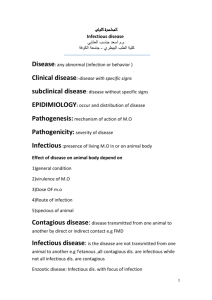
self activity
advertisement
The chair of pediatrics with children’s surgery, course of children infectious diseases Methodological instructions to self activities for the 5th course foreign students No 1 Theme: Urgent stages in case of influenza and acute viral upper respiratory tract infections: hyperthermia, seizures. Croup. Clinical features, diagnostic, therapy. Aim: to learn how to diagnose hyperthermia, seizures, croup syndrome in children with upper respiratory tract viral infection; find complications, perform differential diagnosis, prophylaxis and treatment. Professional motivation: hyperthermia, seizures, croup syndrome in children often are connected with upper respiratory tract viral infection. That’s why it requires from the doctor to know diagnostic criterions, duration, treatment and prevention of this pathology. Basic Level 1. Etiology, epidemiology of influenza, upper respiratory tract viral infections (infectious diseases). 2. Pathogenetical mechanisms of hyperthermia, seizures, croup syndrome development (pathological physiology). 3. Peculiarities of history asking in children (Propedeutic pediatrics). 4. Clinical examination of child by systems and organs. (Propedeutic pediatrics). 5. Interpretation of child’s laboratory and instrumental examination results. (Biochemistry, normal physiology, pathological physiology, roentgenology, Propedeutic pediatrics). 6. Pathogenetical and symptomatical treatment of hyperthermia, seizures, croup syndrome (pharmacology, infection diseases). Students’ Independent Study Program 1. Causes and clinical features of hyperthermia in children with upper respiratory tract viral infection. 2. Causes and clinical features of seizures in children with upper respiratory tract viral infection. 3. Pathogenetical mechanisms of croup syndrome in children with upper respiratory tract viral infection. 4. Prehospital and hospital treatment of hyperthermia, seizures, croup syndrome in children. Result Level Students must know Pathogenetical mechanisms of hyperthermia, seizures, croup syndrome in children with upper respiratory tract viral infection. Clinical features of hyperthermia, seizures, croup syndrome in children with upper respiratory tract viral infection. Prehospital and hospital treatment of children with this pathology. Students should be able to do: To diagnose hyperthermia, seizures, croup syndrome in children with upper respiratory tract viral infection. Interpret results of laboratory and instrumental examination of the child, Prescribe prehospital and hospital treatment to children with this pathology. A real life situation to be solved 1. A boy, 1 year old, is treated in the hospital from influenza, which complicated by seizures. 1. What investigation must be done? 2. Account a dose of Na oxybutiras to this boy. Answer: 1. Lumbar puncture with CSF analysis. 2. 50 mg/kg x 10 kg = 500 mg (2.5 ml of 20% solution). 2. A boy, 3 years old, has upper respiratory tract viral infection. At night body temperature increased to 39C; dry cough became barking, inspiratory dyspnea has appeared. Lung sound is “box”-like; during auscultation – rough breathing. Breathing rate is 36 per minute, cardiac rate – 126 per minute. 1. What is the reason of status worsening? 2. What treatment must be done on prehospital stage? Answer: 1. Development of croup syndrome. 2. Fever control and attempts to alleviate respiratory symptoms and patient anxiety (calming, and exposing the child to the cool night air). References: Main: 1. Current therapy in pediatric infectious diseases – 2 edited by John D. Nelson, M. D. – B.C. Decker inc. Toronto, Philadelphia, 1988, - P. 602-605, 611-615, 618-623, 753755. 2. Ambulatory pediatric care (edited by Robert A. Derchewitz; - 2 nd ed. – Lippincot – Raven, 1992. – P. 38-40, 44-45, 49-51. Additional: 1. Textbook of Pediatric Nursing. Dorothy R. Marlow; R. N., Ed. D. –London, 1989.-661p. 2. Pediatrics ( 2nd edition, editor – Paul H.Dworkin, M.D.) – 1992. – 550 pp. Prepared by I.L.Goryshna Adopted at the chair sitting 22.01.04 Minutes No 6 Revised at the chair sitting Minutes No 1 August 29, 2006. The chair of hospital and faculty pediatrics, course of children infectious diseases Methodological instructions to self activities for the 5th course foreign students No 2 Theme: Rubella. Etiolology, pathogenesis, differential diagnosis with measles, scarlet fewer, allergic exanthema. Inborn rubella. Treatment, prevention. Aim: To know diagnostic criterions of rubella in children, how to examine the child with rubella and prove the diagnosis, differentiate, give the individual treatment and prevention. Professional motivation: Rubella in children has predominantly mild duration. Last years cases of rubella in adults have increased. Especially it is dangerous in pregnant women, because infection of the fetus will lead to inborn defects. That’s why it requires from the doctor to know diagnostic criterions, duration, treatment and prevention of this pathology. Basic Level 1. Etiology, epidemiology of rubella (infectious diseases, epidemiology). 2. Pathomorphological changes in case of rubella (pathological anatomy). 3. Peculiarities of history asking in children (Propedeutic pediatrics). 4. Clinical examination of child by systems and organs. (Propedeutic pediatrics). 5. Interpretation of child’s laboratory and instrumental examination results. (Biochemistry, normal physiology, pathological physiology, Propedeutic pediatrics). 6. Pathogenetical and symptomatical treatment of viral diseases (pharmacology, infection diseases). Students’ Independent Study Program 1. Etiology, epidemiology, pathogenesis of rubella. 2. Main diagnostic criteria of acquired and inborn rubella. 3. Differential diagnostics of rubella. 4. main principles of acquired and inborn rubella treatment and prevention. Result Level Students must know Etiology, epidemiology, pathogenesis of rubella. Main diagnostic criteria of acquired and inborn rubella. Differential diagnosis of rubella. Methods of laboratory and instrumental examination in case of acquired and inborn rubella Complications of rubella. Main principles of rubella treatment and prevention. Students should be able to do: to diagnose acquired and inborn rubella, interpret results of laboratory and instrumental examination of the child in case of acquired and inborn rubella, perform differential diagnosis of rubella, prescribe treatment to children with this pathology and its prevention. A real life situation to be solved 7 years old girl complaints on: rashes on the skin, that appears today. During examination: maculopapular eruption, pallor-pink, on the normal skin, on the unbend surfaces, is separated from each other, body temperature is 37.3 С, enlargement of occipital lymph nodes. 1. Name previous diagnosis. 2. What diseases it must be differentiated from? Answers: 1. Rubella, typical mild form. 2. Measles, scarlet fever, infectious mononucleosis. 2. In one group of kindergarten a boy has rubella. His mother is pregnant (10 weeks) but is not vaccinated against this disease and was never ill. 1. What measures should be done in the kindergarten? 2. What measures should be done to the pregnant woman? Answers: 1. Boy mustn’t visit kindergarten up to 5th day from the beginning of the disease. Quarantine in the group on 21 days after isolation of this boy. 2. Serological investigation that must be repeated in 2 weeks. If titer of antibodies against rubella will increase – pregnancy must be interrupted. References: Main: 1. Current therapy in pediatric infectious diseases – 2 edited by John D. Nelson, M. D. – B.C. Decker inc. Toronto, Philadelphia, 1988. 