2.2.1 The Central Database
advertisement

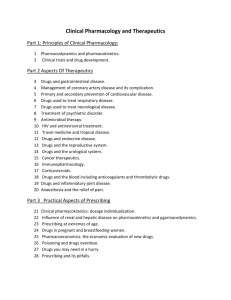
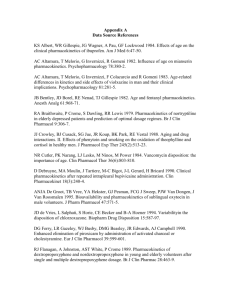
Background and User’s Guide Comparative Child/Adult Pharmacokinetic Database based upon the Therapeutic Drug Literature Dale Hattis, Abel Russ, Prerna Banati, Mary Kozlak, and Rob Goble Clark University and Gary Ginsberg and Susan Smolenski Connecticut Department of Public Health September, 2001 EPA/State of Connecticut Assistance Agreement #827195-0, Dr. Bob Sonawane, EPA Project Monitor Table of Contents 1.0 Introduction ………………………………………………………………… 1 1.1 Goals of the Current Project …..…………………………………… 2 2.0 Methods and Approaches Used for Database Development ……………….. 2.1 Compilation and Description of the Database ………...………... 2.1.1 The Central Database …………………………………………….. 2.1.2 Data Files from Individual Papers ……………………………….. 2.1.3 Files Documenting the Regression Analysis ……………..…….. 3 3 8 12 13 3.0 References ……………………………………………………………………18 2 1.0 Introduction The risks that children incur from environmental chemicals may be quite different than risks in adults due to a number of factors: 1) the degree of exposure tends to be greater in young children due to a greater inhalation rate and food ingestion rate (particularly for certain foods) per body weight, and greater contact with soil, house dust, and other media which may contain contaminants (USEPA, 1997); 2) once exposure has occurred, the pharmacokinetic (PK) handling of chemicals is likely to differ from that in the adult with respect to chemical half-life, clearance, protein binding, and volume of distribution (Morselli, 1989; Besunder, et al., 1988; Kearns and Reed, 1989) 3) the sensitivity of rapidly developing tissues and systems in neonates and young children may differ from that in adults leading to pharmacodynamic (PD) differences (Faustman, et al., 2000; Vesselinovitch, et al., 1979). While all three areas of child-adult differences need to be addressed, the focus of the current project is the second area - the potential for PK differences to play a significant role in modifying risks to children. Physiologic and metabolic factors govern the PK processes of chemical absorption, distribution, metabolism, and excretion. These processes in turn determine the effective internal concentration of a chemical and its metabolites, some of which may be more or less toxic than the parent compound. Given the differences in physiology (e.g., body size, lipid and water content) between adults and children and the immaturity of many systems in young children (e.g., liver metabolizing enzymes, plasma protein binding, renal excretion, bloodbrain barrier function), it is likely that substantial PK differences exist in young children, at least at certain age groups and for certain chemicals. PK differences across human receptors are currently factored into the risk assessment process. The existing approach for non-cancer risk assessment is to use a 10 fold uncertainty factor to reduce exposure for potential inter-individual differences across the human population. This 10 fold factor can be thought of as constituting a half log (3.2) factor for PK differences among human receptors and another half log factor for PD differences (Renwick, 1998). The 1 3.2 fold PK factor is expected to account for racial, ethnic, gender, genetic, and age differences, as well as inter-individual differences due to disease states, and intake of drugs. This latter factor can modify chemical metabolism and fate via enzyme induction, displacement from serum proteins, and other PK mechanisms. It should be noted that since uncertainty factors are traditionally not used in cancer risk assessment, there is no attempt to account for PK variability across individuals in such assessments. 1.1 Goals of the Current Project The primary goal of the current project is to define the types of parameters and range of ages where PK differences between children and adults that may be of greatest importance to risk assessment. To accomplish this goal, a children’s PK database was constructed from the therapeutic drug literature. The pharmacokinetics of many drugs have been evaluated in children to determine the dose levels most appropriate for this age group. When combined with adult PK studies of the same drugs, direct comparisons between adult and child PK can be made. By evaluating PK datasets across chemicals with differing structures and clearance mechanisms (e.g., renal excretion, Phase I metabolism, Phase II metabolism), it is anticipated that differences between adults and children in terms of key metabolism and removal pathways will become evident. In addition to evaluating clearance pathways and specific age groupings for possible differences with adults, the current project uses the children’s PK database to evaluate the degree of inter-subject variability seen in the children’s and adult PK datasets. Given that children are rapidly growing, any pre-set age category will include individuals along a developmental continuum. This creates a type of PK variability that is likely to be more important in children than in adults, and thus is critical to identify,quantitate, and incorporate into children’s risk assessments. By evaluating both the difference in mean value of PK parameters (e.g., clearance, half-life) and also the inter-subject variability in these parameters across ages, this research endeavors to provide some perspective on whether the 3.2 fold uncertainty factor intended to account for PK variability in the human population is sufficient for children. 2 This User’s Guide provides information on how the database is constructed so that the key information can be accessed and utilized. Manuscripts recently submitted to peer review journals further describe the database and 1) how the mean values of children’s PK paramaters compare to adult levels (Ginsberg, et al., 2001); and 2) how inter-subject variability among children in specific age groups creates a distribution of PK function in relation to the mean function as seen in adults (Hattis et al., 2001). These papers also describe ways in which the current database may be useful in children’s risk assessments and places the assembled data in the context of other children’s PK summaries (Renwick, 1998; Renwick et al., 2000; Morselli, 1989, Kearns and Reed, 1989; Gupta and Waldhauser, 1997; Cresteil, 1998). 2.0 Methods and Approaches used for Database Development This project involved identification of chemicals from the therapeutic drug literature having pertinent PK data for children, obtaining and evaluating the primary studies to extract key data, obtaining comparable data for adults, organizing the data into a spreadsheet database, and analyzing the data across age groups. The key data obtained from reviewed studies included: number, gender, and age of subjects, type and number of doses, PK findings in terms of half-life, clearance, volume of distribution, peak and area-under-the-curve blood concentrations, and individual subject data or group variability statistics. The various steps involved are further described below. 