Principles of drug susceptibility testing
advertisement

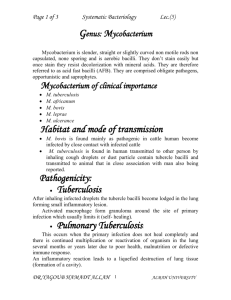
Module 10 Drug susceptibility testing Part 1. Principles of resistance to antituberculosis drugs Part 2. Performing DST on solid media Purpose Part 1. To provide you with knowledge of the principles of antituberculosis therapy and drug resistance, and of the relationship of drug resistance to treatment failure. Part 2. To provide you with the knowledge and skills to perform DST using the proportion method on solid and liquid media. Prerequisite modules Modules 1, 2, 3, 4, 6 and 7 Module time Part 1: 35 minutes Part 2: 1 hour and 10 minutes, plus two practical sessions in the laboratory (3 hours) Learning objectives At the end of Part 1of this module you will understand: ‒ ‒ ‒ ‒ ‒ the objectives and rationale of combined antituberculosis therapy; the basic definitions of drug resistance in TB; how drug resistance develops; the rationale for using a critical concentration of drug in laboratory assays; the rationale for determining the proportion of resistant bacteria that is clinically significant. At the end of Part 2 of the module you will be able to: ‒ ‒ ‒ ‒ Content outline explain the different methods for performing DST; perform and interpret the proportion method; record and report DST results; store strains. Part 1 History and objectives of antituberculosis therapy • Compartmentalization of M. tuberculosis in infected tissue • Bactericidal and sterilizing activity of drugs • First-line antituberculosis drugs • Basic definitions of drug resistance • Development and genetic basis of drug resistance • Relationship of critical concentrations and proportion of resistant bacteria to prediction of treatment failure 1 Part 2 • Drug susceptibility test methods: ‒ direct ‒ indirect • Proportion method: technical protocol, interpretation criteria • Recording and reporting DST results • Storage of strains Exercises Practical work in the laboratory: ‒ ‒ Annexes perform proportion method read DST results. 10.1 Proposed protocol – drug susceptibility testing, proportion method 10.2. Proposed protocol – strain maintenance. 2 PART 1. PRINCIPLES OF DRUG SUSCEPTIBILITY TESTING Introduction Drug-resistant strains of Mycobacterium tuberculosis exist worldwide and constitute a serious threat to the efficacy of TB control programmes. The most effective strategies for limiting further spread of drug-resistant TB are rapid detection of drug resistance followed by prompt and effective therapy. This module provides an introduction to the principles of antituberculosis therapy and drug-resistance and describes the relationship of drug resistance to treatment failure. History of antituberculosis therapy In the 1940s, two drugs – streptomycin (SM) and p-aminosalicylic acid (PAS) – were introduced for TB therapy. Use of either SM or PAS alone in the treatment of TB was initially found to reduce deaths among treated patients. Single-drug therapy soon resulted in the emergence of drug-resistant strains in a majority of the patients; however, by combining SM and PAS, the resistance rate was significantly reduced. Eventually, more effective anti-TB drugs were introduced and used in combined therapy. Isoniazid (INH) was introduced in the early 1950s. Use of INH in combination with SM and PAS was highly effective in preventing the emergence of resistance, but 18 months of treatment were required to ensure an adequate cure. Pyrazinamide (PZA), rifampicin (RMP) and ethambutol (EMB) were also introduced for TB treatment and were prescribed in combinations with INH. Extensive studies to define the optimal drug combination and the minimal duration of therapy were carried out by the British Medical Research Council. The result was the 6month short-course therapy consisting of 2 months’ treatment with INH, RMP and PZA, followed by 4 months’ treatment with INH and RMP. This protocol is still in use today, and is recommended with slight modifications (including possible addition of EMB or SM) by WHO, the International Union Against Tuberculosis and Lung Disease (IUATLD), the American Thoracic Society, the Centers for Disease Control and Prevention (CDC), and the Infectious Disease Society of America. Objectives of antituberculosis therapy Antituberculosis therapy has three important goals: ‒ ‒ ‒ to rapidly kill the large numbers of active bacilli that are multiplying in the infected tissues; to prevent the emergence of a clinically significant proportion of drug-resistant mutants; and to effectively eliminate bacilli that are dormant but still viable from the infected tissues. Anatomical and metabolic compartmentalization of M. tuberculosis in infected tissue Scientists and clinicians have postulated three populations (A, B and C) of tubercle bacilli in a patient with pulmonary TB (see Figure 1). These populations are differentiated by their locations within the lesions and by their metabolic activity. 