Learning Objectives
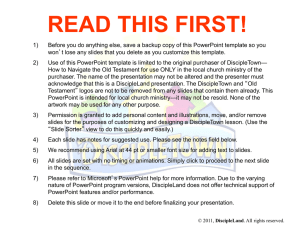
advertisement

Guided Lecture Notes Chapter 18: Disorders of Cardiac Function Learning Objective 1. Describe the function of the pericardium. Describe the anatomy and physiology of the pericardium (refer to PowerPoint Slide 3). Describe the etiology, pathology, clinical manifestations, and treatment of pericarditis (refer to PowerPoint Slides 4–5). Learning Objective 2. Describe the physiology of pericardial effusion. Define pericardial effusion. Identify causes of pericardial effusion, and describe the associated hemodynamic effects (refer to PowerPoint Slide 6). Learning Objective 3. Relate the cardiac compression that occurs with cardiac tamponade to the clinical manifestations of the disorder, including pulsus paradoxus. Define cardiac tamponade, and explain how tamponade results in the associated signs and symptoms (refer to Fig. 18-1). Discuss diagnosis and treatment of cardiac tamponade. Describe pulsus paradoxus (refer to PowerPoint Slide 9). Learning Objective 4. Compare the manifestations of acute pericarditis with those of chronic pericarditis with effusion and constrictive pericarditis. Describe the etiology, pathology, and signs and symptoms associated with acute pericarditis and chronic pericarditis with effusion and constrictive pericarditis. Learning Objective 5. Describe blood flow in the coronary circulation, and relate it to the metabolic needs of the heart. Identify the major coronary arteries (refer to Fig. 18-3). List factors that control and regulate coronary blood flow. Explain how the heart’s metabolic demands are met by coronary blood flow. Explain the pathology of coronary heart disease (refer to PowerPoint Slide 10). Differentiate between chronic ischemic heart disease and acute coronary syndromes (refer to PowerPoint Slides 12–13 and Fig. 18-6). Learning Objective 6. Characterize the pathogenesis of atherosclerosis in terms of fixed atherosclerotic lesions, unstable plaque, and thrombosis with obstruction. Differentiate between the pathologies of fixed atherosclerotic (stable) plaque, unstable plaque, and thrombosis with obstruction (refer to PowerPoint Slide 11 and Fig. 18-5). Learning Objective 7. Define the term acute coronary syndromes and distinguish among chronic stable angina, unstable angina, non–ST-segment elevation myocardial infarction, and ST-segment elevation myocardial infarction in terms of pathology, symptomatology, ECG changes, and serum cardiac markers. Describe angina and differentiate between stable, variant, and silent forms (refer to PowerPoint Slide 15 and Fig. 18-7). List the acute coronary syndromes (ACS). Differentiate between the ACS with regard to pathology, clinical manifestations, ECG results, and serum marker values (refer to PowerPoint Slide 16 and Fig. 188). List risk factors associated with acute myocardial infarction (AMI). Describe the etiology, pathology, signs and symptoms, diagnosis, and treatment of AMI (Refer to PowerPoint Slides 19–21 and Figs. 18-9, 18-10, 18-11, and 1812). Learning Objective 8. Compare the diagnostic measures and treatment goals for stable angina and the acute coronary syndromes. Describe how stable angina and ACS are diagnosed and treated. Learning Objective 9. Define and cite selected causes of myocarditis. Define myocarditis, and list possible causes. Discuss clinical manifestations, diagnosis, and treatment of myocarditis. Learning Objective 10. Characterize the pathogenesis and possible outcomes of viral myocarditis. Describe pathologic changes that occur in the heart as a result of viral myocarditis, and discuss the range of disease courses. Learning Objective 11. Define the term cardiomyopathy, and compare the heart changes that occur with dilated, hypertrophic, and restrictive cardiomyopathies. Define cardiomyopathy, and compare the causes of dilated, hypertrophic, and restrictive forms of the disease (refer to PowerPoint Slides 22–24 and Figs. 1814 and 18-15). Describe the pathology, clinical manifestations, and treatment of each type of myopathy listed above. Learning Objective 12. Distinguish between the role of infectious organisms and the immune system in infective endocarditis and rheumatic heart disease. Describe the etiology, pathology, clinical