2.1 Compilation and Description of the Database Computerized literature searches were conducted to find references to publications describing children’s pharmacokinetics, using search words such as neonate, infant and children and crossing these with terms such as pharmacokinetics, metabolism, distribution, excretion. Additionally, a pediatric pharmacology text (Yaffe and Aranda, 1992 ) and review articles on children’s PK (Anderson, 1997; Jacqz-Aigrain, 1996, Renwick, 1998) were examined to identify chemicals for which PK datasets exist for children. Through these sources, a list of approximately 100 chemicals from the therapeutic drug literature were identified as having at 3 least some PK data in children. A subset of 44 chemicals was selected for more detailed analysis based upon being able to obtain the original data sources, these sources having a reasonable number of subjects, the availability of data for pertinent age groups (especially very early life stages), and considerations of clearance mechanism. The list of chemicals contained in the database and major clearance mechanisms are shown in Table 1. Clearance mechanisms were identified from pharmacology texts (Dollery, 1999, Goodman and Gilman, 1990) a key review article (Bertz, 1997), as well as primary literature for individual compounds as shown in the table. The table provides an indication of the amount of human metabolism of each chemical, with the information generally from PK studies in adults. Most chemicals are cleared by multiple pathways but typically one or two routes of metabolism and elimination predominate. The table provides an estimate of the percentage of parent compound processed by the major fate pathways. The table indicates that of the 44 chemicals contained in the database, 8 chemicals (antibiotics: ampicillin, gentamicin, pepracillin, ticarcillin, tobramycin, vancomycin; other drugs: cimetidine, furosemide) are primarily excreted unchanged in urine and so half-life or clearance information on these chemicals can be indicative of renal function at different ages. Regarding biliary function, bromosulfophthalein (BSP) is the best indicator chemical in the current database given that at least some of dosed BSP is excreted unchanged in bile. BSP has traditionally been used as a clinical marker of hepato/biliary function. However, a portion of dosed BSP is conjugated with glutathione prior to excretion in bile so the overall BSP clearance from blood is actually a composite of these two pathways (GSH conjugation, biliary clearance of unchanged BSP) (Fehring, et al, 1989). Chemicals for which cytochrome p-450 (CYP) Phase I metabolism predominates are well represented in the database, with numerous chemicals having some form of CYP as the primary route of disposition. The most prevalent type of CYP substrate are those chemicals metabolized by CYP3A (alfentanil, fentanyl, ketamine, lidocaine, midazolam, nifedipine, quinidine, remifentanil, teniposide, triazolam), which is the predominant type of CYP in human liver. Other types of CYPs for which information can be gained from chemicals present in the database 4 are CYP1A2 (bupivacaine, caffeine, mepivacaine, theophylline), and the CYP2C family (amobarbital, tolbutamide). Some of the assignments made in the table are based upon close structural analogy with a chemical or a group of chemicals for which CYP specificity is known (e.g., remifentanil, mepivacaine). Finally, chemicals cleared primarily via Phase II conjugation pathways without the need for prior Phase I metabolism are also included in the database. Glucuronidation substrates total 6 (lorazepam, morphine, oxazepam, paracetamol, valproic acid, zidovudine), while sulfation (metoclopramide) and glutatione conjugation (busulfan, BSP) substrates are also contained in the database. In some cases these assignments may best be described as general Phase II substrates rather than substrates for a single conjugation pathway. This is exemplified best by paracetamol, which is a candidate for glucuronidation, sulfation, and glutathione conjugation, with a shift in pathways if the preferred substrate is not available (Besunder, et al., 1988). 5 Table 1. Clearance Pathways for Chemicals in Children’s PK Database Chemical Alfentanil Amobarbital % Metabolized >90% > 70% Ampicillin Antipyrene Bromosulfphthalein Bupivacaine Busulfan Caffeine Carbamazepine Chloral Hydrate Cimetidine Metabolic Pathways CYP3A4 (70%) predom. Cyp 2C19; some gluc. Basis Bertz, 97 Analogy w/related barbs;Bertz,97;G&G, 90 Bertz, 97 Engel, 96; Tanaka, 98 Fehring, 1989 Analogy with ropivicaine; Dollery, 99 Dollery, 99; Ohmori, 98 Bertz, 97 Dollery, 99; Gibbs, 97 Henderson, 97 Bertz, 97 low (75-90% renal) high not available approx. 85% >90% >90% >90% >90% <30-40%; (70% renal) Clavulanic Acid 50 to 60% Cotinine extensive Dapsone 80-90% Dichloroacetic acid >90% Ethanol >90% Fentanyl >90% Furosemide low (50-80% renal) Gentamicin low (>90% renal) Ketamine 90% Lidocaine >90% Lorazepam >90% approx. 85% Mepivicaine Metoclopramide 70% Midazolam >90% Morphine >90% Nicotine >90% >90% Nifedipine Oxazepam >90% Paracetamol (acetamin) >90% Piperacillin low (70% renal) Quinidine >70% Remifentanil >90% --multiple p450s: 1A2, 2B6, 2C, 3A4 biliary excretion; GSH conjugation 1A2 (major); Cyp 3A4 (minor); 40% GSH conj.; various other metab Cyp1A2 (90%)>>2E1 Cyp 3A4 ADH most important Possible minor role for Cyps Unknown Cyp 2A6 and glucuronidation N-acetyl (50%), unknown cyp, gluc. Cyp hydrolysis; redn via radicals ADH>Cyp 2E1>Catalase Major: Cyp 3A4; Minor: 2D6, 2C8/9 Glucuronidation 20-50% --Cyp 3A and 2D; others possible Cyp 3A major; Cyp 1A2, 2B1 (minor) Glucuronidation without Phase I 1A2 (major); Cyp 3A4 (minor); Sulfation (35%) > gluc (<20%) > Cyp CYP3A (primary) Glucuronidation without Phase I Cyp 2A6 - 80%; some glucuron. CYP3A4 (primary) Glucuronidation without Phase I Gluc (60%)>sulf (35%)>Cyp1A2,2E1 --Cyp3A (>50%) Cyp3A4 (major); 2D6, 2C8/9(minor) Dollery, 99 Dempsey, 2000 Dollery, 99 Stacpoole, 98 Dollery, 99 Bertz, 97; Guitton, 97 Bertz, 97 Goodman&Gilman, 90; Bertz, 97 Dollery, 99 Dollery, 99 Dollery, 99; Bertz, 97 Analogy with ropivicaine; Dollery, 99 Bertz, 97 Bertz, 97 Bertz, 97 Dempsey, 2000 Bertz, 97 Bertz, 97 Bertz, 97 Goodman & Gilman, 90 Bertz, 97; Tanaka, 98 Teniposide Theophylline Thiopentone 50% >90% >90% Cyp3A (primary) Cyp1A2 (>70%) > 2E1 > 3A4 predom. Cyp 2C19; some gluc. Ticarcillin Tobramycin Tolbutamide Triazolam Trichloloethanol