3 Population A represents the large number of rapidly multiplying bacilli found in pulmonary cavities. Population B represents bacilli that multiply less rapidly because of local adverse (most often acidic) conditions. Elimination of Populations A and B through effective therapy results in negative sputum smear (usually after 2–3 weeks) and culture (usually after 2 months). Population C consists of dormant bacilli (often sequestered in granulomas) that are still capable of sporadic bursts of metabolism and replication – and it is these organisms that can be the source of potential relapses. Anti-TB drugs such as INH play a pivotal role in killing Population A; these drugs are considered to have rapid bactericidal activity (Figure 1). Bactericidal activity is measured by the rapidity with which sputum smears and culture become negative during treatment of pulmonary TB. The drugs that are most active in killing Population A are also the most effective in preventing the emergence of drug-resistant cells (as discussed in more detail in the next section). Anti-TB drugs that are more effective against Populations B and C are regarded as sterilizing agents. PZA is especially effective against Population B because of its unique sterilizing activity in an acidic environment, while RMP is more active against both Populations B and C (Figure 1). The potency of this activity is reflected in a high cure rate with limited relapses in patients who complete therapy. First-line antituberculosis drugs Isoniazid Isoniazid is a pro-drug that requires activation by the mycobacterial enzyme, catalase. It has a potent early bactericidal effect on rapidly multiplying, metabolically active M. tuberculosis (Population A, Figure 1),. Although INH may act on several targets within the mycobacterial cell, significant evidence supports the concept that it blocks the synthesis of cell-wall mycolic acids, the major component of the envelope of M. tuberculosis (Figure 2). Rifampicin In addition to a significant early bactericidal effect on metabolically active M. tuberculosis (Populations A and B, Figure 1), RMP also exhibits excellent late sterilizing action on semi-dormant organisms undergoing short bursts of metabolic activity (Population C, Figure 1). This late effect of RMP and the additional effectiveness of PZA have allowed routine TB treatment to be reduced from one year to six months. The sterilizing activity of RMP is critical for successful therapy since resistance to this drug is one of the main reasons for treatment failure and a fatal outcome in TB patients. The mechanism of action of RMP is inhibition of RNA transcription in the mycobacterial cell by targeting DNA-dependent RNA polymerase (Figure 2). Pyrazinamide PZA has an excellent sterilizing effect on slowly multiplying tubercle bacilli (Population B, Figure 1) especially in an acidic environment. When PZA is used in combination with RMP, the duration of TB treatment is reduced from one year to six months. PZA is a pro-drug, converted to its active form, pyrazinoic acid, by the mycobacterial enzyme pyrazinamidase; the mechanism of action is not well understood, proposed targets for 4 pyrazinoic acid include an enzyme involved in fatty acid synthesis and the destructive acidification of mycobacterial cytoplasm (Figure 2). Figure 1. Compartmentalization of M. tuberculosis in the infected tissue Adapted from: Iseman M. A clinician‘s guide to tuberculosis. Philadelphia, Lippincott, Williams & Wilkins, 2000. Basic definitions and general principles of drug resistance in M. tuberculosis Members of the M. tuberculosis complex (MTBC) (M. tuberculosis, M. africanum, M. canettii, M. microti, M. bovis, M. bovis BCG, and M. bovis ssp caprae) share several means of natural resistance to some antibiotics. A hydrophobic, lipid-rich cell envelope surrounds these organisms and serves as a permeability barrier to many compounds. Also, drug efflux systems and drug-modifying enzymes are present. However, differences in natural resistance within the MTBC have been observed. For example, strains of M. canettii, M. bovis and M. bovis BCG are resistant to PZA, while other members of the MTBC are usually susceptible to this drug. The following definitions are based on recommendations from WHO: drug resistance among previously treated patients (acquired drug resistance) is the most common type of resistance to any of the first-line drugs, and develops in a patient during chemotherapy. In contrast, drug resistance among newly identified patients (primary 5 drug resistance) is defined as the presence of drug-resistant organisms in