2. Ambulatory pediatric care (edited by Robert A. Derchewitz; - 2 nd ed. – Lippincot – Raven, 1992.. Additional: 1. Cherry JD: Rubella virus. In: Feigin RD, Cherry JD, eds. Textbook of Pediatric Infectious Diseases. Vol 2. 4th ed . WB Saunders Co; 1998:1922-1949. 2. Maldonado YA: Rubella virus. In: Long SS, Pickering LK, Prober CG, eds. Principles and Practice of Pediatric Infectious Diseases. Churchill Livingstone; 1997:1228-1237. 3. Viral Infections of Humans. Epidemiology and Control. 4th edition. New York, NY: Plenum Medical Book Company, 1997. 4. Textbook of Pediatric Nursing. Dorothy R. Marlow; R. N., Ed. D. –London, 1989.-661p. 5. Pediatrics ( 2nd edition, editor – Paul H.Dworkin, M.D.) – 1992. – 550 pp. Prepared by I.L.Goryshna Adopted at the chair sitting 22.01.04 Minutes No 6 Revised at the chair sitting Minutes No 1 August 29, 2006. The chair of hospital and faculty pediatrics, course of children infectious diseases Methodological instructions to self activities for the 5th course foreign students No 3 Theme: Angina in children. Etiolology, making the diagnose, treatment. Treatment of angina at home. Aim: To know diagnostic criterions of angina in children, how to examine the child with angina and prove the diagnosis, differentiate, give the individual treatment and prevention. Professional motivation:Angina in children is one of the most often diseases. It may be caused by different agents (bacteria, viruses and fungi). That’s why it requires from the doctor to know diagnostic criterions, to perform the diagnose in time, give adequate treatment and prevent complications of this pathology. Basic Level 1. Etiology, epidemiology of anginas (infectious diseases, epidemiology). 2. Pathomorphological changes in case of different anginas (pathological anatomy). 3. Peculiarities of history asking in children (Propedeutic pediatrics). 4. Clinical examination of child by systems and organs. (Propedeutic pediatrics). 5. Interpretation of child’s laboratory and instrumental examination results. (Biochemistry, normal physiology, pathological physiology, Propedeutic pediatrics). 6. Etiological, pathogenetical and symptomatical treatment of anginas (pharmacology, infection diseases). Students’ Independent Study Program 1. Etiology, epidemiology of anginas. 2. Clinical features of different anginas (bacterial, viral and fungal). 3. Anginas’ complications. 4. Differential diagnosis of angina. 5. Main principles of anginas’ treatment and prevention/ Result Level Students must know Etiology, epidemiology of anginas. Diagnostic criterions of different anginas (bacterial, viral and fungal). Differential diagnosis of angina. Anginas’ complications. Methods of laboratory examination of the child, who has angina (bacteriological, virusological) Anginas’ treatment. Students should be able to do: to diagnose angina in examined child to prescribe laboratory examination of the child, to interpret results of the child’s laboratory examination, perform differential diagnosis of angina, to prescribe etiological, pathogenetical and symptomatical treatment to ill child. A real life situation to be solved 1. A girl, 6 years old complaints on sore throat, fever 39.2 C. She is ill for 2 days. During examination of the patient: pharyngeal and tonsillar erythema, purulent tonsillar exudate, enlargement of anterior cervical lymph nodes were found. 1. Name the diagnose. 2. Account a dose of penicillin G for this patient. Answers: 1. Lacunar noncomplicated angina, mild stage. 2. 100000 IU/kg x 22kg = 2,200,000 IU per day. 2,200,000:4=550,000 IU four times daily. 2. A boy, 3 years old is treated in infectious department from infectious mononucleosis, hard duration. He receive penicillin, aspirin, antihistamine drugs, multivitamins and local treatment with antiseptic fluids. 1. Which diseases it should be differentiated from? 2. What you can add to the treatment of this patient? Answers: 1. Diphtheria, adenovirus infection, acute leukemia, lymphogranulomathosis. 2. Corticosteroids (prednisone 1-2 mg/ kg/ day), a short course. References: Main: 1. Current therapy in pediatric infectious diseases – 2 edited by John D. Nelson, M. D. – B.C. Decker inc. Toronto, Philadelphia, 1988. -p.31-34, 47-49, 193-195. 2. Ambulatory pediatric care (edited by Robert A. Derchewitz; - 2 nd ed. – Lippincot – Raven, 1992.-p. 58-59; 254, 265, 315-319; 329-330. Additional: 1. Textbook of Pediatric Nursing. Dorothy R. Marlow; R. N., Ed. D. –London, 1989.-661p. 2. Pediatrics ( 2nd edition, editor – Paul H.Dworkin, M.D.) – 1992. – 550 pp. Prepared by I.L.Goryshna Adopted at the chair sitting 22.01.04 Minutes No 6 Revised at the chair sitting Minutes No 1 August 29, 2006. The chair of hospital and faculty pediatrics, course of children infectious diseases Methodological instructions to self activities for the 5th course foreign students No 4 Theme: Bowel yersiniosis. Peculiarities of epidemiology, pathogenesis, clinical features, making the diagnose. Treatment, prevention. Aim: To know diagnostic criterions of yersiniosis in children, how to examine the child with yersiniosis and prove the diagnosis, differentiate, give the individual treatment and prevention. Professional motivation: yersiniosis is an acute infectious disease which is characterized by polysyndromal clinical features; may have recedival, or hard duration. It occurs all over the world, previously in children and teenagers. Clinical polymorphism and widely spreading of the yersiniosis – are reason that doctors of all specialties must know how to diagnose this disease. Basic level 1. To know how to ask complaints, history of the disease, life history in children (propedeutic pediatrics). 2. To perform clinical examination of the child (propedeutic pediatrics). 3. To know microbiology, pathophysiology and pathomorphology of yersiniosis. 4. To diagnose yersiniosis after clinical and laboratory examinationof the child (infectious diseases, propedeutic pediatrics, microbiology, pathophysiology). 5. To give etiological, pathogenetical, symptomatical treatment (pharmacology). Students' Independent Study Program 1. Etiology, epidemiology, pathogenesis of yersiniosis. 2. Clinical diagnostic features of yersiniosis. 3. Laboratory examination of patient with yersiniosis. 4. Differential diagnosis of yersiniosis. 5. Main principles of treatment of yersiniosis. 6. Profilaxys of yersiniosis. Work in the epidemical focus. Result Level Students must know: Etiology, epidemiology, pathogenesis of yersiniosis. Clinical diagnostic features of yersiniosis. Laboratory examination of patient with yersiniosis. Differential diagnosis of yersiniosis. Main principles of treatment of yersiniosis. Profilaxys of yersiniosis. Students should be able to: Separate anamnestic data, which told us about yersiniosis. Find diagnostic clinical criterions of yersiniosis, during examination of the patient. To perform differential diagnosis among diseases, which have the similar clinical features. To learn the main tendentions of the yersiniosis treatment. To prevent yersiniosis. A real life situation to be solved 1. A girl 13 years old was hospitalized to infectious department with diagnose: yersiniosis, typical form. 1. What diseases it must be differentiated from? 2. What laboratory investigation confirm diagnose? Answers: 1. Pseudotuberculosis, acute bowel infections. 2. Bacteriological examinations of feces, urine, nasopharyngeal swab; serological investigations. 2. A girl 5 years old goes to kindergarten. Now she has yersiniosis, middle stage. 1. What preventive measures should be done in the kindergarten? 