Valproic acid Vancomycin Zidovudine <10% (92% renal) <10%, (90% renal) >90% >90% extensive >90% low (75-90% renal) 60-80% Analogy / etoposide, Bertz, 97, G&G,90 Bertz, 97 Analogy w/related barbs;Bertz,97;G&G, 90 Goodman & Gilman, 90 Goodman & Gilman, 90 Bertz, 97 Bertz, 97 Mayers, 91; Henderson, 97 Bertz, 97 Bertz, 97 Bertz, 97 ----Cyp 2C9/10 Cyp 3A Glucuronidation Glucuronidation (20-70%)>Cyps --Glucuron. (major) > Cyp3A (minor) 6 Analogy w/fentanyl & other congeners; Guitton,97 2.2 Database Structure and Contents The database is available in a series of Microsoft Excel 95workbooks as briefly described in the following listing. Additional details regarding several key workbooks and worksheets within each workbook are provided thereafter. Workbook ”chldpk9_01anal.xls” “Central Database” worksheet: summary compilation of entire child and adult data organized by drug, parameter, and age group. It provides basic information on study design, group mean summary data, and literature references. The final two columns of this worksheet provide the workbook and worksheet locations of any detailed calculations we did in the analyses of individual papers. These summary data from this database were used in the regression analyses. “Full Database” worksheet: expanded version of the Central Database in which dummy variables for drug name, clearance pathway, and age group are included. “Data Summaries” worksheet: provides summary tables of the content of the Central Database in terms of the number of data records available for different age groups, clearance pathways, etc. It also shows calculations of the imputed values we used for the small numbers of cases where data on standard deviations or numbers of subjects were missing from the original literature sources. Because different pharmacokinetic parameters had different variability, these imputation calculations were done separately for elimination half lives, clearances, etc. “T1/2 Database” worksheet: This is the portion of the “Full Database” that contains elimination half-life data. “Clearance Database” “Vd Database” “Cmax Database” and “AUC Database” worksheets: Similarly these are the subsets of the “Full Database” pertaining to the different types of pharmacokinetic measurements. 7 “Regression Results” worksheet: presentation of regression statistics for the various parameters analyzed and modes of analysis. “Clearance Category Anal” worksheet: This shows a classification of the chemicals by adult clearance—designed to distinguish chemicals whose metabolism might be appreciably limited by liver flow from less well extracted chemicals whose elimination rates are a smaller fraction of liver flow. This worksheet also contains regression results for the elimination half-life parameter for the chemicals separated into the adult clearance rate categories. Workbooks “chldpkChildOnlyStudies.xls” “chldpk-Adult.xls” and “chldpkCombined.xls”: These Excel worksheets include the detailed documentation of the data as presented by the original source papers, and the calculations made to go from these data to the entries in the Central Database. These workbooks are organized by drug, with each worksheet within a workbook containing data describing a single PK study for that drug. Workbook “chldpk-Individ.xls”: This workbook documents the individual ratios of child/adult values for clearances and elimination half lives, in cases where data for individual subjects were provided by the original authors. 2.2.1 The Central Database The Central Database summarizes the mean values of pharmacokinetic parameters measured in groups of children of various ages with similar types of data also presented for adults. The source references were located from a combination of searches on Medline and Toxline, and reviews of citations to relevant data in secondary sources. Qualifying datasets were included if they were based on measurements in at least four subjects, with a distinct preference for datasets that also provided information on the numbers of subjects studied and some measure of dispersion such as a standard deviation or a standard error (or, even more preferred, the raw individual values for which distributional statistics could be calculated). 8 Generally, each of the 340 lines of the “Central Database” represents the arithmetic average values found in a particular study for a particular age group—although in several cases (particularly for adult data) values from two or more studies have been combined. The Central Database contains all the summary data and so is a convenient listing of the available data for children and adults for the chemicals contained in the database. The fields (columns) of the file are described in more detail below. An additional version of the Central Database, labelled “CDforPrint.xls” is also included. This excel file has the same information as the main Central Database file but with some columns hidden and notations simplified to make the spreadsheet easy to print on 8.5 x 14” paper. A. Chemical—The name of the drug most commonly used in the studies contributing data. B. Predominant Fate Pathway —The predominant mode of elimination of the drug from the body inferred from general sources [e.g., Dollery, 1999; Goodman and Gilman, 1990] and in several cases from the paper contributing data. C. Metabolic Type Label – this hidden column contains the fate pathway assignment for each chemical to be used in subsequent regression runs. D. Parameter—Indicating the type of measurements made, including clearance “C”; elimination half life “T1/2” (generally for the second or terminal phase if more than one compartment was indicated in classical pharmacokinetic analysis); Volume of distribution “Vd” (generally at steady state, if given); the maximum concentration achieved in the blood after dosing “Cmax”, or the integrated Area Under the Concentration X time curve “AUC” after dosing. E. Parameter Standardized - this column reflects the standardized label given to the column for the purposes of assigning parameters to different regression analyses. F. Units—These are the units used to express the data. In many cases it was necessary to convert the original data given in the source papers to common sets of units to assure comparability across different studies—generally clearances were expressed in mg 9 chemical/(min-kg body weight); elimination half-lives were expressed in hours, and volumes of distribution were expressed in liters per kilogram of body weight, etc. G. Mean—The arithmetic average of the values of the parameter that were given. H. Log(Mean)—This hidden column contains the Log10 of the arithmetic mean. I. Standard Error—Essentially this functions like a standard deviation, but applied to the mean of some number (N) of values. It is calculated as the standard deviation divided by the square root of N. Sometimes these values were given directly by the source paper—in other cases they were calculated from data in the source paper. J. Coefficient of Variation – this column shows the degree of variability in the data for this line, expressed as the standard deviation divided by the group arithmetic mean. K. “In Var Weight (Mean/SE)^2—this column contains the “inverse variance weight” - a statistical weight used in some of the regression analyses. It is calculated as the square of [the mean of the parameter (column F) divided by the standard error (column G)] squared. Dividing the mean value of the parameter by the standard error in this procedure creates a unitless quantity that, when squared, represents the reciprocal of the variance of the mean. In several cases, where the standard error in column G is listed as “not given” the corresponding entry in column H is “Value!”