REASON FOR CONSULTATION: Newly
advertisement
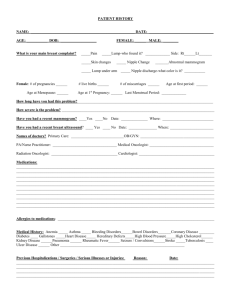
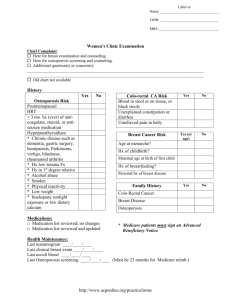
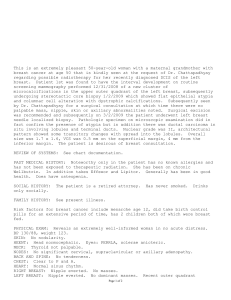
REASON FOR CONSULTATION: Newly-diagnosed breast cancer. REFERRING PHYSICIAN: This is as part of the multi-disciplinary cancer care with referring physician, Dr. Landreville. HISTORY OF PRESENT ILLNESS: Patient is a premenopausal, 48-yearold female who on a routine bilateral screening mammogram on January 14, 2009, was noted to have no suspicious findings on the left breast, but in the right inner breast a cluster of microcalcifications. Spot compression views on February 18, 2009, confirmed a cluster of irregular pleomorphic with the suggestion of a few branching forms in addition to linear grouping of calcifications nearby with the dominant cluster measuring 5 x 7 mm, considered suspicious. Stereotactic local-guided needle biopsy on February 4, 2009, revealed intermediate grade ductal carcinoma in situ with necrosis. The patient is now here for further discussion of the roll of systemic therapy. With regard to how she is feeling, she is still in shock of the diagnosis. In retrospect, she had not noticed any changes in her breast including nipple retraction, masses, skin changes. Her 14-point review of systems is negative other than some longstanding joint pain. PAST MEDICAL HISTORY: Status post right total hip replacement and cord decompression in the right hip. History of vascular thrombosis, status post resection of a benign tumor in her shoulder as a teenager. History of alcohol abuse. ALLERGIES: VICODIN causes a rash. SULFA causes nausea. MEDICATIONS: 1. Effexor. 2. Microgestin for migraines. 3. Trazodone. 4. Ativan. 5. Synthroid. 6. Maxalt. 7. Ibuprofen. 8. Promethazine for nausea associated with migraines. ETHYL AND TOBACCO: History of alcohol abuse, quit 6 months ago, but since then with this diagnosis has had 2 lapses. SOCIAL HISTORY: Lives alone and has no children. She has been trained as a radiation technologist but used to do office work and is currently not working. FAMILY HISTORY: Grandfather died of lung cancer in his 70s. aunt had ovarian cancer in her 50s. PHYSICAL EXAM: An ECOG performance status is zero. VITAL SIGNS: Per EPIC. GENERAL: She is an obese woman, somewhat anxious understandably. HEENT: Clear oropharynx. LYMPH NODES: No adenopathy. CHEST: Clear to auscultation bilaterally. CARDIOVASCULAR EXAM: Regular rate and rhythm. No murmurs. ABDOMEN: Soft, nontender, nondistended. No organomegaly. EXTREMITIES: No clubbing, cyanosis, or edema. BREASTS: Left: Normal contour. Normal nipple areolar complex. No dominant masses palpated. Right breast: Well-healed incision from needle biopsy with no dominant masses palpated. No skin changes. Normal nipple areolar complex. LABORATORY DATA: None. IMAGING STUDIES: Mammogram is as per above. ASSESSMENT AND PLAN: 48-year-old, premenopausal woman found to have a suspicious-appearing group of microcalcifications on a routine screening mammogram with stereotactic needle biopsy showing intermediate grade DCIS. We talked about the natural history of this disease and emphasized the curability of this disease. Explained that the patient needs to go in for a resection. She appears to be a candidate for breast conservation therapy, but is also of course a candidate for mastectomy and right now patient is opting for breast conservation therapy. I talked about the role of radiation therapy and reducing the chances of local recurrence. Spoke then about the role of the tamoxifen for prevention of recurrence of the ipsilateral and contralateral breast and told her that tamoxifen decreases the chances of a further breast cancer episode by almost 50 percent. Spoke about the adverse effects of tamoxifen including but not limited to weight gain, hot flashes, changes in mood, and the potentially serious risk of thromboembolic disease and uterine cancer. Explained to her that she would have to take tamoxifen for 5 years. The patient will think about these issues. For now I counseled her with regard to the risks of taking an oral contraceptive pill in the context of newly diagnosed breast cancer and I suggested that she find an alternative not containing estrogen. The patient will set up lumpectomy and then will see me 1 week after her surgery to discuss final pathology. Questions were answered, her concerns were addressed. Greater than 50 percent of this 40-minute was spent in consultation.