a previously untreated person, presumably because that person has been infected with a strain that had acquired resistance in another host. Cross-resistance can occur between drugs that are chemically related and/or have the same or a similar target within the mycobacterial cell. For example, approximately 70– 90% of RMP-resistant strains are also resistant to rifabutin (chemically related); some strains of M. tuberculosis with low-level resistance to INH are cross-resistant to ethionamide (similar target); and cross-resistance can develop between certain aminoglycosides, e.g. kanamycin and amikacin, or between fluoroquinolones. However, no cross-resistance has been seen between INH and PZA, even though both drugs are analogues of a common component, nicotinamide. Figure 2. First-line anti-TB drugs and their mechanisms of action 6 Porin Lipoarabinomannan (LAM) Mycolic Acids INH Arabinogalactan Cytoplasm PZA Short chain fatty acid precursors Chromosomal DNA Cell Wall and cytoplasmic membrane Free Wall Glycolipids and Proteins RNA Polymerase (ß-subunit) RNA Transcription RMP Adapted from Somoskovi, Parsons, Salfinger. 2001, Respir. Res. 2:164-168 Polyresistance occurs when a strain of M. tuberculosis develops resistance to more than one anti-TB drug. Resistance to INH and RMP, which are the most effective anti-TB drugs, results in treatment failure and fatal outcomes more often than resistance to other drugs. Strains resistant to both INH and RMP are therefore distinguished from other polyresistant strains and defined as multidrug-resistant tuberculosis (MDR-TB). An even more serious threat is the recently described extensively drug-resistant tuberculosis (XDR-TB); these strains of M. tuberculosis are resistant not only to INH and RMP but 7 also to at least one of the fluoroquinolones and to one injectable drug such as kanamycin or amikacin. Development of resistance to antituberculosis drugs in M. tuberculosis Resistance to anti-TB drugs in M. tuberculosis occurs when resistant mutants, naturally occurring in the mycobacterial population, are selected by inadequate or interrupted treatment with anti-TB agents. Mutations occur spontaneously in the DNA of all cells, but many of these changes are deleterious and are selected against during growth of bacterial populations. However, a bacterial cell carrying a mutation that changes the structure of a protein that is the target for a particular drug, but does not compromise the protein’s functioning, will be selected for in the presence of the drug. Thus, for example, mutations that alter the amino acid sequence of the DNA-dependent RNA polymerase of M. tuberculosis such that it will no longer bind RMP will result in an RMP-resistant clone of tubercle bacilli. If single antibiotic treatment of TB were to be used, such clones would predominate in the population and, if not removed by the immune system, would cause therapy failure. This is what occurred in the 1940s when single-drug therapy with SM was used. Mutants resistant to any given drug occur randomly and rarely, on average once in every 108 (100 million) cells. That is, there is a chance of one mutation occurring in a given gene (e.g. a gene encoding a target protein) each time 100 million bacteria divide. Given exposure to selection pressure by antibiotics, this rare event can readily give rise to substantial clones of resistant cells because of the large numbers of bacteria involved (easily 108 per lesion in lung cavities). By using two antibiotics, however, the chances that any given cell in the population will simultaneously carry resistance to both antibiotics is 10–8 x 10–8 , or 10–16. Consistent with this theory, it was found that monotherapy led to selection of drugresistant populations more frequently in cases of cavitary disease, in which lesions contain abundant tubercle bacilli (108–109 per lesion), than in cases with non-cavitary lesions, which contain relatively few cells (about 103–104 per lesion). Other factors can also influence the emergence of drug resistance. Although the tubercle bacillus replicates actively in vivo, it has a long generation time and a tendency to shift its metabolism toward a dormant state (Population C, Figure 1). Such variations in metabolic activity make this organism a difficult therapeutic target. In addition, penetration of antibiotics to various body sites can vary significantly, resulting in some lesions with suboptimal concentrations of drugs and thus a greater opportunity for selection of drug-resistant mutants. The individual patient’s influence on the development of drug resistance should also be considered. It has been found that the TB patients most likely to produce drug-resistant mutants are those who are experiencing increases in the bacterial