. In these cases, the entries for this column were imputed from other information specific to the observed uncertainty in the same parameter measured in other studies. The detailed calculations are provided in the “Data Summaries” worksheet, colmuns AT through BE. L. “Sqrt N Weight”—This is an alternative weight used in some regression analyses. One possible concern with the inverse variance weight in column H is that it depends heavily on the authors’ reports of standard deviations of their measurements. Because these standard deviations are based on relatively modest numbers of data points they are themselves subject to appreciable statistical uncertainty. Therefore this column is a weight that depends only on the number of subjects in the group giving rise to the data—N0.5. 10 M. N—This is the number of subjects studied to give rise to the reported average. In some cases this information was not supplied in the source paper, and a value of 9 (shown in italics) was imputed from the median study size of papers that did provide their N’s. Of 340 total data sets, there were imputed values for group size (median = 9) in only3 cases. N. Child Age Range shows the range of ages of the children studied or “adults” if the group consisted of people over 18 years of age. O. Mean Child Age (yrs) is the mean age of the children subjects that was reported or could be calculated. P. Reference gives short references to the source paper, allowing identification of the full references in the bibliography. Q. (Blank) R. (Blank) S. (Blank) T. (Blank) U. Workbook—Shows the Excel workbook containing the detailed documentation (for cases with stars, the mean and standard deviation/standard error data were entered into the Central Database without separate calculations). There are three workbooks—one for child data; one for adult data, and one for papers that combined child and adult data (child.xls, adult.xls, and combined.xls, respectively). V. Worksheet—This gives the specific worksheet for the detailed calculations within the workbook cited in column U. An overview of the contents of the Central Database is provided in the spreadsheet titled Data Summaries, and also in one of the submitted manuscripts (Ginsberg, et al., 2001). Age groupings were developed in an effort to capture the rapid physiological and biochemical/metabolism changes that occur in the first weeks to months of life. Given the 11 evidence that changes occur in liver cytochrome P-450 (CYP) enzymes and other systems within the first hours to days of life (Cresteil, 1998; Tanaka, 1998), it was important to determine whether PK changes could be detected in the first week vs. the 1 week to 2 month age comparison. Further, the fact that premature infants have many underdeveloped systems at birth, it was important to evaluate them as a separate group. The age groupings beyond the neonatal period were intended to represent a developmental continuum, although the number of groups possible and the age cutoffs were a function of the data available for these ages (i.e., there would be no point in having an age group with too few data points for statistical evaluation). A large age group encompassing 10 years was used to characterize children beyond the toddler stage up until adolescence. This appeared reasonable based upon initial judgements that there was not a large degree of variability in the PK parameters under study over this broad age range. Further, there was not much data available for older children. In summary, the age groupings used to organize and summarize the children’s PK data are as follows: Neonates (first week of life, full term); Neonates (first week of life, premature); Newborns (1 week to 2 months of age); Early infants (2 –6 months of age); Crawlers/Toddlers (6 months – 2 yrs of age); Pre-Adolescents (2-12 yrs of age); Adolescents (12-18 years of age); Adults Of course, individuals within any age group are at slightly different developmental stages, with such inter-individual differences evaluated in the variability analysis (Hattis, et al., 2001). 2.2.2 Data Files From Individual Papers Three Excel workbooks comprise the “original study” database which represents an extraction of key data from the PK studies themselves. The information extracted included data on study protocol, subject ages, group size, and PK results. The three workbooks consist of papers that (1) provided only adult data for comparison (“chldpk-adult.xls”) (2) provided only data for groups of children, (“chldpkchild.xls”) or (3) provided data for both adults and children (“chldpk-combined.xls). Within each workbook, analyses of specific papers are filed in individual worksheets titled with the name of the chemical/drug studied. In addition, some 12 worksheets—usually labeled “comb” for combination—document our aggregation of data across different experimental groups. In most cases the methodology used is self-explanatory—simple unit conversions (to obtain data in comparable units), and calculations of means, standard deviations, standard errors, and geometric standard deviations (the latter as measures of interindividual variability, usually represented on the spreadsheet in bold face, and calculated as the standard deviation of the logarithms of individual parameter values). Where combinations were made across studies, in cases where the individual data points were not available, combined group standard errors were calculated from a weighted average of the variances indicated for the measurements in each experimental group (for an example, see the “Alfentanil” worksheet in the “chldpkChild.xls” workbook, cell F14). 