2. Prescribe etiotrope therapy. Answers: 1. Disinfection, contacts’ observation during 3 weeks (thermometry, examination of the skin, throat, feces), one bacteriological investigation of the feces. 2. Furazolidone: 10 mg x 20 kg = 200 mg/day : 4 = 50 mg per dose, 4 times per day. Rp: Tab. Furazolidoni 0.05 D.t.d. №20 S. 1 tablet 4 times per day References: Main: 1. Current therapy in pediatric infectious diseases – 2 edited by John D. Nelson, M. D. – B.C. Decker inc. Toronto, Philadelphia, 1988. 2. Ambulatory pediatric care (edited by Robert A. Derchewitz; - 2 nd ed. – Lippincot – Raven, 1992. Additional: 1. Cleary TG: Yersinia. In: Behrman RE, Kliegman RM, Jenson HB, eds. Nelson Textbook of Pediatrics. 16th ed. Philadelphia: WB Saunders; 2000: 857-859. 2. Pickering L, ed: Yersinia enterocolitica and Yersinia pseudotuberculosis infections. In: Red Book: Report of the Committee on Infectious Diseases. 25th ed. Elk Grove Village, Ill: American Academy of Pediatrics; 2000: 642-643. 3. Textbook of Pediatric Nursing. Dorothy R. Marlow; R. N., Ed. D. –London, 1989.661p. 4. Pediatrics ( 2nd edition, editor – Paul H.Dworkin, M.D.) – 1992. – 550 pp. Prepared by I.L.Goryshna Adopted at the chair sitting 22.01.04 Minutes No 6 Revised at the chair sitting Minutes No 1 August 29, 2006. The chair of hospital and faculty pediatrics, course of children infectious diseases Methodological instructions to self activities for the 5th course foreign students No 5 Theme: Urgent stages in case of meningococcal infection (toxic shock syndrome, brain edema), making the diagnose, treatment on prehospital and hospital stage. Aim: To know diagnostic criterions of meningococcal infection complications in children, how to examine the child with meningococcal infection complications and prove the diagnosis, differentiate, give the individual treatment and prevention. Professional motivation: duration of meningococcal infection’s generalized forms very often is complicated by brain’s edema, life threatened hemorrhages into inner organs (suprarenal glands), toxic shock syndrome, hemodynamic and metabolic disorders. These processes develop very quickly, may have lethal exit. That’s why, knowledge of their diagnostic criterions, treatment and prevention is very actual. Basic Level 1. Etiology, epidemiology of meningococcal infection (infectious diseases, epidemiology). 2. Pathogenetical mechanisms of brain’s edema, toxic shock syndrome development (pathological physiology). 3. Peculiarities of history asking in children (Propedeutic pediatrics). 4. Clinical examination of child by systems and organs. (Propedeutic pediatrics). 5. Interpretation of child’s laboratory and instrumental examination results. (Biochemistry, normal physiology, pathological physiology, Propedeutic pediatrics). 6. Etiological, pathogenetical and symptomatical treatment of brain’s edema, toxic shock syndrome (pharmacology, reanimathology). Students’ Independent Study Program 1. Causes and clinical features of brain’s edema in children with meningococcal infection. 2. Causes and clinical features of toxic shock syndrome in children with meningococcal infection. 3. Prehospital treatment of brain’s edema, toxic shock syndrome. 4. Hospital treatment of brain’s edema, toxic shock syndrome. Result Level Students must know Pathogenetical mechanisms of brain’s edema, toxic shock syndrome development in children with meningococcal infection. Clinical features of brain’s edema, toxic shock syndrome development in children with meningococcal infection. Prehospital and hospital treatment of children with this pathology. Students should be able to do: To diagnose brain’s edema, toxic shock syndrome in children with meningococcal infection. Interpret results of the laboratory and instrumental examination of the child, Prescribe prehospital and hospital treatment to children with this pathology. Real situations to be solved: 1. A boy of 1 year old was hospitalized in infectious department. The disease has begun 4 hours before. Objectively: hard condition, adynamia, cold extremities, body temperature is 39.5°C. Skin is pallor, with hemorrhagic ''star-like'' rashes of different size on buttocks, legs. Conjunctiva and pharynx are hyperemied. Heart beats are rhythmic, 176 per minute. Heart tones are dull. Arterial pressure on arms – 75/45 mm Hg. Breathing is puerile, 62 per minute. Abdomen is soft, painless. Meningeal symptoms are absent. 1. Name the diagnosis; 2. what etiothrope therapy should be prescribed? Account its dose. Answers: 1. Meningococcal infection, generalized form, meningococcemia, toxic shock syndrome 2nd stage. 2. Chloramphenicol (Laevomycetin) parenterally 80-100 mg/kg/day in 4 devided doses. 10 kg x 100 mg/kg = 1,000 mg per day, 250 mg per dose. 2. A girl, 2.5 years old was hospitalized in infectious department. The disease has begun yesterday: increased body temperature to 39°C, excitement, and tremor, repeated vomiting. Today seizures have appeared. 3 days ago was in a contact with brother, who now is treated from meningococcemia. Objectively: hard condition, adynamia, unconsciousness, seizures that periodically repeat. Meningeal symptoms are positive. Anisocoria, asymmetry of reflexes. Body temperature is 39.2°C. Skin is pallor. Heart beats are rhythmic, 100 per minute. Heart tones are dull. Breathing is superficial, 52 per minute. Abdomen is soft, painless. 1. Name the diagnosis; 2. Prescribe pathogenetical treatment to this child in the hospital. Answers: 1. Meningococcal infection, generalized form, meningitis. Brain’s edema. 2. manitol 1 g/kg IV droplet; in 2-5 hours lasix 1-2 mg/kg IV; dexazone 1 mg/kg, prednizone 5 mg/kg, hydrocortizone 20-30 mg/kg IV, albumin 10-20% – 10 ml/kg, concentrated plasma 10 ml/kg IV droplet, anticonvulsants (lytic suspension 0.1 ml/kg) References: Main: 1. Current therapy in pediatric infectious diseases – 2 edited by John D. Nelson, M. D. – B.C. Decker inc. Toronto, Philadelphia, 1988, - P. 134-138, 285. 2. Ambulatory pediatric care (edited by Robert A. Derchewitz; - 2 nd ed. – Lippincot – Raven, 1992. – P. 570-574; 255. Additional: 1. Textbook of Pediatric Nursing. Dorothy R. Marlow; R. N., Ed. D. –London, 1989.661p. 2. Pediatrics ( 2nd edition, editor – Paul H.Dworkin, M.D.) – 1992. – 550 pp. 3. Nadel S, Levin M, Habibi P: Treatment of meningococcal disease in childhood. In: Meningococcal Disease. John Wiley & Sons; 1995:207-43. 4. Tunkel AR, Scheld WM: Acute meningitis. In: Principles and Practice of Infectious Diseases. 4th ed. Churchill Livingstone; 1995:831-65. 5. Krugman, Saul, et al. Infectious Diseases of Children . St. Louis: Mosby Year Book, 1992. Prepared by I.L.Goryshna Adopted at the chair sitting 22.01.04 Minutes No 6 Revised at the chair sitting Minutes No 1 August 29, 2006. The chair of hospital and faculty pediatrics, course of children infectious diseases Methodological instructions to self activities for the 5th course foreign students No 6 Theme: Herpes virus infection (herpes simplex, herpes zoster). Etiology, epidemiology, pathogenesis, clinical features, making the diagnose, treatment, prevention. Aim: To know diagnostic criterions of Herpes virus infection in children, how to examine the child with Herpes virus infection and prove the diagnosis, differentiate, give the individual treatment and prevention. Professional motivation: Herpes virus infection – diseases that predominantly are characterized by skin and mucosal membranes damage. In newborns have severe, septic duration with high mortality. In elder children have recedival duration that tell us about immunodeficiency (often in case of AIDS, leukemia, malignant tumors). This has some prognostic meaning. That’s why, knowledge of their diagnostic criterions, treatment and prevention is very actual. Basic level 1. To know how to ask complaints, history of the disease, and life history in children (propedeutic pediatrics). 