for Midwives 2010 62 DANGER SIGNS? •History of convulsion •Difficulty feeding •Temperature of 37.5ºC and above •Temperature <35.5ºC •Movement only when stimulated •Respiratory rate of 60 breaths per minute or more •Severe chest in-drawing If Danger Signs present,CLASSIFY : POSSIBLE SERIOUS ILLNESS TREAT AND ADVISE: •Give first dose of 2 IM antibiotics Ampicillin •Refer baby urgently to hospital •After emergency treatment, explain the need for referral to the mother/father. •Organize safe trasportation. •Always send the mother with the baby, if possible. •Send referral note with the baby •Inform the referral center if possible by phone or radio. Normal findings 1 A baby: • passes urine six or more times a day after day 2. •May pass six to eight watery stools a day. •May have some vaginal bleeding for a few days during the first week after birth. It is not a sign of a problem. Assess Breathing When assessing breathing: •count number of breaths taken for one full minute. •If not sure of breaths per minute, repeat count. •Look for chest in-drawing •Listen for grunting •Normal respiratory rate of a newborn baby - 30 to 60 breaths per minute. •No chest idrawing •No grunting on breathing out •Babies may breathe irregularly (up to 80 breaths per minute) for short periods of time. •Small babies (less than 2.5 kg at birth or born before 37 weeks gestation) may: –have some mild chest in-drawing –periodically stop breathing for a few seconds. POGS MDG COUNTDOWN: Capacity Enhancement Program for Midwives 2010 63 Color : • Face, chest, tongue and lips are pink • Hands and feet may be bluish during the first 48 hours • Jaundice occurring on the second day lasting for about 14 days Posture and tone: •Arms and legs are well bent (flexed) •Loosely clenched fists •Flexed arms, hips and knees •Preterm babies have less flexion •Babies who were in breech position may have fully flexed hips and knees; the feet may be near the mouth; or the legs and feet are at the side of the baby Activity : •Moves both arms and legs equally •+ rooting, moro, grasp, sucking reflex Warmth: Baby’s abdomen or back or feet feels warm Heart Rate: Count the baby’s heartbeat for 1 full minute • 100 – 160 beats/min Skin : •Milia •Mongolian spots •Peeling/desquamation •Erythema toxicum (red spots with tiny white centers) seen on the face, trunk and back on day 2 and later Head : • Molding ( usually disappears in 2-3 days after birth) • Caput succedaneum(soft swelling over the presenting part of the head (disappears after 48 hours) • Anterior fontanelle is flat and may swell when the baby cries • Anterior fontanelle is flat and may swell when the baby cries Eyes: no discharge Mouth: Lips, gums and palate are intact • Baby sucks vigorously on your finger Chest : • Moves equally with breathing • Abdomen pushes out with each breath • Breast nodules maybe enlarged (boys and girls) Abdomen : • Rounded, soft • Umbilical cord is dry, no bleeding • Small umbilical hernia is normal during the 1st year POGS MDG COUNTDOWN: Capacity Enhancement Program for Midwives 2010 64 Back and spine: • Skin over the back has no openings • No defects Anus : • Patent • Baby passes stool by 24 hours Female Genitalia : • white vaginal discharge • A bloody vaginal discharge that starts on day 2-3 and continues up to day 7 Male Genitalia: • Foreskin retracted easily • Urethra opens at the end of the penis • Testes are felt in the scrotum Temperature : • 36 - 37ºC axillary • If no thermometer, feel the chest or back with the back of your hand Weight : • 2.5 up to 3.99 kg • Weight loss of 5-10% of their birth weight in the first few days of life. Regains birthweight by 10 – 14 days of life. Weigh the Baby Why do we weigh the baby? •Assess weight gain( K7) •Provides a baseline and is part of growth monitoring •Indicates whether the baby is receiving adequate nutrition •Identifies a low birth weight baby who are at risk and needs monitoring and special care •For drug calculation •Identifies babies who have an underlying condition and needs examination and treatment How to weigh a baby : Take the scales to the baby Prepare the scales »Cover pan with a clean cloth Preparing and weighing the baby »Remove all clothing including the diaper »Weigh baby naked »WAIT till baby stops moving »Read and record the weight »Wrap the baby »Return baby to the mother