population, together with compromised drug penetration due to underlying host conditions, particularly poor intestinal absorption of drugs due to HIV/AIDS. Critical antituberculosis drug concentrations, proportion of resistant mutants and their relation to the accurate prediction of therapeutic failure in vivo Early investigators of laboratory diagnosis of drug resistance faced two significant challenges. First, critical concentrations – drug concentrations necessary to eliminate susceptible (wild-type) strains of M. tuberculosis – needed to be determined. Second, 8 the proportion of a population of M. tuberculosis that would need to be resistant to a drug in order for that strain to be interpreted as resistant, thus permitting accurate prediction of therapeutic failure, was unknown. With regard to the first challenge, it was observed that drug-susceptible strains of M. tuberculosis that have not been exposed to anti-TB drugs (wild-type strains) do not exhibit much variation in the minimum inhibitory concentrations (MICs) to those drugs. It was thus determined that the critical concentration should be the concentration of drug that inhibits the growth of wild-type strains without appreciably affecting the growth of resistant cells. It was also found that the critical concentration varies with the media used in the different susceptibility assays, which has resulted in slight variations in the concentrations tested in laboratory assays, especially when using either solid or liquid media. Since drug resistance develops by natural selection of mutants pre-existing in the bacterial population, both drug-resistant and drug-susceptible cells will be present during the early stages of resistance development, even without exposure to any anti-TB drugs. Thus, clinically significant resistance to all anti-TB drugs was defined as in vitro growth, in the presence of the critical concentration of the drug, that is equal to or greater than 1% of the growth in the absence of the drug. This definition is justifiable: for a susceptible strain of M. tuberculosis, the proportion of potentially resistant mutants (based on a mutation rate of 1 in 100 million cells) would theoretically be only 0.000 001 % of the entire population. Thus, the presence of 1% resistant cells represents a substantial increase in resistance. Based on these assumptions, laboratory assays compare the growth of a 1:100 dilution of the M. tuberculosis isolate on media without drug with growth of the undiluted suspension on media containing each drug. If the undiluted suspension grows faster or more abundantly in the presence of the drug than does the 1:100 dilution in the absence of the drug, the isolate is considered to contain a resistant population greater than 1% and is reported as resistant. Comparison of laboratory findings with clinical outcomes of patients has revealed that such an increase in the proportion of drug-resistant cells, measured at the critical concentration of a particular drug, would adequately predict therapeutic failure, while a smaller proportion (≤1%) of resistant cells may still be well controlled with standard first-line therapy. In summary, the critical concentration is the amount of drug in the medium that inhibits the growth of susceptible organisms but not that of the resistant mutants, while the clinically significant proportion of resistant mutants indicates the magnitude of the proportion of drug-resistant bacilli that either predict or reflect therapeutic failure. 9 KEY MESSAGES Combined anti-TB therapy is the cornerstone of effective treatment and prevention of drug resistance. The first-line anti-TB drugs are INH, RMP, PZA and sometimes EMB and SM. M. tuberculosis may exhibit natural resistance to certain antibiotics and may develop resistance to anti-TB agents as a result of spontaneous mutations in genes encoding drug targets or drug-activating enzymes. Anatomical, metabolic compartmentalization, mutation rates and increase in the bacterial load in the lesion may also greatly influence the emergence of drug resistance. WHO recommends use of the phrase “drug resistance in newly identified patients” instead of primary resistance, and “drug resistance in previously treated patients” instead of acquired resistance. Critical concentration is the amount of drug in the medium that inhibits the growth of susceptible organisms but not that of resistant mutants The clinically significant proportion of resistant mutants (determined to be greater than 1% of the population) indicates the magnitude of the population of drug-resistant cells that either predict or reflect therapeutic failure. 