2. To perform clinical examination of the child (Propedeutic pediatrics). 3. To know microbiology, pathophysiology and pathomorphology of Herpes virus infection (microbiology, pathophysiology, pathomorphology). 4. To diagnose Herpes virus infection after clinical, laboratory examination of the child (infectious diseases, propedeutic, pediatrics, microbiology, and pathophysiology). 5. To give etiological, pathogenetical, symptomatical treatment (pharmacology). Students' Independent Study Program 1. Etiology, epidemiology, pathogenesis, pathomorphology of Herpes virus infection. 2. Classification of Herpes virus infection. 3. Main diagnostic criterions of Herpes simplex infection. 4. Main diagnostic criterions of Herpes zoster infection. 5. Complications of Herpes virus infection. 6. Differential diagnosis of Herpes virus infection. 7. Main principles of Herpes virus infection treatment and prevention. Result Level Students must know Etiology, epidemiology, pathogenesis, pathomorphology of Herpes virus infection. Classification of Herpes virus infection. Main diagnostic criterions of Herpes simplex infection. Main diagnostic criterions of Herpes zoster infection. Complications of Herpes virus infection. Differential diagnosis of Herpes virus infection. Main principles of Herpes virus infection treatment and prevention. Students should be able to do To diagnose Herpes virus infection. Interpret results of laboratory and instrumental examination of the child in case of Herpes virus infection. Perform differential diagnosis of Herpes virus infection. Prescribe treatment to children with this pathology and its prevention. A real life situation to be solved 1. A girl, 5 years old has herpes simplex infection, localized form (labial’s herpes), recedival duration. 1. What laboratory methods will prove this diagnose? 2. Prescribe treatment to this child. Answers: 1. Serologic examination, virusological examination of vesicles’ contents. 2. Unguent of acyclovir on damaged region 5-6 times per day. Adaptogens (Echinacea 5 drops 3 times per day during 1-2 months). Group B vitamins (B1, B2). 2. A boy, 10 years old complaints on pain, rashes on left lateral surface of the chest. 3 days ago had increased body temperature to 38.7 о С, pain in the same region. Rashes had appeared today. During examination: in left lateral surfase of the chest, along the 4th intercostal spase: hyperemia, infiltration of the skin with groupe of vesicles on it. General condition is satisfactory. 1. What disease must be suspected? 2. What evolution of rashes in this case? Answers: 1. Herpes zoster infection 2. Groupe along nerws’ branches: spot → papule → vesicle with transparent then cloud contents → crust → pigmentation. References: Main: 1. Ambulatory Pediatric care/edited by Robert Derchewitz;- 2nd ed.-LippingcotRaven,1992.- p.151-153. 2. Current therapy in pediatric infections disease-2/edited by John D. Nelson, M.D.- B. C. Decker inc. Toronto. Philadelphia,1988.-p.247-251. Additional: 1. Textbook of Pediatric Nursing. Dorothy R. Marlow; R. N., Ed. D. –London, 1989.-661p. 2. Pediatrics ( 2nd edition, editor – Paul H.Dworkin, M.D.) – 1992. – 550 pp. Prepared by I.L.Goryshna Adopted at the chair sitting 22.01.04 Minutes No 6 Revised at the chair sitting Minutes No 1 August 29, 2006. The chair of hospital and faculty pediatrics, course of children infectious diseases Methodological instructions to self activities for the 5th course foreign students No 7 Theme: Parapertussis. Etiology, epidemiology, pathogenesis, clinical features, making the diagnose, treatment, prevention. Aim: To know diagnostic criterions of Parapertussis in children, how to examine the child with Parapertussis and prove the diagnosis, differentiate, give the individual treatment and prevention. Professional motivation: Parapertussis clinically looks like pertussis or acute viral upper respiratory tract infection. Absence of active immune prophylaxis of parapertussis leads to epidemic flashes in kindergartens. That’s why, knowledge of Parapertussis diagnostic criterions, treatment and prevention is very actual. Basic Level: 1. To know how to ask complaints, disease history and life history in children (Propedeutic Pediatrics) 2. To perform clinical examination of the child (Propedeutic Pediatrics). 3. To know microbiology, pathophysiology, and pathomorphology of parapertussis (microbiology, pathophysiology, pathomorphology). 4. To diagnose parapertussis after clinical and laboratory examination of the child (infectious diseases, Propedeutic Pediatrics, microbiology, pathophysiology). 5. To give etiological, pathogenetical, and symptomatical treatment (pharmacology). Students' Independent Study Program 1. Etiology, epidemiology, pathogenesis, pathomorphology of parapertussis. 2. Classification of parapertussis. 3. Main diagnostic criterions of parapertussis. 4. Differential diagnosis of parapertussis. 5. Parapertussis treatment and prevention. Result Level Students must know Etiology, epidemiology, pathogenesis, pathomorphology of parapertussis. Classification of parapertussis. Main diagnostic criterions of parapertussis. Differential diagnosis of parapertussis. Parapertussis treatment and prevention. Students should be able to do To diagnose parapertussis. Interpret results of the laboratory and instrumental examination of the child in case of parapertussis. Perform differential diagnosis of parapertussis. Prescribe treatment to children with this pathology and its prevention. A real life situation to be solved 1. In the kindergarten 5 children became ill. All are coughing, cough is increasing. All children are vaccinated against pertussis. 1. What disease must be suspected? 2. Prescribe laboratory investigations. Answers: 1. Parapertussis 2. A culture of nasopharyngeal secretions for B. Parapertussis and B. Pertussis 2. A child, 3 years old complaints on cough, which progresses for last 10 days, is dry, and troubles him at nighttime. 2 days ago cough became spasmatic, near 10 times per day. Boy goes to kindergarten, is vaccinated against pertussis. 3 weeks ago exposured with a boy, who had the same cough. Other signs of disease are absent. 1. Name the diagnose. 2. What preventive measures should be done in the kindergarten? Answers: 1. Parapertussis, pertussis like form, mild stage, uncomplicated. 2. Disinfection, contacts’ observation during 2 weeks, cultural examination of nasopharyngeal secretions for B. Parapertussis and B. Pertussis. References: Main: 1. Ambulatory pediatric care/ edited by Robert A. Derchewitz; - 2nd ed. – Lippincot – Raven, 1992. – P. 742-747. 