course, diagnosis, and treatment of infective endocarditis and rheumatic heart disease (refer to Fig. 18-16). Learning Objective 13. Compare the effects of rheumatic fever and bacterial endocarditis on cardiac structures and their function. Describe the cardiac damage associated with infective endocarditis and rheumatic heart disease. Learning Objective 14. Describe the relationship between the infective vegetations associated with infective endocarditis and the extracardiac manifestations of the disease. Differentiate between local and systemic effects produced by infective vegetative lesions. Explain how these effects result in the clinical manifestations associated with the lesions. Learning Objective 15. Explain measures that can be used to prevent infective endocarditis. Identify measures that can be used to prevent infective endocarditis. Learning Objective 16. State the function of the heart valves, and relate alterations in hemodynamic function of the heart that occur with valve disease. Differentiate between the two types of heart valves with regard to their anatomy and physiology. Explain hemodynamic changes that result when the heart valves do not function properly (refer to PowerPoint Slides 27–28). Learning Objective 17. Compare the effects of stenotic and regurgitant mitral and aortic valvular heart disease on cardiovascular function. Differentiate between stenosis and regurgitation (refer to PowerPoint Slide 30 and Fig. 18-17). Explain hemodynamic changes that result from stenosis and regurgitation (refer to Fig. 18-18). Learning Objective 18. Compare the methods of and diagnostic information obtained from cardiac auscultation, phonocardiography, and echocardiography as they relate to valvular heart disease. Explain how heart murmurs can be diagnosed (refer to PowerPoint Slides 34– 35). Describe diagnostic methods including auscultation, phonocardiography, and echocardiography. Learning Objective 19. Trace the flow of blood in the fetal circulation, and state the function of the foramen ovale and ductus arteriosus. Describe how fetal circulation differs from postnatal circulation (refer to Fig. 1821). Explain where the foramen ovale and ductus arteriosus are located, and describe their purpose (refer to PowerPoint Slide 40). Learning Objective 20. State the changes in circulatory function that occur at birth. Describe the hemodynamic changes that occur at birth. Learning Objective 21. Compare the effects of left-to-right and right-to-left shunts on the pulmonary circulation and production of cyanosis. Define shunt (refer to PowerPoint Slide 39). Differentiate between a left-to-right and a right-to-left shunt in terms of its effect on both pulmonary and systemic circulations (refer to PowerPoint Slides 41–42). Explain why a left-to-right shunt is considered to be a noncyanotic birth defect, and a right-to-left shunt is considered cyanotic. Learning Objective 22. Describe the anatomic defects and altered patterns of blood flow in children with atrial septal defects, ventricular septal defects, endocardial cushion defects, pulmonary stenosis, tetralogy of Fallot, patent ductus arteriosus, transposition of the great vessels, and coarctation of the aorta (refer to PowerPoint Slide 38). Describe the anatomic defects that occur in children with atrial septal defects, ventricular septal defects, endocardial cushion defects, pulmonary stenosis, tetralogy of Fallot, patent ductus arteriosus, transposition of the great vessels, and coarctation of the aorta. Describe the hemodynamic changes that occur in children with atrial septal defects, ventricular septal defects, endocardial cushion defects, pulmonary stenosis, tetralogy of Fallot, patent ductus arteriosus, transposition of the great vessels, and coarctation of the aorta (refer to PowerPoint Slide 43 and Fig. 1822). Learning Objective 23. Compare the role of infectious organisms in Kawasaki disease to that of the immune system. Describe the pathology of Kawasaki disease. Explain why the disease is believed to be of immunologic origin. Learning Objective 24. Describe the manifestations related to each phase—acute, subacute, and convalescent—of Kawasaki disease. Outline the clinical course of Kawasaki disease, and discuss diagnosis and treatment.