10 Module 10 Part 1: Review Find out how much you have learned by answering these questions. Give the definitions of primary and acquired drug resistance ________________________________________________________________________ ________________________________________________________________________ ________________________________________________________________________ ________________________________________________________________________ How does M. tuberculosis develop drug resistance? ________________________________________________________________________ ________________________________________________________________________ ________________________________________________________________________ ________________________________________________________________________ Explain how the relationship of critical concentrations and proportion of resistant bacteria predicts treatment failure. ________________________________________________________________________ ________________________________________________________________________ ________________________________________________________________________ ________________________________________________________________________ 11 PART 2. PERFORMING DRUG SUSCEPTIBILITY TEST Principles of DST Drug susceptibility testing (DST) is the determination of a strain’s susceptibility to drugs used in therapy: a “sensitive” result means that the patient with that strain has a high probability of treatment success, while a “resistant” result means that there is a high possibility of treatment failure and that the therapy should be changed. Thus, standardized and reliable DST of M. tuberculosis provides guidance for the treatment of the patient. A false resistance result may prompt the physician to replace an effective regimen with a less effective one, with a consequent detrimental effect on the patient’s health. Moreover, therapy for drug-resistant TB lasts longer and uses more expensive drugs, meaning a waste of drugs and money for the health system and a high probability of side-effects for the patient. A false sensitivity result prompts clinicians to continue with ineffective treatment and may result in the spread of drug-resistant strains in the community. Carrying out DST also provides an assessment of the drug resistance rates and trends in a country (or in different areas of a country); standardization is therefore essential to allow data from different laboratories to be compared. Standardization of DST is difficult: at each step there are certain variables that are not simple to control. For example, the potency and stability of drugs vary with conditions of sterilization and storage. Human factors may influence DST results: incorrect drug concentrations and/or inocula for the particular test may be used. Moreover, a deep understanding of resistance criteria is essential for reliable results. Drug susceptibility test methods DST methods currently in use are divided into two main groups – direct method and indirect methods. Direct drug susceptibility method In the direct DST method, a smear-positive sputum (at least 2+) is inoculated directly onto drug-containing and drug-free media. The inoculum size is adjusted according to the number of AFB observed on smear microscopy of treated and concentrated sputum; one control tube is inoculated with a dilution (10–2) of the sample. This method has certain advantages compared with indirect methods. First, the bacillary population used for performing DST is more representative of those existing in vivo, since all the bacilli in the sputum are represented in the inoculated sample. Second, the direct method takes 3–4 weeks less than indirect testing and there is no need for subculturing. There are also some disadvantages. The direct method can be used for highly smearpositive cases only (> or = 2+). This method has a high contamination rate and is more difficult to calibrate because both live and dead bacilli are seen on the smear. The failure rate of the method is 10–15% It is mandatory to perform identification at the species level before reporting DST results. Indirect drug susceptibility methods 12 For indirect DST methods, organisms from clinical materials are isolated in culture; either a homogeneous suspension of their growth or a broth culture is inoculated onto control and drug-containing egg-based media. The three main methods are: ‒ ‒ ‒ absolute concentration method; resistance ratio method; proportion method. Resistance of an M. tuberculosis strain determined by the proportion method differs from the usual concept of resistance in clinical microbiology. Any M. tuberculosis strain (even a “sensitive” one) always has some bacilli resistant to a particular drug, so reporting resistant cells becomes important only if they make up more than 1% of the total. This module explains only the proportion method, as it is the one recommended