2.2.3 Files Documenting the Regression Analysis While one may be able to make general inferences of child/adult PK differences from data presented in the Central Database, regression analysis was used to develop a statistical description of trends in mean parameter values over different age groups. The main documentation for regression analyses is contained in the spreadsheet labeled “Regression Results”. Regressions were run in a multiple regression engine from SAS, Inc. called JMP, Version 3.1.6. The regression analysis was conducted across all chemicals in the database by normalizing the results for each chemical back to a single reference chemical (theophylline was arbitrarily chosen). In this way, the inherent differences between chemicals in terms of clearance or half-life were normalized to the respective values for theophylline. The regression equation (see below) used dummy variables to normalize for chemical identity against theophylline. This then allows the inter-age differences in clearance or half-life to be evaluated for all chemicals in the database simultaneously. To accomplish this the regression equation also used dummy variables to normalize for age group relative to adults. The regression coefficient for each age group represents that age group’s composite (across all chemicals) ratio compared to adults with respect to that PK parameter. Since the regression equation is performed as a Log function, the antilog of the regression coefficient provides the ratio to adults. 13 The worksheet labeled “Full database” consists of the basic data contained in the Central Database file discussed earlier, plus a few items added in preparation for the regression analysis: Columns B through AS are a series of “dummy” (0 or 1) variables for each drug/chemical in the analysis—given a value of “1” if the chemical corresponds to the label in row A and “0” if it doesn’t. This allows the regression analysis to control for differences among chemicals in the typical values of studied parameters (e.g., clearance, half life) and draw overall inferences about the multiplicative differences associated with specific age categories. Columns AV through BH are similar “dummy” variables designating different predominant modes of elimination. In the actual regression these variables were mainly used for quick sorting of the database, rather than to control for elimination types as was done for the chemical specific dummies. Columns BU through CB provide another set of “dummy” variables related to the age group of the children (or adults) included in each data group. The classifications are based on either the mean age or the center of the age range given in the previous columns. Once again, the value of “1” is used to designate that the targeted age group is being analyzed and “0” if some other age group is represented. Column BO provides calculations of coefficients of variation (that is, the standard deviation divided by the mean) in cases where standard errors or individual data have been provided by the source reference. The results in this column are used in later calculations of imputed values for the inverse variance weights for data groups where the source reference did not provide individual data or measures of dispersion such as standard errors or standard deviations. The worksheet “Data summaries” characterizes the database by chemicals, parameters, numbers of subjects, etc., and provides the foundation for the data imputation calculations. Unfortunately, the number of subjects in a group was not available in all cases. Based upon the number of subjects per study group where this information was provided, the judgment was made that there was no clear evidence of a tendency for median group sizes to be appreciably larger for some parameters than for others. Therefore the overall median value of 9 14 was used for assigning statistical weights for all data groups where the source paper did not provide this information. The regression analysis was run in several formats to test the effects of prioritizing or weighting those papers that had larger numbers of subjects (“N”) or less variability. Without such weighting, the regression technique gives equal weight to studies of varying robustness and statistical confidence. To weight according to number of subjects per study group, the square root of N was used (N=9 used as default if no N given). To weight according to variability the “inverse variance weight” (see Central Database, Column H description) was used. This statistic is an indicator of the coefficient of variation (arithmetic standard deviation divided by the arithmetic mean) and so is a useful index of the spread of the data around the mean value. Since not all papers provided dispersion information (standard deviation or standard error) to include such papers in our variance weighting procedure, it was necessary to provide a default estimate of study variability. To gain some insight on this, Table 2 shows the median coefficients of variation across measurements of different PK endpoints. 15 Table 2 Median Coefficient of Variation for Different PK Endpoints PK Parameter Median Coeff. of variation* AUC 0.3777 Clearance 0.3707 Cmax 0.3004 t1/2 0.3086 Vd 0.3398 All 0.3428 *Coefficient of variation is the arithmetic standard deviation divided by the arithmetic mean. The table indicates differences in coefficients of variation across these different endpoints which might not be entirely negligible, which suggests that different parameters could be subject to systematically different amounts of experimental measurement error per individual studied. Therefore in our imputations for the inverse variance weights we elected to use the parameterspecific median coefficients of variation for cases where the source paper did not provide dispersion information . The imputation calculations themselves are documented in the “inverse variance weight” columns of the worksheets which yields the final databases used for regression analyses for each individual parameter (see, especially, the worksheets labeled “Clearance database”, “T1/2 dataabase, and “Vd database”). The worksheet labeled Regression Results” in this workbook documents our full regression results. For each parameter we used a conventional multiple regression model of the form: Log(Mean) = B0 + B1*(1 or 0 for chemical 1) + B2*(1 or 0 for chemical 2) + … + Ba*(1 or 0 for age group 1) + Bb*(1 or 0 for age group 2) + … 16 In this model, the chemical-specific “B’s” correct for differences among chemicals in average clearance (or other parameter) relative to a specific reference chemical (e.g., theophylline). Similarly, the age-group-specific “B’s” assess the average log differences between each age group and the reference group (adults). In the table provided for each regression run, the central estimates of the “B” coefficients are provided under the column labeled “estimate”, with conventional standard errors, t statistics, and P values provided in subsequent columns. The key information