Update on parenteral lipids: therapeutic goals
advertisement

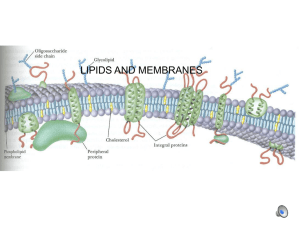
Update on Parenteral Lipids: Therapeutic Goals Bart Morlion, M.D. Dept. of Anaesthesiology /MPC, Universiteire Ziekenhuisen Gasthuisberg,, B-3000 Leuven, Belgium phone +32-26-348740, fax +32-26-348742, e-mail: bart.morlion@uz.kuleuven.ac.be Learning objectives To identify the biochemical nature of lipids To list three therapeutic goals for including lipids in parenteral nutrition To describe the energetic role of lipids To identify the need for essential fatty acids To list five mechanisms by which fatty acids alter immune and inflammatory responses To evaluate the theoretical advantages of different new lipid emulsions Introduction Total parenteral nutrition (TPN) is well established as a useful means of nutritional support when the enteral route cannot be safely or optimally used. Parenteral administration of nutrients has progressively evolved from a feeding modality to a complex form of metabolic care. Indeed, metabolic care of patients has traditional goals: to detect and to prevent malnutrition, to optimize the metabolic status, to reduce morbidity and the subsequent duration of recovery, and new goals focused on organ and system functions: to modulate inflammation and acute phase responses to support the metabolism of failing organs to maintain function and structure of the gastrointestinal mucosa to promote anabolism This line of reasoning is important in defining the therapeutic goals of parenteral lipids [1]. Biochemistry of Lipids Biological lipids are a chemically heterogeneous group of compounds composed of fatty acids and their common denominator is the insolubility in water. The physical properties of lipids are largely determined by the length and degree of unsaturation of the fatty acid chains. Different families of fatty acids (FA) can be defined: saturated FA (SFA; no double bond), mono-unsaturated FA (MUFA; one double bond on position 9; 9) and the poly-unsaturated FA (PUFA). The PUFA contain two ore more double bonds. On the basis of the position of the first double bond the 3 and 6 series can be identified. The biological functions of lipids are equally diverse. Lipids function as the primary source of stored energy, namely in mammalian adipose tissue. The average 70-kg human has approximately 12.5 kg of fat representing approximately 112.500 kcal. Apart from their energetic function lipids have several structural functions: they are an essential component of cell membranes, mechanically protect critical organs, and insulate against physical injury and heat loss. Other lipids, although present in relatively small quantities, play a crucial role as enzyme cofactors, electron carriers, light-absorbing pigments, hydrophobic anchors, emulsifying agents, hormones, and intracellular messengers. In addition, the plasma lipid system serves as an important carrier of lipids themselves, as well as of various lipid-soluble substances (e.g. vitamins A, D, E and K) to different tissues of the body [2,3]. Therapeutic Goals - Provision of Energy Lipids represent a valuable and compact (9 kcal/g) non-carbohydrate source of energy in parenteral nutrition, especially in patients with glucose intolerance or poor CO2 clearance. The high energy density of lipid emulsions, i.e. their high energy / volume ratio, requires the infusion of smaller volumes, thus helping to minimize the risk of fluid overload. Thereby the risk of metabolic complications associated with excessive glucose administration can be reduced, including hyperglycemia, water retention, and increased CO 2 production. Particles of the available lipid emulsions in general have characteristics similar to chylomicrons and are cleared from the blood with similar kinetic profiles [3]. The maximum lipid elimination capacity is about 3.8 g lipid/kg/day. At low lipid concentration the elimination rate is dependent upon the lipoprotein lipase concentration. Abnormal lipid clearance has been described in critically ill patients, but other publications report a normal or increased clearance of intravenous lipids, especially during sepsis. In patients with a metabolic stress response, the overall energy expenditure increases and the metabolism of carbohydrates, lipids and proteins are profoundly modified. In these hypermetabolic patients, lipid emulsions alone have minimal or no significant effect on nitrogen metabolism [4]. However, when combined with amino acids, lipids induce significant protein sparing effect although some of this effect can be attributed to the glycerol contained in the lipid emulsions. When used as a source of calories for critically ill patients, 15 up to 50 percent of total calories may be supplied as fat. In patients on TPN plasma lipids (triacylglycerols) should be measured before and during TPN. This is particularly important in patients who are at high risk of impaired fat clearance, such as those who are hyperlipidemic, diabetic, septic, or with impaired renal function, or those who are critically ill [5] These patients are susceptible to the fat-overload syndrome, which consists of hyperlipidemia, pyrexia, gastrointestinal disorder, anemia, a bleeding tendency, thrombocytopenia, and hepatosplenomegaly. In such situations lipid deposits may occur in the pulmonary capillaries, resulting in decreased pulmonary gas exchange and arterial hypoxemia, and can also involve the reticuloendothelial system. Therapeutic Goals - Provision of Essential Fatty Acids The human body is unable to synthesize either linoleic acid or -linolenic acid, the main components of the -3 and -6 series PUFA [2]. Essential fatty acid deficiency can develop in patients who receive fat-free parenteral nutrition for longer than 2 weeks. This condition is characterized by hepatomegaly, thrombocytopenia, impaired wound healing, hair loss and dry, desquamated skin. In order to prevent essential fatty acid (EFA) deficiency, linoleic