by WHO. Proportion method for DST Two principles form the basis of DST proportion method – critical concentration and critical proportion. The critical concentration is the level of drug in the medium that inhibits the growth of wild-type organisms but not that of resistant mutants; the critical proportion is the proportion of resistant mutants compatible with therapeutic success. The proportion method is the preferred DST method worldwide. In this method, several dilutions of the inoculum are inoculated on control and drugcontaining media to obtain colonies from one or other dilution so that exact numbers of colonies can be counted. From these counts, corrected by multiplying for the dilution of inoculum used and the total number of viable units in the population, the rate of resistant mutants in the population can be calculated and expressed as a percentage. The technique depends on two important criteria ‒ the critical concentration of the drug and the critical proportion of resistant bacilli. The method is simple and standardization of the inoculum is not critical for the results, which are influenced more by the dispersion of the inoculum on the surface of the medium: if not incubated perfectly slanted, bacilli grow on one side of the medium and colonies are not countable. It should be remembered that, in the absence of sufficient growth (>20 colonies, 1+) of the primary culture, DST should not be performed unless the culture comes from a patient who has completed anti-TB treatment. From cultures with scarce growth, the bacillary population used for performing DST may not be representative of those existing in vivo. Procedure and interpretation Calibration of the bacterial suspension from a culture With a loop, a representative sample of 5–10 mg is taken from the primary culture and placed in a spherical, flat-bottomed flask containing 5‒7 glass beads of diameter 3 mm. The flask is shaken for 20–30 seconds; drops of distilled water are added slowly with continuous shaking. The opacity of the bacterial suspension is then adjusted by the addition of distilled water to that of a MacFarland standard n°1 suspension by comparing with standard MacFarland suspension on a dark background. 13 Either a calibrated loop or pipettes may be used for further processing and for inoculation. Loop The loop should be of platinum wire (diameter 0.7 mm) and should have an internal diameter of 3 mm, which delivers 0.01 ml. (Delivery volume must be verified by weighing 10 loopfuls of distilled water deposited on a filter paper.) The two bacterial dilutions required for inoculation with the loop are 10–2 mg/ml and 10–4 mg/ml; additional dilutions 10–3 mg/ml and 10–5 mg/ml are useful for beginners and for safety of the procedure. The dilution 10–2 mg/ml is produced by discharging two loopfuls of the bacterial suspension, standardized at 1 mg/ml, into a small tube containing 2 ml of distilled water, and shaking. Similarly, the dilution 10–4 mg/ml is produced by discharging two loopfuls of the dilution 10–2 mg/ml into a small tube containing 2 ml of distilled water, and shaking. Two slopes of medium without drug and slopes of medium with drug are inoculated with a loopful of each dilution (see annex 1). Pipettes If pipettes are used, the inoculum for each slope is 0.1 ml. Accordingly, the two bacterial dilutions required for inoculation with the pipette are 10–3 mg/ml and 10–5 mg/ml; additional dilutions 10–4 mg/ml and 10–6 mg/ml are useful for beginners and for safety of the procedure. The dilutions are prepared by 10-fold dilution steps (0.5 ml of the bacterial suspension 1 mg/ml, discharged into 4.5 ml of distilled water, produces the dilution 10–1 mg/ml; 0.5 ml of the new dilution, discharged into 4.5 ml of distilled water, produces the dilution 10–2 mg/ml, etc., down to 10–6 mg/ml). The pipette is changed for each dilution. Two slopes of medium without drug and slopes with drug are inoculated with 0.1 ml of the two chosen dilutions (see annex 1). Reading of test The results are read for the first time on the 28th day. Colonies are counted only on slopes seeded with an inoculum that has produced exact readable counts or actual counts (up to 100 colonies on the slope). This inoculum may be the same for the control slopes and the drug-containing slopes, or it may be the low inoculum (10–6 mg of bacilli) for the control slopes and the high inoculum (10–4 mg of bacilli) for the drug-containing slopes. The average number of colonies obtained for the drug-containing slopes indicates the number of resistant bacilli contained in the inoculum. Dividing the second figure by the first gives the proportion of resistant bacilli existing in the strain. Below a certain value – the critical proportion – the strain is classified as