for each table is contained in the column labeled “Antilog”. This is the best estimate of the ratio of the values of each parameter found for the data in each age group, relative to the corresponding values for adults. It is calculated simply as 10B where B is the regression estimate for the age group involved. The three types of regression runs done for each parameter are presented as follows: (1) simple unweighted regressions are provided in columns A through F; (2) Square Root of N weights were used for the results in columns H through M; and finally (3) full Inverse variance weights were the basis for the regressions reported in columns O through T. It can be seen from the R values and the P values for the age group coefficients that the regressions using the most sophisticated inverse variance weights performed appreciably better, although the central tendencies of the results of all the weighting schemes are similar. Results of regression runs for different parameters and data subsets are provided in different sets of rows of the worksheet. Clearance results for the whole data set are provided beginning at Row 10, half-life results for the whole data set begin at row 528, Vd results for the whole data set begin at row 1200, and AUC results begin at row 1600. There was insufficient data for similar regression analyses of Cmax. Finally, the remaining sections of the spreadsheet show the results of regression runs for the Clearance and T1/2 parameter for various subsets of the data by predominant elimination types (renal clearance, “Any P450”, and conjugation). For these runs, only the best-performing inverse square weightings were used. 17 3.0 References Anderson, B. J., McKee, A. D., and Holford, N. H. G. (1997) Size, Myths and the Clinical Pharmacokinetics of Analgesia in Paediatric Patients. Clin. Pharmacokinet. 33:313-327 (1997). Aranda, J. V.,k Sitar, D. S., Parsons, W. D., Loughnan, P. M., and Neims, A. H. (1976) Pharmacokinetic aspects of theophylline in premature newborns. N. Engl. J. Med. 295: 413416 Aranda, J. V., Perez, J., Sitar, D. S., Collinge, J., Portuguez-Malavasi, A., Duffy, B., and Dupont, C. (1978) Pharmacokinetic disposition and protein binding of furosemide in newborn infants. J. Pediatrics 93:507-511. E Autret, J-P Dutertre, M Breteau, A-P Jonville, Y Furet, J Laugier Pharmacokinetics of Paracetamol in the neonate and infant after administration of propacetamol chlorhydrate. Dev Pharmacol Ther 20:129-134 (1993). Batra, V. K., Morrison, J. A., Lasseter, K. C. and Joy, V. A. Piperacillin kinetics. Clin Pharmacol Ther 26:41-53 (1979). Bertz, R.J. and Granneman, G.R. (1997) Use of in vitro and in vivo data to estimate the likelihood of metabolic pharmacokinetic interactions. Drug Interactions 32: 210-258. Besunder, J.B., Reed, M.D. and Blumer, J.L. (1988) Principles of drug biodisposition in the neonate: a critical evaluation of the pharmacokinetic-pharmacodynamic interface (Part I). Clin. Pharmaco. 14: 189-216. Bhat, R., Cart, G., Gulati, A. et al. “Pharmacokinetics of a single dose of Morphine in Preterm Infants During the first Week of Life.” J. Pediatr. 117: 477-481 (1990). 18 Blouin RA, Mann HJ, Griffen WO, Tobramycin pharmacokinetics in morbidy obese patients. Clin Pharmacol Ther 26:508-512 (1979). Bragonier, R., Brown, NM. "The Pharmacokinetics and toxicity of once-daily tobramycin therapy in children with cyctic fibrosis" J. of antimicrobial chemotherapy 1998, 42, 103-6. Chay, P. C. W., Duffy, B. J., and Walker, J. S. “Pharmacokinetic-Pharmacodynamic Relationship of Morphine in Neonates,” Clin. Pharmacol. Ther. 51: 334-342 (1992). Chester, E., Reed, R.C., and Schwartz, H.J. (1982). The comparative evaluation of a new sustained-release theophylline preparation, bronkodylar- SR, with a theophylline elixir, elixophylline, in volunteers. Current Therapeutic Research, 32: 476-491. Choonara, I., Lawrence, A., Michalkiewicz, A., et al. “Morphine Metabolism in Neonates and Infants.” Br. J. Clin. Pharmacol. 34: 434-437. Cook, D. R., and Davis, P. J. Pediatric Anesthesia Pharmacology, In: Lake, C. ed. Pediatric Carciac Anesthesia Sydney, Prentice-Hall (1988), p. 138, cited in Anderson et al., (1997). Cresteil, T. (1998) Onset of xenobiotic metabolism in children: toxicological implications. Food Add. Contam. 15, Suppl. pp. 45-51. Cutler, N. R., Narang, P. K., Lesko, L. J., Ninos, M., and Power, M. Vancomycin disposition: the importance of age. Clin. Pharmacol Ther. 36:803-810 (1984). Cutler, R. E., Forrey, A. W., Christopher, T. G., and Kimpel, B. M. (1974) Pharmacokinetics of furosemide in normal subjects and functionally anephric patients. Clinical Pharmacology and Therapeutics 15:588-596. 19 Davis, P.J , Killian, A., Stiller, R. L. et al. Pharmacokinetics of Alfentanil in Newborn Premature Infants and Older Children, Developmental Pharmacology and Therapeutics 13:21-27 (1989). Debruyne, D., Moulin, M. A., Tartiere, J., Bigot, M., C., Gerard, J. L., and Bricard Clinical Pharmacokinetics After Repeated Intrapleural Bupivacaine Administration. Clin. Pharmacokinet. 18:240-244 (1990). Dempsey D et al Nicotine metabolism and elimination kinetics in newborns. Clin Pharm Ther 67(5)458-465;2000 Dollery, C. (ed.) (1999) Therapeutic Drugs, 2nd Edition. Churchill Livingstone, Edinburgh. Ecoffey C et al. Bupivacaine in children : Pharmacokinetics following caudal anesthesia. Anesthesiology 63(4);447-448:1985 Engel, G., Hofmann, U., Heidemann, H., Cosme, J. and Eichelbaum, M. (1996) Antipyrene as a probe for human oxidative drug metabolism: identification of the cytochrome P450 enzymes catalyzing 4-hydroxyantipyrine, 3-hydroxymethylantipyrine, and norantipyrine formation. Clin. Pharm. Ther. 59: 613-623. Evans, W.E., Relling, M.V., Rodman, J.H. and Crom, W.R. (1989) Anticancer therapy as a pediatric pharmacodynamic paradigm. Dev Pharmacol Ther 13:85-95. Faustman, E.M., Silbernagel, S.M., Fenske, R.A., Burbacher, T.M. and Ponce, R.A. (2000) Mechanisms underlying children’s susceptibility to environmental toxicants. Environ. Health Perspect. 108 (Suppl. 1): 13-21. Fehring, S.I. and Ahokas, J.T. (1989) Effect of the glutathione-S-transferase inhibitor, tienilic acid, on biliary excretion of sulphobromopththalein. Chem.-Biol. Int. 69: 23-32. 20 Franko, TG, Powell, DA, Nahata, MC. "Pharmacokinetics of Theophylline in Infants with Bronchiolitis" Eur J of Clin Pharmacol. 