POGS MDG COUNTDOWN: Capacity Enhancement Program for Midwives 2010 65 Scale maintenance »Clean the scale pan between each weighing »Calibrate daily In postnatal clinics: Weigh a baby on THE SAME SCALES at each visit Assess Breastfeeding •If the baby is breastfeeding at the time of examination, observe and assess the feed. •If the mother is not breastfeeding, ask the mother to call the health worker when the baby next wants to feed so that feeding can be observed. •Observe breastfeeding for at least five (5) minutes. Normal findings: • Baby should breastfeed at least 8X in 24 hours (at least every 3 hours) • A low birthweight baby needs to breastfeed more often, at least every 2 to 21/2 hours. • Suckling should be vigorous and suckling well Make a plan and care for the needs and problems of the newborn • Education and counseling • Medical treatment • Referral and follow up. Check Color Abnormal findings and plan of action Abnormal findings Action < 24 hours old with yellow skin Refer on face >24 hours old with yellow p[alms and soles (possible infection, blood group incompatibility) Pallor (bleeding, poor circulation, cold, low blood sugar) Make sure cord tie is tight Warm the baby Check respiration Ensure breastfeeding Refer POGS MDG COUNTDOWN: Capacity Enhancement Program for Midwives 2010 66 Breathing Posture and tone Noisy breathing Refer (grunting) Flaring nostrils Indrawing of the chest between ribs (Obstruction of airway, infection) RR < 30 or >60/min Apnea or gasping Limp, floppy (prematurity, birth injury, asphyxia Rigid, stiffness or arching of the back Rhythmic movements of one or both limbs (tetanus, birth injury meningitis) Newborn resuscitation Refer Keep baby warm Give initial dose of antibiotics prior to referral Skin Pustules, blisters, red or purple Treat skin pustules: spots Wash hands (localized infection but may lead Wash off pus and crusts with boiled and to sepsis if untreated cooled water and soap Dry with a clean cloth Paint with gential violet Head Cephalhematoma (swelling on None. the blood is slowly absorbed and one side of the head) disappears by 1-2 months Eyes Discharging pus Sticky eyes Swollen eyelids ( eye infection – gonorrhea or chlamydia) Mouth Cleft lip / palate (congenital abnormality abdomen Distended and hard ( possible intestinal obstruction) Abdomen Refer Wash hands Wet clean cloth with cooled boiled water Use wet cloth to gently was off pus from the baby’s eyes Apply antimicrobial to eyes 4x a day Re-assess in 2 days Re-assure the mother Encourage mother to breastfeed/ feed the baby expressed breast milk by cup Refer to specialist Refer Open tissue on the abdomen ( Refer omphalocele, gastroschisis) Cover with sterile tissue soaked with sterile saline solution Bleeding from the umbilical cord Retie the cord tightly Red umbilicus or skin around it Treat umbilical infection (local umbilical infection) -wash hands -wash off pus and crusts with cooled POGS MDG COUNTDOWN: Capacity Enhancement Program for Midwives 2010 67 boiled water -dry with clean cloth -paint with gentian violet Back and spine Open tissue on the back ( neural tube defects) External genital organs Unable to define gender Refer Cover witjh sterile tissues soaked with saline solution Refer No urine or wet diaper by 24 hours Boys external genitalia Urethra does not open at the end of penis but under the penis; foreskin not retractable Temp. Weight Refer Scrotum is empty ( no testes felt) Explain to parents that the testes may descend Examine the baby again at 6 months Refer if the testes has not come down Axillary temp <36ºC or >37ºC, or Baby’s back or chest feels cooler or hotter than the skin of a normal person Weight less than 2500 grams (preterm or SGA) Refer Give first dose of antibiotics Keep the temperature normal Special care Weight > 4000 grams Feed as soon as possible after birth (infant of diabetic mother, risk of low blood sugar Care of the newborn until Discharge Teach and counsel a mother and her family about newborn care ; •What care to give •Why to give the care Warmth Keep the room warm ( 25 - 28ºC) Skin-to-skin contact Dress the baby or cover with dry, clean cloth Cover the head with a cap especially if the baby is small Assess warmth - touch feet, abdomen or back Sleep POGS MDG COUNTDOWN: Capacity Enhancement Program for Midwives 2010 68 •At