sensitive; above that value, it is classified as resistant. The proportions are reported as percentages. If, according to the criteria indicated below, the result of the reading made on the 28th day is “resistant”, no further reading of the test for that drug is required: the strain is classified as resistant. If the result at the 28th day is “sensitive”, a second reading is made on the 42nd day: this provides the definitive result. Criteria of resistance Any strain with 1% (the critical proportion) of bacilli resistant to any of the four drugs – rifampicin, isoniazid, ethambutol, and streptomycin – is classified as resistant to that drug. 14 For calculating the proportion of resistant bacilli, the highest counts obtained on the drug-free and on the drug-containing medium should be taken, regardless of whether both counts are obtained on the 28th day, both on the 42nd day, or one on the 28th day and the other on the 42nd. Critical μg/ml Critical % 4 1 Isoniazid 0.2 1 Rifampicin 40 1 Ethambutol 2 1 Drug Streptomycin “Borderline cases” (about 1% growth on drug-containing medium) should be reported as resistant and retested. For details see Annexe 10.1. Critical points in performing DST proportion method Inoculum Control and drug-containing media must be inoculated with the proper number of organisms: if the numbers are too small, the sample size will not be enough for the critical proportion of resistant organisms to be detected; if the numbers are too large, the growth of naturally occurring drug-resistant mutants may simulate drug resistance (e.g. when big clumps of mycobacteria are inoculated). DST should be performed with actively growing cultures only, although subculturing of old strains might dilute the proportion of drug mutants. In indirect testing, the bacterial inoculum is laboratory-dependent and a proportion of susceptible or resistant bacilli not representing the situation in the patient’s lesion might be selected; hence the importance of performing correctly the inoculum, without choosing the colonies for DST. Contamination by NTM may also affect DST results and is not always easy to identify. As NTM are often resistant to the anti-TB drugs, a resistance pattern may be obtained that does not reflect the true susceptibility of the M. tuberculosis strain. Media The utmost care should be taken in the preparation of drug solutions and drugcontaining media. If drug concentration is lower than the recommended value, a sensitive strain may appear to be resistant; similarly, if the drug concentration is higher than the recommended value, a resistant strain may appear to be sensitive. The real concentration of drug depends on correct storage of drug solutions and drug-containing media: if incorrectly stored, the potency of the drug falls and give false sensitivity results. The same phenomenon results from prolonged or excessive heat during inspissation of the media. 15 Excessive moisture on the surface of the medium may affect the correct spreading of the inoculum, while excessive dehydration has a negative influence on the growth of bacteria. An H37Rv strain should be used to test each new batch of DST media. For each drug, a slant of the critical concentration and media with lower drug concentrations are tested with H37Rv strain. Compare results with the MIC of H37Rv (see Module 11). If the batch meets quality control standards, the results for patients’ strains may be reported as “susceptible” or “resistant”. DST should be done under an external quality assessment (EQA) programme (see Module 11 for details). Recording and reporting Reporting DST results is an important element of correct management of patients’ therapy. Rapid communication of a resistance, for example, will allow a prompt switch from an ineffective therapy to an effective one. The third part of the form suggested by WHO should be completed (figure 3). The essential data to be reported are: ‒ ‒ ‒ ‒ specimen number susceptibility date of reporting identity (signature) of the responsible person. 16 Figure 3. Request for sputum examination, culture and DST. Storage of strains 17 Once a strain has been identified and DST has been performed, the strain should be stored for further purposes, for example repeating DST in case of treatment failure, or sending to the reference laboratory for retesting. The storage conditions should never reduce the viability of bacilli and should therefore be sterile to avoid contamination. All the following procedures should be carried in the biological safety cabinet and vials can be thawed and frozen 2 or 3 times without reducing mycobacterial viability. For short-term storage, cultures on egg-based media kept at 4 °C should remain viable for up to 1 year. These cultures may also be kept at room