2. Current therapy in pediatric infections disease – 2/ edited by John D. Nelson, M.D. – B.C. Decker Inc. Toronto, Philadelphia, 1988. – P. 46-47. Additional: 1. Textbook of Pediatric Nursing. Dorothy R. Marlow; R. N., Ed. D. –London, 1989.661p. 2. Pediatrics ( 2nd edition, editor – Paul H.Dworkin, M.D.) – 1992. – 550 pp. Prepared by I.L.Goryshna Adopted at the chair sitting 22.01.04 Minutes No 6 Revised at the chair sitting Minutes No 1 August 29, 2006. The chair of hospital and faculty pediatrics, course of children infectious diseases Methodological instructions to self activities for the 5th course foreign students No 8 Theme: Poliomyelitis. Etiology, epidemiology, pathogenesis, clinical features, making the diagnose. Treatment, prevention. Differential diagnosis with ECНO and Coxsackie’s infection. Aim: To know diagnostic criterions of Poliomyelitis in children, how to examine the child with Poliomyelitis and prove the diagnosis, differentiate, give the individual treatment and prevention. Professional motivation: Poliomyelitis is a viral disease that predominantly develops in preschoolers (75–90%). Due to vaccination its frequency decreased more than 100 times. But in many countries last years sporadic paralytic forms of Poliomyelitis have been registered. In that cases mortality was 9–10%. That’s why, knowledge of Poliomyelitis diagnostic criterions, treatment and prevention is very actual. Basic Level: 1. To know how to ask complaints, disease history and life history in children (Propedeutic Pediatrics) 2. To perform clinical examination of the child (Propedeutic Pediatrics). 3. To know microbiology, pathophysiology, and pathomorphology of Poliomyelitis (microbiology, pathophysiology, pathomorphology). 4. To diagnose Poliomyelitis after clinical and laboratory examination of the child. (infectious diseases, Propedeutic Pediatrics, microbiology, pathophysiology). 5. To give etiological, pathogenetical, and symptomatical treatment (pharmacology). Students' Independent Study Program 1. Etiology, epidemiology, pathogenesis, pathomorphology of poliomyelitis. 2. Classification of poliomyelitis. 3. Main diagnostic criterions of poliomyelitis. 4. Differential diagnosis of poliomyelitis. 5. Poliomyelitis treatment and prevention. Result Level Students must know Etiology, epidemiology, pathogenesis, pathomorphology of poliomyelitis. Classification of poliomyelitis. Main diagnostic criterions of poliomyelitis. Differential diagnosis of poliomyelitis. Poliomyelitis treatment and prevention. Students should be able to do To diagnose poliomyelitis. Interpret results of the laboratory and instrumental examination of the child in case of poliomyelitis. Perform differential diagnosis of poliomyelitis. Prescribe treatment to children with this pathology and its prevention. A real life situation to be solved 1. A boy, 7 years old became ill 3 days ago: body temperature 39,6о С, repeated vomiting, headache, weakness. On the 3rd day he couldn’t close right eye, face asymmetry during speaking has appeared. The boy wasn’t vaccinated. 1. What disease is suspected? 2. What his family doctor must do? Answers: 1. Poliomyelitis, typical pontine form, paralytic period, severe stage. 2. Hospitalize the boy into infectious hospital, where he must be isolated for 40 days; inform sanitary-epidemiologic structures; look after contact persons. 2. A health boy, 3 months old was brought to ambulatory clinic to perform plane vaccination. 1. What vaccine against poliomyelitis he would receive, when next doses of primary vaccination must be given? 2. What specific complication may occur? Answers: 1. Oral poliomyelitis vaccine, in 4, 5 months. 2. Vaccinal poliomyelitis. References: Main: 1. Ambulatory pediatric care/ edited by Robert A. Derchewitz; - 2nd ed. – Lippincot – Raven, 1992. 2. Current therapy in pediatric infections disease – 2/ edited by John D. Nelson, M.D. – B.C. Decker Inc. Toronto, Philadelphia, 1988. Additional: 1. Textbook of Pediatric Nursing. Dorothy R. Marlow; R. N., Ed. D. –London, 1989.661p. 2. Pediatrics ( 2nd edition, editor – Paul H.Dworkin, M.D.) – 1992. – 550 pp. Prepared by I.L.Goryshna Adopted at the chair sitting 22.01.04 Minutes No 6 Revised at the chair sitting Minutes No 1 August 29, 2006. The chair of hospital and faculty pediatrics, course of children infectious diseases Methodological instructions to self activities for the 5th course foreign students No 9 Theme: Enterovirus infection. Etiology, epidemiology, pathogenesis, clinical features, making the diagnose, treatment, prevention Aim: To know diagnostic criterions of Enterovirus infection in children, how to examine the child with Enterovirus infection and prove the diagnosis, differentiate, give the individual treatment and prevention. Professional motivation: ECНO and Coxsackie’s viruses caused several acute infections, that have vide spectrum of clinical features: from mild temperature increase and asymptomatic carrying up to severe meningoencephalitis, myocarditis and other. That’s why, knowledge of Enterovirus infection diagnostic criterions, treatment and prevention is very actual. Basic Level: 1. To know how to ask complaints, disease history and life history in children (Propedeutic Pediatrics) 2. To perform clinical examination of the child (Propedeutic Pediatrics). 3. To know microbiology, pathophysiology, and pathomorphology of Enterovirus infection (microbiology, pathophysiology, pathomorphology). 4. To diagnose Enterovirus infection after clinical and laboratory examination of the child (infectious diseases, Propedeutic Pediatrics, microbiology, pathophysiology). 5. To give etiological, pathogenetical, and symptomatical treatment (pharmacology). Students' Independent Study Program 1. Etiology, epidemiology, pathogenesis, pathomorphology of Enterovirus infection. 2. Classification of Enterovirus infection. 3. Main diagnostic criterions of Enterovirus infection. 4. Differential diagnosis of Enterovirus infection. 5. Enterovirus infection treatment and prevention. Result Level Students must know Etiology, epidemiology, pathogenesis, pathomorphology of Enterovirus infection. Classification of Enterovirus infection. Main diagnostic criterions of Enterovirus infection. Differential diagnosis of Enterovirus infection. Enterovirus infection treatment and prevention. Students should be able to do To diagnose Enterovirus infection. Interpret results of the laboratory and instrumental examination of the child in case of Enterovirus infection. Perform differential diagnosis of Enterovirus infection. Prescribe treatment to children with this pathology and its prevention. A real life situation to be solved 1. A boy, 5 years old became ill 3 days ago: body temperature 38.6о С, vomiting, sore throat, headache. On the 3rd day maculopapulous rashes all over the body have appeared. Conjunctives are hyperemied, hyperemia of pharynx, tonsils; they are covered with small papules and vesicles that are fulled with transparent exudate. 1. Name previous diagnose. 2. What laboratory investigations could prove it? Answers: 1. Enterovirus infection, combined form: exanthema, herpangina, moderate duration. 2. Virusological investigation of nasopharyngeal mucus, paired serological investigation. 2. A girl, 12 years old complaints on: high body temperature (39.2о С), headache, severe spasmodic pain in the neck, chest, upper part of abdominal wall. Pain increases with deep breathing. Objectively: conjunctives are hyperemied, hyperemia of pharynx, tonsils. Heart tones are loud, heart rate – 100 per minute. Breathing – vesicular. Breathing rate – 20 per minute. Abdomen is soft, slight painful in upper parts. Peritoneal signs are absent. 1. Name previous diagnose. 2. What diseases it must be differentiated from? Answers: 1. Enterovirus infection, epidemic myalgia, moderate duration. 2. From influenza, pleuritis, pleuropneumonia, “acute abdomen”. References: Main: 1. Ambulatory pediatric care/ edited by Robert A. Derchewitz; - 2nd ed. – Lippincot – Raven, 1992. 