acid must be provided as 2 to 4 percent of total calorie intake. Traditionally, lipid emulsions have been prepared using long-chain triglycerides (LCTs) obtained from either soybean or safflower oil and egg yolk phospholipids. Soy bean based emulsions contain a very high level of polyunsaturated fatty acids (PUFAs). The need for EFA is met already by small volumes of such emulsions [4]. It has been suggested that high levels of -6 PUFA may impair host defence and that TPN therefore could increase infectious complications in certain types of patients. Therapeutic Goal - Modulation of Immune Function Malnutrition is associated with a depressed function of the immune system which can be ameliorated non-specifically by adequate nutrition. In addition, fatty acids can specifically modulate function of the immune cells. The administration of lipids influences phospholipid composition and fluidity of cell membranes, thereby affecting essential funtions like enzyme activities, transport-receptor and regulatory functions [6,7]. These essential functions also relate to the formation of eicosanoids and cytokines. The modulation of eicosanoid and cytokine biology by lipids provides, in theory, an intervention strategy by which cytokines and eicosanoids can express their beneficial effects rather than their potentially damaging properties in patients [7]. Besides these effects on the cell membranes the composition of fatty acids also modifies the serum lipoprotein profile, which influences the activities of the immune cells. Fatty acids are also the ligands for the peroxisome proliferator-activated receptors. Those receptors regulate a variety of anabolic and catabolic functions in different cell types. Taken together, there is a theoretical case for tailoring the FA composition of new lipid emulsions to the needs of the individual patient and the organ failure profile. As a consequence, a variety of lipid emulsions based on either medium-chain triglycerides (MCT), or olive oil, or fish oil (-3 PUFA), or structured triglycerides (containing both long and medium chain FA on the same glycerol backbone) have been developed and studied during the last decade. Currently, most of these emulsions are commercially available. One principle common to many new emulsions also is the reduction of the high PUFA load of soybean oil. In emulsions containing olive oil, which is rich in the -9 MUFA, oleic acid may offer an immunologically neutral alternative to -6 PUFA rich oils. In MCT/LCT emulsions there is a 50% reduction of -6 PUFA by comparison to pure soybean oil based LCT emulsion [8]. Futhermore, MCTs are not dependent on carnitine for transport into the mitochondria of skeletal muscle and therefore may be more efficiently oxidized than LCTs. Another reason, apart from immunological considerations for reducing the high PUFA load in lipid emulsions is oxidative stress. Indeed, increasing PUFA intake increases oxidative stress, which, if not counterbalanced by antioxidant nutrients, can cause lipid peroxidation and tissue dammage. Thus, the antioxidant nutrient status of our patients is of critical significance in determing the effects of PUFA on immune and inflammatory responses. During the past 15 years, numerous studies have investigated the effects of -3-PUFA on human immune and inflammatory responses. Anti-inflammatory and antithrombotic properties of -3-PUFA have been observed in various experimental and clinical studies. These effects seem to be related to the incorporation of eicosapentaenoic acid (EPA) into cellular membrane lipids and its subsequent metabolisation. After inflammatory activation EPA is released besides arachidonic acid (AA) and competes with AA for metabolisation via the cyclo- and lipoxygenase pathway. Compared to AA the derivatives of EPA have less pro-inflammatory and chemotactic characteristics. Thus, it seems plausible to use -3 PUFA supplements in order to attenuate the inflammatory response by modulating the generation of lipid mediators during inflammation. At present, the optimal fatty acid composition of lipid emulsions for any particular group of patients remains to be elucidated, particularly so when modulation of the immune function is aimed for. Not surprisingly, there are in fact marked differences in the host response to trauma, elective surgery and the different types of life-threatening sepsis seen in the ICU. References 1. Chioléro R, Kinney JM. Metabolic and nutritional support in critically ill patients: feeding the whole body or individual organs? Curr Opin Clin Nutr Metab Care 2001; 4: 127 -130 2. Lehninger AL, Nelson DL, Cox MM. Principles of Biochemistry, 2nd edition. New York: Worth Publishers, 1993 3. Carpentier YA, Dupont IE. Fatty acids, lipoproteins, and lipid emulsions. In: Pichard C, Kudsk K (eds). From nutrition support to pharmacologic nutrition in the ICU. Berlin: Springer, 2000: 38-53 4. Kinney JM, Furst P, Elwyn D, Carpentier YA. The intensive care patient: In: Kinney JM, Jeejeebhoy KN, Hill GL, Owen OE (eds) Nutrition and metabolism in patient care. Philadelphia: WB Saunders, 1988: 656-661 5. Crook MA. Lipid clearance and total parenteral nutrition: the importance of monitoring plasma lipids. Nutrition 2000; 16: 774-775 6. Kelley DS. Modulation of human immune and inflammatory responses by dietary fatty acids. Nutrition 2001; 17: 669673 7. Grimble RF. Nutritional modulation of cytokine biology. Nutrition 1998; 14: 634-640 8. Gelas P, Cotte L, Poitevin-Later et al. Effect of parenteral medium- and long-chain triglycerides on lymphocyte subpopulations and functions in patients with acquired immunodeficiency syndrome: a prospective study. J Parent Enteral Nutr 1998; 22: 67-71 Further reading Rombeau JL. Clinical nutrition: Parenteral nutrition, 3rd edition. Philadelphia: WB Saunders, 2000 Pichard C, Kudsk KA. From nutrition support to pharmacologic nutrition in the ICU. Update in intensive care and emergency medicine 34. Berlin: Springer, 2000