night let the baby sleep with the mother or within easy reach to facilitate breastfeeding •Let the mother and baby sleep under a bed net to protect them from malaria •A baby who is hard to wake up or sleeps too much may be sick Support breastfeeding •Counsel on the importance of exclusive breastfeeding •Encourage breastfeeding on demand day and night –Do not give any other feeds or water –Do not use artificial teats and pacifiers Breastfeeding •Ask the mother if there is a breastfeeding problem/difficulty. •If mother has breastfeeding difficulty, assess breastfeeding •Teach correct positioning and attachment Key points to good attachment The baby’s mouth is widely open •The tongue is far forward in the mouth, and may be seen over the bottom gum •The lower lip is turned outwards •The chin is touching the breast •More areola is visible above the baby’s mouth than below it Problems that may arise if the baby is not well attached to the breast The baby: •May cry a lot and be unhappy •May be slow to gain weight, or may even lose weight The mother: •May get sore/cracked nipples •May get very full breasts which feel hard, sometimes they may feel hot and may look red Key points to good positioning •The baby’s head and body are in a straight line •The baby’s face is opposite the nipple and breast •The baby’s upper lip or nose is opposite the mother’s nipple •The baby is held as close to the mother’s body as possible •The baby’s whole body is supported if the mother is in a sitting position. Breastfeeding Care •Before a baby is discharged assess if the baby is breastfeeding well. •Do not discharge if breastfeeding is not yet established or if the baby is not feeding well POGS MDG COUNTDOWN: Capacity Enhancement Program for Midwives 2010 69 Protection from infection •Importance of washing her hands before and after handling the baby •Cord care •Keeping her baby clean •Immunizations Hygiene ( Washing, Bathing) •Wash the face, neck and underarms daily •Look for signs of infection while washing the baby –Skin infection: spread the skin folds to look for pustules –Cord infection: redness of skin, discharge, foul odor –Eye infection: redness, swelling of eyelids, discharge •Wash the buttocks when soiled. Dry thoroughly Hygiene ( Washing, Bathing) •Bath when necessary: – Ensure the room is warm – Use warm water for bathing – Thoroughly dry the baby, dress and cover after bath •Never use soap on a newborn’s face, only clean water •Do not clean inside the NB’s ear canal or nose, only the outside •Do not use baby powder Cord care •Wash hands before and after cord care - Put nothing on the stump - Fold diaper below the stump - Keep stump loosely covered with clean clothes - If the stump is wet, wash with clean water and soap, dry with clean cloth. •DO NOT bandage the stump or abdomen •DO NOT apply substances or medicines to stump •Avoid touching the stump unnecessarily •If umbilicus is red or draining pus or blood, see the health worker Eye care •Do not apply anything on the baby’s eyes except an antimicrobial at birth! Immunizations •BCG •Hepatitis B POGS MDG COUNTDOWN: Capacity Enhancement Program for Midwives 2010 70 MONITORING THE BABY •Watch the baby for any danger signs: –Breathing difficulty –Noisy breathing (grunting) –Fast of slow breathing –Chest in-drawing –Feels cold –Fever –Red swollen eyelids and with pus –Redness of skin around the umbilicus with pus discharge –Convulsions –Jaundice/yellow skin •Bleeding from the cord: Check if the tie is loose and retie the cord Press to stop bleeding Examine and assess the baby immediately Check for special treatment needs •Give prescribed treatments according to the schedule treatment for infections TB Congenital Syphilis Maternal illness: risk of bacterial infection Eye/cord infection Follow up Visits •Routine visits: •Follow-up Visits • Advise the mother to seek care for the baby •Return or go to the hospital immediately if the baby has: - Difficulty breathing - convulsions - Fever or feels cold - Bleeding - Has diarrhea - not feeding at all •Go to the health center as quickly as possible if the baby has: - Difficulty feeding - Pus from eyes - Skin pustules - Yellow skin - A cord stump which is red and draining pus - Feed less than 5 times in 24 hours - Other concern POGS MDG COUNTDOWN: Capacity Enhancement Program for Midwives 2010 71