2. Current therapy in pediatric infections disease – 2/ edited by John D. Nelson, M.D. – B.C. Decker Inc. Toronto, Philadelphia, 1988. Additional: 1. Textbook of Pediatric Nursing. Dorothy R. Marlow; R. N., Ed. D. –London, 1989.661p. 2. Pediatrics ( 2nd edition, editor – Paul H.Dworkin, M.D.) – 1992. – 550 pp. Prepared by I.L.Goryshna Adopted at the chair sitting 22.01.04 Minutes No 6 Revised at the chair sitting Minutes No 1 August 29, 2006. The chair of hospital and faculty pediatrics, course of children infectious diseases Methodological instructions to self activities for the 5th course foreign students No 10 Theme: Acute bowel infections, caused by relative pathogenic bacteria. Bacteriological and serological diagnostic. Aim: To know diagnostic criterions of acute bowel infections, caused by relative pathogenic bacteria in children, how to examine the child with acute bowel infections, caused by relative pathogenic bacteria and prove the diagnosis, differentiate, give the individual treatment and prevention. Professional motivation: last years, acute bowel infections, caused by relative pathogenic bacteria in children, appeared more often predominantly in maternal houses and children’s hospitals. That’s why, knowledge of diagnostic criterions of acute bowel infections, caused by relative pathogenic bacteria in children, their treatment and prevention are very actual. Basic Level: 1. To know how to ask the complaints, disease history and life history in children (Propedeutic Pediatrics) 2. To perform clinical examination of the child (Propedeutic Pediatrics). 3. To know microbiology, pathophysiology, and pathomorphology of acute bowel infections, caused by relative pathogenic bacteria (microbiology, pathophysiology, pathomorphology). 4. To diagnose acute bowel infections, caused by relative pathogenic bacteria after clinical and laboratory examination of the child (infectious diseases, Propedeutic Pediatrics, microbiology, pathophysiology). 5. To give etiological, pathogenetical, and symptomatical treatment (pharmacology). Students' Independent Study Program 1. Etiology, epidemiology, pathogenesis, pathomorphology of acute bowel infections, caused by relative pathogenic bacteria. 2. Classification of acute bowel infections, caused by relative pathogenic bacteria. 3. Main diagnostic criterions of acute bowel infections, caused by relative pathogenic bacteria. 4. Differential diagnosis of acute bowel infections, caused by relative pathogenic bacteria. 5. Treatment and prevention of acute bowel infections, caused by relative pathogenic bacteria. Result Level Students must know Etiology, epidemiology, pathogenesis, pathomorphology of acute bowel infections, caused by relative pathogenic bacteria. Classification of acute bowel infections, caused by relative pathogenic bacteria. Main diagnostic criterions of acute bowel infections, caused by relative pathogenic bacteria. Differential diagnosis of acute bowel infections, caused by relative pathogenic bacteria. Treatment and prevention of acute bowel infections, caused by relative pathogenic bacteria. Students should be able to do To diagnose acute bowel infections, caused by relative pathogenic bacteria. Interpret results of laboratory and instrumental examination of the child in case of acute bowel infections, caused by relative pathogenic bacteria. Perform differential diagnosis of acute bowel infections, caused by relative pathogenic bacteria. Prescribe treatment to children with this pathology and its prevention. A real life situation to be solved. 1. A child, 5.5 years old enters the infectious department from the kindergarten, where some cases of acute gastrointestinal infection were noticed. The disease has acute beginning: fever 38.5 ºC, vomiting, abdominal pain, liquid feces, and defecation 5 times per day. Objectively: skin pallor, tachycardia, tenderness of abdomen in the left inguinal region, spasms of the sigmoid colon. Feces are brown-green, with mucus. During feces bacteriological examination Proteus vulgaris was found. 1. Name main syndromes of disease. 2. what number of Proteus vulgaris give us possibility to diagnose proteosis? Answers: 1. Toxic, colitis. 2. more than 1х106 in 1 gram of feces. 2. A child, 2 years old is treated in the infectious department for 4 days because of klebsiellosis caused by Klebsiella pneumoniae, gastrointestinal form, moderate stage. 1. When patient can be discharged from department? 2. Name prevention in the epidemical focus. Answers: 1. When he becomes healhy, and after normalization of complete blood analysis. 2. Fecal culture from contacts, looking after contacts for 7 days, disinfection. References: Main: 1. Ambulatory pediatric care/ edited by Robert A. Derchewitz; - 2nd ed. – Lippincot – Raven, 1992. – p. 404-411 2. Current therapy in pediatric infections disease – 2/ edited by John D. Nelson, M.D. – B.C. Decker Inc. Toronto, Philadelphia, 1988. – p.80-81 Additional: 1. Textbook of Pediatric Nursing. Dorothy R. Marlow; R. N., Ed. D. –London, 1989.661p. 2. Pediatrics ( 2nd edition, editor – Paul H.Dworkin, M.D.) – 1992. – 550 pp. Prepared by I.L.Goryshna Adopted at the chair sitting 22.01.04 Minutes No 6 Revised at the chair sitting Minutes No 1 August 29, 2006. The chair of hospital and faculty pediatrics, course of children infectious diseases Methodological instructions to self activities for the 5th course foreign students No 11 Theme: Toxicosis and exicosis in case of acute bowel infections. Pathogenesis, clinical features, making the diagnose, treatment, oral rehydration. Aim: to learn how to diagnose toxicosis and exicosis syndrome in children, determine its type, period and phase, perform differential diagnosis, and treatment. Professional motivation: Toxicosis and exicosis are nonspecific generalized answer on infectious agent or its products in case of massive toxins’ income in blood with development of endotoxemia. Main pathologic processes in organism are connected with development of dehydration and loss of electrolytes. Progress of these processes leads to impairment of blood circulation, hypoxia of tissues, metabolic acidosis, toxic shock syndrome, and polyorganic insufficiency. That’s why it requires from the doctor to know diagnostic criterions, duration, treatment and prevention of this pathology. Basic Level 1. Etiology, epidemiology of acute bowel diseases (infectious diseases). 2. Pathomorphological changes in organs and systems, pathogenetical mechanisms in case of toxicosis with exicosis (pathological anatomy, pathological physiology). 3. To know how to ask the complaints, disease history and life history in children (Propedeutic Pediatrics) 4. To perform clinical examination of the child (Propedeutic Pediatrics). 5. To interpret results of laboratory and instrumental examination of the child. (Biochemistry, normal physiology, pathological physiology, roentgenology, Propedeutic pediatrics). 6. Pathogenetical and symptomatical treatment of toxicosis (pharmacology, infection diseases). Students’ Independent Study Program 1. Etiology, pathogenesis of toxicosis with exicosis. 2. Classification of toxicosis with exicosis. 3. Diagnostic criterions of different types of toxicosis with exicosis. with exicosis 4. Differential diagnosis of toxicosis with exicosis between neurotoxicose. 5. Prehospital and hospital treatment of toxicosis with exicosis, prognosis and prophylaxis. Result Level Students must know Etiology, pathogenesis of toxicosis with exicosis. Classification of toxicosis with exicosis. Diagnostic criterions of different types of toxicosis with exicosis. Differential diagnosis of toxicosis with exicosis between neurotoxicose. Prehospital and hospital treatment of toxicosis with exicosis, prognosis and prophylaxis. Students should be able to do: ask complaints, disease and epidemiologic history, examine the patient, interpret results of laboratory and instrumental examination of the child, perform differential diagnosis of toxicosis with exicosis, prescribe to child prehospital and hospital treatment of toxicosis with exicosis. A real life situation to be solved. 