Rheumatology 5 – Case Presentation
advertisement

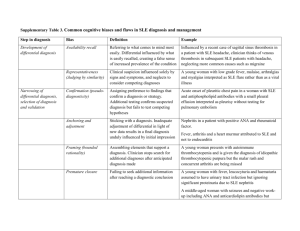
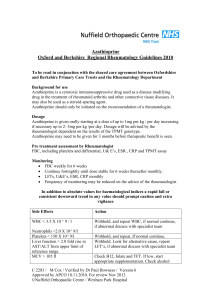
Rheumatology 5 – Case Presentation Anil Chopra History 41 year old man of African origin Presented in Africa in November 1997 at the age of 35 years Lethargy and hyperpigmentation of both cheeks. Alopecia Arthralgia and joint swelling of his wrists, small joints of the hands and ankles No significant past medical history and was a non-smoker March 1998: difficulty in breathing and a productive cough Pleural effusion. No pathogen was isolated and extensive cultures for tuberculosis were negative. Clinical suspicion for TB high: given trial of anti-tuberculous drugs for a total of ten weeks Unresponsive to this therapy Worsening shortness of breath precipitated another hospital admission Chest radiograph- basal pulmonary fibrosis Echocardiogram- pericardial effusion Sputum for AFB consistently negative HIV test negative ESR 5mm in 1st hour (low) o Normal ESR can be calculated as age/2 (M) or age+10/2 (F) Rheumatoid factor –ve; no LE cells. Diagnosis and Initial Treatment • A diagnosis of systemic lupus erythematosus (SLE) was made. • Treated with prednisolone, initiated at 60mg/day. • Shortness of breath and arthralgia resolved; chest X-ray findings persisted. • Discharged on prednisolone 15mg/day and later commenced on azathioprine 200mg/day with a reduction in prednisolone to 5mg/day. • Referred to rheumatology in the United Kingdom. History In UK • Summer 1999: – significant shortness of breath on exertion – arthralgia – Cushingoid Investigations FBC normal ESR 54mm in 1st hour C-reactive protein (CRP) 28mg/l Normal biochemical profile Normal complement levels C3 and C4 Polyclonal rise in gamma globulins Rheumatoid factor -ve Antinuclear antibody (ANA) 1:2560 Positive: o anti-Sm, nRNP, Ro and La Negative: o anti-dsDNA o antineutrophil cytoplasmic antibodies (ANCA) o anticardiolipin antibodies. Radiographs o demineralisation at the MCP joints and wrists o no erosive changes. A high resolution CT scan of the chest o small bilateral pleural effusions with basal fibrosis Diagnosis and Treatment • Results confirmed the diagnosis of SLE • Prednisolone dose increased to 10mg daily • Hydroxychloroquine 400mg daily added • Azathioprine 200mg daily continued • Calcichew D3 forte 1 tablet bd Progress » Seen in the UK on a yearly basis and in between was monitored in Africa » SLE remained under reasonable control » Developed type II diabetes mellitus, presumed to be steroid related » Summer 2003: pain in lower legs from mid-shaft of tibia to toes, maximal in his heels » Some difficulty walking » Osteoarthrits: • tenderness and warmth in hind feet • both feet showed mild generalised swelling. • peripheral pulses normal » T scores: • hip -0.5 • lumbar spine -1.6 – osteopenia. Diagnosis Calcaneal osteonecrosis: Characterised by death of the constituents of bone marrow Peripheral neuropathy: Death or damage to peripheral nerves resulting in loss of feeling in the legs. Algodystrophy This is a complex of symptoms and signs characterised by severe pain, swelling, autonomic vasomotor dysfunction and impaired mobility in affected joint areas. A radiographic picture of the affected joint area shows inconsistent demineralisation in a patchy or diffuse distribution. It may occur following trauma