1982, vol 23, pp. 123-127. Gaspari F, et al Elimination Kinetics of thiopentone in Mothers and their Newborn Infants, Eur J clin Pharm 1985 - 28:321-325. Gibbs, J.P., Murray, G., Risler, L., Chien, J.Y., Dev, R. and Slattery, J.T. (1997) Age-dependent tetrahydrothiophenium ion formation in young children and adults receiving high dose busulfan. Cancer Res. 57: 5509-5516. Ginsberg, G., Hattis, D., Sonawane, B., Russ, A., Banati, P., Kozlak, M., Smolenski, S., and Goble, R. (2001, submitted) “Evaluation of Child/Adult Pharmacokinetic Differences from a Database derived from the Therapeutic Drug Literature.” Goodman Gilman, A., Rall, T.W., Nies, A.S. and Taylor, P. (1990) The Pharmacological Basis of Therapeutics, 8th Edition. Pergamon Press, NY. Grahnen, A., Bahr, C. von, Lindstrom, B., and Rosen, A. (1979). Bioavailability and pharmacokinetic parameters. Journal of Pharmokinetics and Biopharmaceutics, vol. 7, p. 579-602. Greenblatt, D., Shader, R.I., franke, K., MacLaughlin, D.S., Harmatz, J.S., Allen, M.D., Werner, A., and Woo, E. (1979) Title. J. Pharmaceutical Science, vol 68, no.1, p 57-? Guitton, J., Buronfosse, T., Desage, M., Lepape, A., Brazier, J.-L. and Beaune, P. (1997) Possible involvement of multiple cytochrome P-450s in fentanyl and sufentanil metabolism as opposed to alfentanil. Biochem. Pharmacol. 53: 1613-1619. Gupta, A. and Waldhauser, L.K. (1997) Adverse drug reactions from birth to early childhood. New Frontiers in Pediatric Drug Therapy 44: 79-92. 21 Gustafsson, L.L., Grell, A.M., Garle, M., Rane, A., and Schildt, B. (1984). Kinetics of morphine in cerebrospinal fluid after epidural adminstration. Acta Anaesthesiol. Scand., vol. 28, p. 535-9. Hakkola, J., Tanaka, E., and Pelkonen, O. (1998) Developmental expression of cytochrome P450 enzymes in human liver. Pharm. & Toxicol. 82: 209-217. Hall, K., Otten, N., Irvine-Meek, J., Leroux, M., Budnick, D., Verma, M., and Seshia, S. S. "First-Dose and Steady-State Pharmacokinetics of Valproic Acid in Children with Seizures," Clin. Pharmacokinet. 8: 447-455 (1983). Hartley, R., Green, M., Quin, M., et al. “Pharmacokinetics of Morphine Infustion in Neonates,” Arch. Dis. Child. 69: 55-59 (1993). Hattis, D., Ginsberg, G, Sonawane, B., Smolenski, S., Russ, A., Kozlak, M, and Goble, R. (2001, submitted) “Differences in Pharmacokinetics Between Children and Adults—II. Children’s Variability in Drug Elimination Half-Lives and in Some Parameters Needed for Physiologically-Based Pharmacokinetic Modeling,” presented at the California-EPA Children’s Environmental Health Workshop, April 23, 2001, Monterey, California, submitted to Risk Analysis. Hendeles, L., and Weinberger, M. “Theophylline—A ‘state of the Art’ Review,” Pharmacotherapy 3: 2-44 (1983) Jacqz-Aigrain, E., and Burtin, P. “Clinical Pharmacokinetics of Sedatives in Neonates,” Clinical Pharmacokinetics 31: 423-443 (1996). Jarrett, R. V., Marinkovich, G. A., Gayle, E. L., and Bass, J. W. "Individualized Pharmacokinetic Profiles to Compute Vancomycin Dosage and Dosing Interval in Preterm Infants" The Pediatric Infectious Disease Journal Vol 12, no 2,pp. 156-157 (1993). 22 Jochemsen, R., Wesselman, J.G.J., Boxtel, C.J. van, hermans, J., and Breimer, D.D. Comparative pharmacokinetics of brotizolam and triazolam in healthy subjects. Br. J. Clin. Pharmac., Vol. 16, p.291S-297S (1983). Johnson, C. E., Beekman, R. H., Kostyshak, D. A., Nguyen, T., Oh, D., and Amidon, G. L., "Pharmacokinetics and Pharmacodynamics of Nifedipine in Children with Bronchopulmonary Dysplasia and Pulmonary Hypertension" Ped Res. 29:500-503 (1991). Johnson, K. L., Erickson, J. P., Holley, F. O., and Scott, J. C. “Fentanyl Pharmacokinetics in the Pediatric Population” Anesthesiology 61:A441 (1984). Karl HW, Milgrom, P., Domoto, P., Kharasch, ED, Coldwell, SE, Weinstein, P., Leroux B., Awamura, K, Mautz, D, "Pharmacokinetics of Oral Triazolam in Children,” J of clinical psychopharmacology vol 17, no 3 169-72, (1997) Kearns, G.L. and Reed, M.D. (1989) Clinical pharmacokinetics in infants and children: a reappraisal. Clin. Pharmaco. 17 (Suppl 1): 29-67. Kearns, G., van den Anker, JN, Reed M., Blumer JL. "Pharmacokinetics of metoclopramide in neonates" J Clin pharmacol 38:122-128 (1998). Killian, A., Davis, P. J., Stiller, R. L. et al. Influence of Gestational Age on the Pharmacokinetics of Alfentanil in Neonates. Developmental Pharmacology and Therapeutics 15:82-85 (1990). Kirkpatrick, CMJ , SB Duffull & EJ Bragg Pharmacokinetics of gentamicin in 957 patients with varying renal function dosed once daily. Br J Clin Pharmacol 47:637-6431999 Kleinbloesem, C. H., Brummelen, P.. van, Linde, J. A., van de, Voogd, P. J., and Breimer, D. D. (1984). Nifedipine: Kinetics and dynamics in healthy subjects. Clin Pharmacol. Ther., vol. 35, p. 742-749. Koehntop, D., Rodman, J., Brundage, D., Hegland, M., and Buckley, J. Pharmacokinetics of Fentanyl in Neonates Anesthesiology 61:A439 (1984). 23 Koehntop, D.E., Rodman, J. H., Brundage, D. M., Hegland, M.G., and Buckley, J. J. "Pharmacokinetics of Fentanyl in Neonates," Anesth. Analg. 65:227-232 (1986).Koopmans, R., Dingemanse, J., Danhof, M., Horsten, G.P.M., van Boxtel, C.J. (1988) "Pharmacokinetic-Pharmacodynamic modeling of midazolam effects on the Central Nervous System" Clin. Pharm. Ther., 44: 14-22 Krauer,B., G.H. Draffan, F.M. Williams, R.A. Clare, C.T. Dollery, D.F. Hawkins, Elimination kinetics of amobarbitol in mothers and their newborn infants. Clin Pharmacol Ther 14:442447, 1973 Kuhnz W ., Jager-Roman, E.J., Rating, D., Deichl, A., Kunze, J., Helge, H. and Nau, H. Carbamazepine and carbamazepine epoxide during pregnancy and postnatal period in epileptic mothers and their nursed infants. Ped Pharm 3:199-208 (1983) Lemmens, H.J.M., Dyck, J.B., Shafer, S.L., Stanski, D.R. (1994) PharmacokineticPharmacodynamc Modeling in Drug development: Application to the Investigational Opioid trefentanil, Clin. Pherm. Ther. 56 (3): 261-271. Levy, M. Koren, G., Klein, J., McLorie, G., and Balfe, J.W. (1991) Captoril pharmacokinetics, blood pressure response and plasma renin activity in normotensive children with renal scarring. Dev Pharmacol Ther 4:185-193. Linday, L. A., Greenblatt, D. J. Warren, M.P., Harmatz, J.S., DeCresce, R., Cicalese, C., and LeDuc, B.W. “Changes in antipyrine pharmacokinetics during adolescence, correlated with age, hormonal levels, and Tanner stage,” Dev Pharmacol Ther 4:194-202 (1991). Lloyd CW, Martin WJ, Taylor BD, and Hauser AR, "Pharmacokinetics and Pharmacodynamics of Cimetidine and Metabolites in Critically Ill Children" The J of Pediatrics. vol 107 no 2, pp 295-300 (1985). Lynn, A. M., and Slattery, J. T., “Morphine pharmacokinetics in Early Infancy,” Anesthesiology 66: 136-139 (1987). 24 Mather, L.E. "Clinical Pharmacokinetics of Fentanyl and its Newer Derivatives,” Clinical Pharmacokinetics 8:422-446 (1983). McClain, D. A., and Hug, C. C. "Intravenous Fentanyl Kinetics" Cllinical Pharmacology and Therapeutics 28:106-114 (1980). McCracken, GH Jr Clinical pharmacology of gentamicin in Infants 2 to 24 months of age. American Journal of Diseases of Child. 