1. A boy 6 months old has repeated vomiting, appetite is absent; is ill for 2 days. Disease has developed after he had drunk unboiled milk. During examination: malaise, skin is pallor, mucus membranes of oral cavity are dry. Moderate thirst is present. Large fontanel is lower than skull bones. Weight loss is 4 %. Tachycardia – 130 per minute. Body temperature 38° C. Abdomen is soft, tender when colon is palpated. Feces are liquid, dark yellow without blood and mucus 12 times per day. Urination was 8 times per day. 1. Name previous diagnose. 2. What type of dehydration has developed? How to prove it? Answers: 1. Escherichiosis, moderate form, toxicosis with exicosis, 1st stage. 2. Isotonic. To measure electrolytes in the blood. 2. A boy, 8 months old, entered the infectious department. The disease had acute beginning. Now: doesn’t want to drink anything; repeated vomiting, body temperature is 35.5 ºC. Objectively: skin pallor, with “marble” paint, skin and mucus membranes are dry; large fontanel is lower than skull bones; cold extremities; tachycardia, tenderness of abdomen in the left inguinal region. Feces are in a large amount, looks like mud, with mucus. In entrance room he became unconscious, tonico-clonic seizures has appeared. Body weight is 8 kg. 1. What type of exicosis has developed? 2. Accoun daily amount of fluids to this child for the 1st stage of rehydration. How many saline and water fluids must be given? Answers: 1. Salt defficiensy (hypotonic). 2. 220 ml/kg x 8 kg = 1760 ml. 1 part (600 ml) of saline fluids, 2 parts (1200 ml) of water fluids. References: Main: 1. Ambulatory pediatric care/ edited by Robert A. Derchewitz; - 2nd ed. – Lippincot – Raven, 1992. – p. 404-411 2. Current therapy in pediatric infections disease – 2/ edited by John D. Nelson, M.D. – B.C. Decker Inc. Toronto, Philadelphia, 1988. – p.80-81 Additional: 1. Textbook of Pediatric Nursing. Dorothy R. Marlow; R. N., Ed. D. –London, 1989.-661p. 2. Pediatrics ( 2nd edition, editor – Paul H.Dworkin, M.D.) – 1992. – 550 pp. Prepared by I.L.Goryshna Adopted at the chair sitting 22.01.04 Minutes No 6 Revised at the chair sitting Minutes No 1 August 29, 2006. The chair of hospital and faculty pediatrics, course of children infectious diseases Methodological instructions to self activities for the 5th course foreign students No 12 Theme: Cholera in children. Pathogenesis and clinical peculiarities in children. Making the diagnose, treatment Aim: To know diagnostic criterions of cholera in children, how to examine the child with Cholera and prove the diagnosis, differentiate, give the individual treatment and prevention. Professional motivation: cholera is quarantine infection. 7 pandemias of this disease are known. The last one has begun since 1961. South-Eastern Asia is en endemic center of cholera. That’s why, knowledge of Cholera diagnostic criterions, treatment and prevention is very actual. Basic Level: 1. To know how to ask complaints, disease history and life history in children (Propedeutic Pediatrics) 2. To perform clinical examination of the child (Propedeutic Pediatrics). 3. To know microbiology, pathophysiology, and pathomorphology of Cholera (microbiology, pathophysiology, pathomorphology). 4. To diagnose Cholera after clinical and laboratory examination of the child (infectious diseases, Propedeutic Pediatrics, microbiology, pathophysiology). 5. To give etiological, pathogenetical, and symptomatical treatment (pharmacology). Students' Independent Study Program 1. Etiology, epidemiology, pathogenesis, pathomorphology of Cholera. 2. Classification of Cholera. 3. Main diagnostic criterions of Cholera. 4. Differential diagnosis of Cholera. 5. Cholera treatment and prevention. Result Level Students must know Etiology, epidemiology, pathogenesis, pathomorphology of Cholera. Classification of Cholera. Main diagnostic criterions of Cholera. Differential diagnosis of Cholera. Cholera treatment and prevention. Students should be able to do To diagnose Cholera. Interpret results of laboratory and instrumental examination of the child in case of Cholera. Perform differential diagnosis of Cholera. Prescribe treatment to children with this pathology and its prevention. A real life situation to be solved 1. A girl, 13 years old became ill 5 hours ago. Nausea, repeated vomiting, nonstop diarrhea without abdominal pane are present. Body temperature is 36º C. Has developed 3rd stage of dehydration. Feces and vomits looks like rice-water. 1. Name previous diagnose. 2. Prescribe etiotrope treatment to this girl. Answers: 1. Cholera. 2. Chloramphenicol (Laevomycetin) enterally 50 mg/kg/day in 4 devided doses. 40kg x 50 mg/kg = 2,000 mg per day; 500 mg per dose. 2. A girl, 10 years old is hospitalized in infectious department with previous diagnose cholera. 1. What diseases it must be differentiated from? 2. What contra epidemic measures in the focus of infection must be done? Answers: 1. Rotaviral infection; enterotoxigenic escherichiosis. 2. Isolation of the girl into “choleric hospital”, disinfection, contacts’ supervising, in case of appearing in them suspect symptoms – isolation into “provisor hospital”. References: Main: 1. Ambulatory pediatric care/ edited by Robert A. Derchewitz; - 2nd ed. – Lippincot – Raven, 1992. – p. 404-411 2. Current therapy in pediatric infections disease – 2/ edited by John D. Nelson, M.D. – B.C. Decker Inc. Toronto, Philadelphia, 1988. – p.80-81 Additional: 1. Textbook of Pediatric Nursing. Dorothy R. Marlow; R. N., Ed. D. –London, 1989.661p. 2. Pediatrics ( 2nd edition, editor – Paul H.Dworkin, M.D.) – 1992. – 550 pp. Prepared by I.L.Goryshna Adopted at the chair sitting 22.01.04 Minutes No 6 Revised at the chair sitting Minutes No 1 August 29, 2006. The chair of hospital and faculty pediatrics, course of children infectious diseases Methodological instructions to self activities for the 5th course foreign students No 13 Theme: Rota-viral infection. Etiology, epidemiology, pathogenesis, clinical features, making the diagnose, treatment, prevention Aim: To know diagnostic criterions of rotavirus infection in children, how to examine the child with Rotavirus infection and prove the diagnosis, differentiate, give the individual treatment and prevention. Professional motivation: rotavirus infection is the main cause of viral gastroenteritis in infants. This infection is widely spread all over the world. Secretory diarrhea leads to moderate or severe exicosis that needs to perform differentiation of rotavirus infection between cholera, enterotoxigenic escherichiosis, and other secretory diarrheas. That’s why, knowledge of Rotavirus infection diagnostic criterions, treatment and prevention is very actual. Basic Level: 1. To know how to ask complaints, disease history and life history in children (Propedeutic Pediatrics) 2. To perform clinical examination of the child (Propedeutic Pediatrics). 3. To know microbiology, pathophysiology, and pathomorphology of Rotavirus infection (microbiology, pathophysiology, pathomorphology). 4. To diagnose Rotavirus infection after clinical and laboratory examination of the child (infectious diseases, Propedeutic Pediatrics, microbiology, pathophysiology). 5. To give etiological, pathogenetical, and symptomatical treatment (pharmacology). Students' Independent Study Program 1. Etiology, epidemiology, pathogenesis, pathomorphology of Rotavirus infection. 2. Classification of Rotavirus infection. 