Emergency Room Report: Flu Syndrome & Dehydration
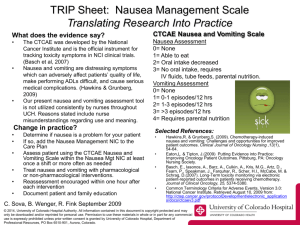
advertisement
SUTTER COAST HOSPITAL EXAMPLE - EMERGENCY ROOM REPORT, James H. Holmes, M.D. [DATE OF VISIT automatically added by iTran] HISTORY OF PRESENT ILLNESS: This 15-year-old young woman was brought to the emergency room by her mother because she has been ill for a couple days. She has had a sore throat, chills, fever, and myalgias, and she has been nauseated and has vomited several times. She has been complaining of severe pains all over in her back, arms, and legs. PAST MEDICAL HISTORY: She has a history of a heart murmur. She is not on any medications except some medicine for her recent "flu syndrome." ALLERGIES: No known drug allergies. REVIEW OF SYSTEMS: CONSTITUTIONAL: Chills and fever for the past couple days. HEENT: Sore throat. RESPIRATORY: Mild cough. Some pain with deep breathing. GI: Nausea and vomiting. No diarrhea. GU: No dysuria or frequency. PHYSICAL EXAMINATION: VITAL SIGNS: Temperature 37, pulse 144, respirations 24, and blood pressure 145/63, with O2 saturation on room air 99%. GENERAL: The patient is alert. She is in moderate distress. She is complaining of aches and pains. When asked where she hurts, she hurts all over, no specific area. HEENT: Eyes: Pupils equal and reactive to light. Extraocular muscles are intact. Throat: Minimal erythema in the posterior pharynx. NECK: Moves freely. There is no adenopathy. CHEST/LUNGS: A few rhonchi. No wheezes. No rales. ABDOMEN: Active bowel sounds. Soft. Nontender. BACK: No CVA tenderness. SKIN: Clear. There are no rashes. EXTREMITIES: No edema. There are good peripheral pulses. There is no pain with movement of all joints. DIAGNOSTIC STUDIES: White count is 10,500, 13 and 39 H&H, and platelets 185,000, with 90 segs, and 4 lymphs. Sodium 139, potassium 3.4, chloride 101, CO2 21, sugar 117, BUN 8, and creatinine 0.8. Liver function studies are normal. Pregnancy test is negative. Urinalysis: Specific gravity 1.010, no blood, no leukocytes. There were 2+ ketones. IMPRESSION: Flu syndrome with nausea, vomiting, and dehydration. COURSE IN THE EMERGENCY ROOM: The patient was given 2 liters of fluid IV; first liter normal saline and second liter LR. She was given morphine 2 mg IV and Phenergan 12.5 mg IV. The morphine was repeated x1. After approximately 8 hours in the emergency room, the patient felt much better. She was ambulatory. Her blood pressure was 100/63, pulse 117, respiratory rate 16, and O2 saturation 94% on room air. At this point she was discharged home with her mother. She was advised bedrest for the next couple days, clear liquids, broth, 7-up, soups, Gatorade, and follow up at the Del Norte Community Health Clinic. Recheck in the ER at any time if worse, increased pain, vomiting, or weakness, or if she is not fine in 2 days. She was given prescriptions for Phenergan and Vicodin. She is to take the Phenergan for nausea, and Tylenol or Vicodin for her myalgias and her pain.