temperature (maximum 20 °C, in air-conditioned rooms if necessary), in the dark, but media quality may deteriorate and viability may be affected Storage of liquid cultures for more than 1 month is not recommended since media quality deteriorates rapidly and affects viability, while clumping in liquids makes the determination of bacterial concentration highly unreliable. Moreover, liquid media are more prone to contamination. For long-term storage, patient cultures can be stored at -20 °C; note, however, that the viability of tubercle bacilli declines at -20 °C and only 1% are still viable after 2 years. It is thus crucial to prepare the heaviest bacterial load possible to compensate for the loss of viability. Provided that cultures (or subcultures) show luxuriant and abundant growth, they can be stored for up to 5 years after the initial isolation at -20 °C. Laboratories that perform culture identification also have to be able to maintain NTM species, specifically M. terrae, used for quality control of biochemical tests. Survival of NTM is usually much better but varies with species and strain. Most bacterial species other than tubercle bacilli survive equally well at -20 °C (100% survival after 3 years). Long-term storage of reference cultures, such as reference strains for quality control of DST and media preparation (M. tuberculosis H37Rv) is essential in the laboratory. Serial subculturing could lead to genetic drift and alter the phenotypic biological characteristics of strains. For details see Annexe 10.2. 18 Source material 1. Canetti G et al. Advances in techniques of testing mycobacterial drug sensitivity, and the use of sensitivity tests in tuberculosis control programmes. Bulletin of the World Health Organization, 1969, 41:21-43. 2. Collins C H, Grange J M, Yates M D. Tuberculosis bacteriology. Organization and practice. Oxford, Butterworth-Heinemann, 1997. 3. Kent PT, Kubica GP. Public health mycobacteriology: a guide to the Level III laboratory. Atlanta, GA, Centers for Disease Control, 1985. 4. Abdel Aziz M. Guidelines for surveillance of drug resistance in tuberculosis. 2003. Geneva, World Health Organization, 2003 (WHO/TB/2003.320). 5. Rüsch-Gerdes S, Domehl C, NArdi G, Gismondo MR, Welscher HM, Pfyffer GE. 1999. Multicenter evaluation of the Mycobacteria Growth Indicator Tube for testing susceptibility of Mycobacterium tuberculosis to first-line drugs. Journal of Clinical Bacteriology, 37:45-48. 6. Kim TH, Kubica GP. Long-term preservation and storage of mycobacteria. Applied Microbiology, 1972, 24(3):311-317. 7. Kim TH, Kubica GP. Preservation of mycobacteria:100% viability of suspensions stored at -70 °C. Applied Microbiology, 1973, 25(6):956-960. 8. Collins CH, Grange JM, Yates MD. Tuberculosis bacteriology: organization and practice. London, Oxford University Press, 1997. 9. http://www.who.int/tb/dots/r_and_r_forms/en/index.html 19 KEY MESSAGES The proportion method is valid for susceptibility testing of M. tuberculosis complex against anti-TB drugs. This method is considered to be the reference standard against which other routine methods shall be assessed. The proportion method determines the percentage of growth of a defined inoculum on a drug-free control medium vs. growth on culture media containing the critical concentration of an anti-TB. Slants must be read after 4 weeks of incubation for a provisional result and after 6 weeks of incubation for the definitive interpretation of results. The critical concentration to define a resistant strain is 1% of the inoculum. Test with invalid growth control should be repeated. 20 Module 10: review Find out how much you have learned by answering these questions. Explain the differences between direct and indirect DST methods. ________________________________________________________________________ ________________________________________________________________________ ________________________________________________________________________ List the possible errors in performing the proportion method. ________________________________________________________________________ ________________________________________________________________________ ________________________________________________________________________ List the consequences of a false resistance. ________________________________________________________________________ ________________________________________________________________________ ________________________________________________________________________ List the consequences of a false sensitivity. ________________________________________________________________________ ________________________________________________________________________ ________________________________________________________________________ 21