124:884-887 (1972). McDermott CA, Kowalczyk AL, Schnitzler ER, Mangurten HH, RodvoldKA, Metrick S. "Pharmacokinetics of Lorazepam in Critically Ill neonates with Seizures" The J of Pediatrics vol 120 no 3 pp. 479-83 (1993). McRorie, T. I., Lynn, A.M., Nespeca, M.K., Opheim, K.E., and Slattery, J.T. The maturation of morphine clearance and metabolism. AJDC 146: 972-976 (1992). Mazoit, JX, Denson, DD, Samii, K. "Pharmacokinetics of Bupivacaine following Caudal Anesthesia in Infants" Anesthesiology 68:387-391 (1988). Meistelman C, Saint-Maurice C., Lepaul M., Levron J. , Loose J., Mac Gee K. "A Comparison of Alfentanil Pharmacokinetics in Children and Adults" Anesthesiology 66:13-16 (1987). Mihaly, G.W., Moore, R.G., Thomas, J., Triggs, E.J., Thomas, D., and Shanks, C.A.”The pharmacokinetics and metabolism of the anilide local anaesthetics in neonates I:Lignocaine.” Europ J Clin Pharmacol 13:143-152 (1978). Miller, M., Opheim, K.E., and Raisys, V.A. (1984). Theophylline metabolism: Variation and genetics. Clin. Pharmacol. Ther., vol. 35, p. 170-182. Miller, C.A., Slusher, L.B., and Vesell, E.S. (1985). Polymorphism of theophylline metabolism in man. J.Clin. Invest., vol. 75, p. 1415-1425. 25 Morgan, D., McQuillan, D., and Thomas, J. (1978). Pharmacokinetics and Metabolism of the Anilide Local Anaesthetics in Neonates: II-Etidocaine Europ J Clin Pharmacol 13:365-371. Morselli, P.L. (1989) Clinical pharmacology of the perinatal period and early infancy. Clin. Pharmaco. 17 (Suppl 1): 13-28. Nash, R.M., Stein, L., Penno, M.B., Passananti, G.T., and Vesell, E.S. (1984). Sources of interindividual variations in acetaminophen and antipyrine metabolism”. Clin. Pharmacol. Therap., vol. 36, p. 477-430. Parsons, W.D. and Neims, A.H. (1978) Effect of smoking on caffeine clearance Clin Pharm Ther 24:40-45. Parsons, W.D., Aranda, J. V., and Neims, A. H. (1976). Elimination of transplacentally acquired caffeine in fullterm neonates. Pediatric Research 10:333- Pasanisi, F., Meredith, P.A., and Reid, J.L. (1985). Pharmacokinetics of nifediphine. Int. J. of Pharm. Res., vol. 5, p. 63-66. Peterson, R. G., Simmons, M. A., Rumack, B. H., Levine, R. L., and Brooks, J.G. (1980) Pharmacology of furosemide in the premature newborn and infant. J. Pediatrics 97:139-143. Pokela, M.-L., Olkkola, K.T., Seppala, T., and Koivisto, M. Age-related morphine kinetics in infants. Dev Pharmacol Ther 20:26-34 (1993). Pynnonen S, Carbamazepine and its 10,11-epoxide in children and adults with epilepsy. Eur J Clin Pharmacol 11:129-133 (1977). Reed, M. D. Rational Prescribing of Extended-Spectrum Penicillin ß-Lactamaze Inhibitor Combinations: Focus on Ticarcillin/Clavulanic Acid. Annals of Pharmacology 32(suppl):S17-21 (1998). 26 Renwick, A.G. (1998) Toxicokinetics in infants and children in relation to the ADI and TDI. Food Addit. & Contam. 15, Suppl. pp. 17-35. Renwick, A.G., Dorne, J.L. and Walton, K. (2000) An analysis of the need for an additional uncertainty factor for infants and children. Regulatory Tox. & Pharm. 31: 286-296. Rey, E., Gelauney, L. Pons, G., Richard, M. O., Saint-Morraine, C., and Olive, G. "Pharmacokinetics of midazolam in children: comparative study of intranasal and intravenous administration" Eur J Clin Pharmacol. 41:355-357 (1991). Rodvold, K. A., Gentry, C. A., Plank, G. S., Kraus, D. M., Nickel, E., and Gross, J. R. “Prediction of Gentamicin concentrations in neonates and infants using a bayesian pharmacokinetic model.” Dev Pharmacol Ther 20:211-213 (1993). Ross-Lee, L.M., Eadie, M.J., Hooper, W.D., Bochner, F. "Single-Dose Pharmacokinetics of Metoclopramide" Eur. J. Clin. Pharmacol.20, 465-471 (1981). Rowland, M., Thomson, P. D., Guichard, A., and Melmon, K. L. “Disposition kinetics of lidocaine in normal subjects.” Ann NY Acad Sci 179:383-398 (1971) Santeiro, ML, Christie, J, Stromquist, C., Torres, BA, Markowsky, SJ "Pharmacokinetics of Continuous Infusion Fentanyl in Newborns" J of Perinatology, 17:135-139 (1997). Saarenmaa, E., and Neuvonen, P. J. “Gestational age and birth weight effects on plasma clearance of fentanyl in newborn infants” J. Pediatrics 136:767-770 (2000). Shively, C.A. and Vesell, E.S. (1975). Temporal variations in acetaminophen and phenacetin half-life in man. Clin. Pharm. Ther., vol. 18, p. 413-424. 27 Siber, G. R., Smith, A. L., and Levin, M. J. "Predictability of Peak Serum Gentamicin Concentration with dosage Based on Surface Area," Pediat. Pharmacol. Therap. 94: 135-138 (1979). Singleton, M. A., Rosen, J. I., and fisher, D. M. “Pharmacokinetics of Fentanyl for Infants and Adults,” Anesthesiology 61:A440 (1984). Sorbo S et al. (1984) ‘The Pharmacokinetics of Thiopental in Pediatric Surgical Patients,’ Anesthesiology 61:666-670. Stanski, D.R., Greenblatt, D.J. and Lowenstein, E., (1978). Kinetics of Intravenous and Intramuscular morphine. Clin. Pharmacol. Ther., vol. 24, no.1, p. 52-59. Swain AF et al J of Dermatology (1983). Pharmacokinetic observations on dapsone in dermatitis herpetiformis. 108:91-98. Tanaka, E. (1998) In vivo age-related changes in hepatic drug-oxidizing capacity in humans. J. Clin. Pharm. Ther. 23: 247-255. Thummel, K.E., O’Shea, D., Paine, M.F., Shen, D.D., Kunze, K.L., Perkins, J,D. and Wilkinson, G.R. (1996). Oral first-pass elimination of Midazolam involves both gastrointestinal and hepatic CYP3A-mediated metabolism. Clin. Pharm. and Therapeutics, vol. 59, no. 5, p. 491502. Tomson, G., N.-O. Lunell, A. Sundwall, and A. Rane, “Placental passage of oxazepam and its metabolism in mother and newborn.” Clin Pharmacol Ther 25(1):74-81 (1979). Treluyer, J.M., Cheron, G., Sonnier, M., and Cresteil, T. (1996) Cytochrome P-450 expression in sudden infant death syndrome. Biochem. Pharmacol. 52: 497-504. USEPA (1997) Exposure Factors Handbook. EPA/600/P-95/002Fb. Vesselinovitch, S.D., Rao, K.V.N. and Mihailovich, N. (1979) Neoplastic response of mouse tissues during perinatal age periods and its significance in chemical carcinogenesis. Natl. Canc. Inst. Monogr. 51: 239-250. 28 Vogelstein, B., Kowarski, A. A., and Leitman, P.S. “The Pharmacokinetics of Amikacin in Children. J. Pediatrics 91: 333-339 (1977). Walker, J.M., Wise, R., Mitchard, M. "The Pharmacokinetics of Amikacin and Gentamicin in Volunteers: A Comparison of Individual Differences" Journal of Antimicrobial Chemotherapy 5, 95-99 (1979). Wiest, D. B., Ohning, B. L., and Garner, S. S. The Disposition of Alfentanil in Neonates with Respiratory Distress. Pharmacotherapy 11:308-311 (1991). Wilson, C. B., Koup, J. R., Opheim, K. E., Adelman, L. A., Levy, J., Stull, T. L. Clausen, C., and Smith A. L. Antimicrobial agents and chemotherapy 22:442 (1982). Wistanley P et al Chlorproguanil/dapsone for uncomplicated Plasmodium falciparum malaria in young children: pharmacokinetics and therapeutic range. Trans Royal Society Trop Med Hyg (1997) 91,322-327. Yaffe, S.J., and J.V. Aranda (eds.) Pediatric Pharmacology, 2nd edition. 1992. WB Saunders Company. 29