Post- Operative nausea and Vomiting (PONV)
advertisement

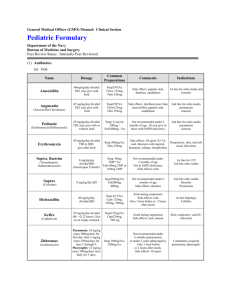
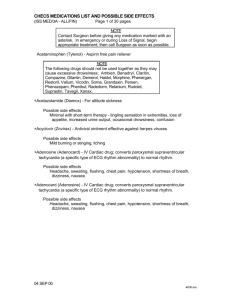
Post- Operative nausea and Vomiting (PONV) Apfel et al. A Factorial Trial of Six Interventions for the Prevention of Postoperative Nausea and Vomiting. NEJM 2004; 350: 244151 Gan TJ, et al. Society for Ambulatory Anesthesia Guidelines for the Management of Postoperative Nausea and Vomiting. Anes Analg 2007;105:1618-28. - Untreated, 1/3 will have post op n, v or both. In high risk estimated as high as 70-80% Annual costs in the US is estimated to be around several hundred million dollars Physiology of Vomiting--main sensors of somatic stimuli are located in the gut and chemo-receptor trigger zone (CTZ) --triggered by stimulation of chemo receptors in the upper GI tract and mechanoreceptors in the wall of the GI tract --area postrema is rich in dopamine-r and is a target for antagonists: haloperidol, metoclopramide, and the phenothiazines --Histamine-1 and muscarinic cholinergic recepotors are present in the nucleus ambiguous and lateral vestublar nucleus --5-hydroxytryptamine (5HT)-receptors are also present w/i the area postrema.5HT can activate dopamine release Causes: 1. Pharyngeal stimulation 2. Gastrointestingal distension 3. Abdominal Surgery 4. Anesthetic agents 5. Pain 6. Opiod medications 7. Hypoxia 8. HTN 9. Vestibular disturbances 10. Psychological factors 11. MI 12. Appendicitius, cholecystitis, pancreatitis, SBO, elevated ICP, Factors to consider that may predispose patients to a higher incidence: 1. Patient factors a. Female gender b. Non-smoker c. h/o motion sickness or h/o ponv d. Environmental: use of postop opioids, emetogenic surgery (type + duration) e. Obesity- believed to 2/2 excessive production of estrogen from adipose tissue and excessive stores of anesthetic agents w/I adipose. f. Conditions that predispose to delayed gastric emptying: DM, hypothyroidism, pregnancy, or other intrabdominal pathology. g. Type of surgery (i.e. gyn, abdominal, ophthalmologic, lap) Pharmacological treatment options: (see next page Table) Summary: --Pt’s at high risk of PONV should receive prophylaxis with a combo therapy. --when PONV occurs post-op, treatment should be admistered with an antiemetic from a different drug class from that given introp. Drug treatment of nausea and vomiting Drug Class Generic Name (Trade Name) Uses Recommended Doses Side Effects Phenothiazines Chlorpromazine (Thorazine) Uncommonly used for Nausea and Vomiting 10 - 25 mg q 4 - 6 po 25mg q 3h IV slow 25-50 mg q 4h IM 100 mg q 6-8h pr Hypotension Prochlorperazine (Compazine) Nausea and vomiting 5-10 mg tid po 2.5 10 mg IV slow infusion 5-10 mg q 4h IM 25 mg bid pr Hypotension Metoclopramide (Reglan) Gastroparesis 10-20 mg qid po 10-20 mg IV Extrapyramidal symptoms Cisapride (Propulsid) GERD 10-20 mg qid po Abd pain, diarrhea Drowsiness Trimethobenzamide (Tigan) Nausea and vomiting 250 mg tid/qid po 200 mg tid/qid IM 200 mg tid/qid pr Diarrhea, abd pain Erythromycin Gastroparesis 250 mg qid IV or po Abd pain Bethanechol Gastroparesis 10-25 mg qid po Abd pain Dymenhydrinate (Dramamine) Motion sickness 50 mg q 4h po Drowsiness Meclizine (Antivert) Motion sickness 50 mg q 24h po Drowsiness Cyclizine (Marezine) Meniere's disease 50 mg q 4h po 50 mg q 4h IV Drowsiness Promethazine (Phernagen) Motion Sickness 25 mg q 12h po 25 mg q 12h IV 12.5-50 mg q 12h IM 12.5-50 mg q 12h pr Drowsiness Dyphenhydramine (Benadryl) Motion Sickness 25-50 mg q 6h po Drowsiness Droperidol Post-op 2.5-5 mg IV Hypotension Sedation Extrapyramidal symptoms Haloperidol Rarely used 0.5-2 mg po Hypotension Sedation Extrapyramidal symptoms Anticholinergics Scopolomine (Transderm patch) Motion Sickness 1.5 mg patch q 3 days delivers 0.5g/day Drowsiness 5-HT3 Receptor Antagonists Ondansetron (Zofran) Post-op Chemotherapy 4 - 8 mg IV 32 mg one time dose Elevated LFTs Granisetron (Kytril) Chemotherapy 1 mg bid po 10 mcg/kg IV Headache Prokinetics Antihistamines Butyrophenones

![[Physician Letterhead] [Select Today`s Date] . [Name of Health](http://s3.studylib.net/store/data/006995683_1-fc7d457c4956a00b3a5595efa89b67b0-300x300.png)