3. Main diagnostic criterions of Rotavirus infection. 4. Differential diagnosis of Rotavirus infection. 5. Rotavirus infection treatment and prevention. Result Level Students must know Etiology, epidemiology, pathogenesis, pathomorphology of Rotavirus infection. Classification of Rotavirus infection. Main diagnostic criterions of Rotavirus infection. Differential diagnosis of Rotavirus infection. Rotavirus infection treatment and prevention. Students should be able to do To diagnose Rotavirus infection. Interpret results of laboratory and instrumental examination of the child in case of Rotavirus infection. Perform differential diagnosis of Rotavirus infection. Prescribe treatment to children with this pathology and its prevention. A real life situation to be solved A boy 3 years old is ill for 2 days. Main syndromes are: toxic with hyperthermia; dyspeptic with vomiting, diarrhea (like rice-water); catarrhal changes in upper respiratory tract; moderate exicosis. 1. What infection can cause this signs? 2. How to prove the diagnosis? Answers: 1. Rotaviral 2. Virusological investigation of feces, serological reactions. 2. A girl, 1.5 years old has rotaviral infection. 1. What diseases it must be differentiated from? 2. What type of diarrhea is typical for it? Answers: 1. Cholera; enterotoxigenic escherichiosis. 2. Secretory. References: Main: 1. Ambulatory pediatric care/ edited by Robert A. Derchewitz; - 2nd ed. – Lippincot – Raven, 1992. – p. 404-411 2. Current therapy in pediatric infections disease – 2/ edited by John D. Nelson, M.D. – B.C. Decker Inc. Toronto, Philadelphia, 1988. – p.80-81 Additional: 1. Textbook of Pediatric Nursing. Dorothy R. Marlow; R. N., Ed. D. –London, 1989.661p. 2. Pediatrics ( 2nd edition, editor – Paul H.Dworkin, M.D.) – 1992. – 550 pp. Prepared by I.L.Goryshna Adopted at the chair sitting 22.01.04 Minutes No 6 Revised at the chair sitting Minutes No 1 August 29, 2006. The chair of hospital and faculty pediatrics, course of children infectious diseases Methodological instructions to self activities for the 5th course foreign students No 14 Theme: Typhus abdominals, paratyphus А and В in children. Clinical, pathogenetical peculiarities in age aspect. Early diagnostic criterions Aim: To know diagnostic criterions of typhus abdominals, paratyphus А and В in children, how to examine the child with Rotavirus infection and prove the diagnosis, differentiate, give the individual treatment and prevention. Professional motivation: typhus abdominals, paratyphus A and B are spread all over the world. In 2-10 % of cases will form carrying of infection that even may be chronic. Discharge of bacteria will support epidemic process. That’s why, knowledge of Typhus abdominals, paratyphus A and B diagnostic criterions, treatment and prevention is very actual. Basic Level: 1. To know how to ask the complaints, disease history and life history in children (Propedeutic Pediatrics) 2. To perform clinical examination of the child (Propedeutic Pediatrics). 3. To know microbiology, pathophysiology, and pathomorphology of Typhus abdominals, parayphus A and B (microbiology, pathophysiology, pathomorphology). 4. To diagnose Typhus abdominals, parayphus A and B after clinical and laboratory examination of the child (infectious diseases, Propedeutic Pediatrics, microbiology, pathophysiology). 5. To give etiological, pathogenetical, and symptomatical treatment (pharmacology). Students' Independent Study Program 1. Etiology, epidemiology, pathogenesis, pathomorphology of Typhus abdominals, paratyphus A and B. 2. Classification of Typhus abdominals, paratyphus A and B. 3. Main diagnostic criterions of Typhus abdominals, paratyphus A and B. 4. Differential diagnosis of Typhus abdominals, paratyphus A and B. 5. Typhus abdominals, paratyphus A and B treatment and prevention. Result Level Students must know Etiology, epidemiology, pathogenesis, pathomorphology of Typhus abdominals, paratyphus A and B. Classification of Typhus abdominals, paratyphus A and B. Main diagnostic criterions of Typhus abdominals, paratyphus A and B. Differential diagnosis of Typhus abdominals, paratyphus A and B. Typhus abdominals, paratyphus A and B treatment and prevention. Students should be able to do To diagnose Typhus abdominals, paratyphus A and B. Interpret results of laboratory and instrumental examination of the child in case of Typhus abdominals, paratyphus A and B. Perform differential diagnosis of Typhus abdominals, paratyphus A and B. Prescribe treatment to children with this pathology and its prevention. A real life situation to be solved 1. A child, 10 years old enters the infectious department. He is ill for 1.5 week. The disease has gradual beginning: temperature subfebril, than 38.5-40.2 ºC, head ache, abdominal pain, cramps. Objectively: skin is pallor, near 20 roseols on chest and abdomen; tongue is covered with gray, enlarged; bradycardia, dull heart tones; rough breathing; tenderness of abdomen in the right inguinal region, liver and spleen are lower costal ribs. 1. What infection is suspected? 2. What laboratory investigations should be done? Answers: 1. Typhus abdominals. 2. Blood-, urine-, fecal-culture, Vidal reaction; complete blood and urine analyses. 2. A child, 8 years old, is treated in infectious department from: Typhus abdominals, typical, moderate form. 1. What diseases it must be differentiated from? 2. When patient could be discharged from hospital? Answers: 1. Paratyphus A and B; salmonellosis, typhoid form; enterovirus infection; pseudotuberculosis; yersiniosis; infectious mononucleosis. 2. Clinically health, not earlier 21st day of normal temperature, after 3 negative fecal and urinal cultures (on the 5th, 10th, 15th day of normal temperature), 1 negative bile culture (on 12th day of normal temperature). Antibiotic therapy could be abolished not earlier than 11th day of normal body temperature. References: Main: 1. Ambulatory pediatric care/ edited by Robert A. Derchewitz; - 2nd ed. – Lippincot – Raven, 1992. – p. 404-411 2. Current therapy in pediatric infections disease – 2/ edited by John D. Nelson, M.D. – B.C. Decker Inc. Toronto, Philadelphia, 1988. – p.80-81 Additional: 1. Textbook of Pediatric Nursing. Dorothy R. Marlow; R. N., Ed. D. –London, 1989.661p. 2. Pediatrics ( 2nd edition, editor – Paul H.Dworkin, M.D.) – 1992. – 550 pp. Prepared by I.L.Goryshna Adopted at the chair sitting 22.01.04 Minutes No 6 Revised at the chair sitting Minutes No 1 August 29, 2006. The chair of hospital and faculty pediatrics, course of children infectious diseases Methodological instructions to self activities for the 5th course foreign students No 15 Theme: Neurotoxicose syndrome in infection diseases in children. Pathogenesis, clinical features, making the diagnose, treatment. Aim: to learn how to diagnose neurotoxicose syndrome in children, determine its period and phase, perform differential diagnosis, and treatment. Professional motivation: Neurotoxicose is nonspecific generalized answer on infectious agent or its products in case of massive toxins’ income in blood with development of endotoxemia. Neirotoxicose may develop in severe duration of many infectious diseases. Clinically it looks like neuroinfections. That’s why it requires from the doctor to know diagnostic criterions, duration, treatment and prevention of this pathology. Basic Level 1. Anatomic-physiological peculiarities of child’s CNS (propedeutic pediatrics). 2. Pathomorphological changes in organs and systems in case of neurotoxicose (pathological anatomy). 3. Signs of CNS pathology (propedeutic pediatrics). 4. To interpret results of laboratory and instrumental examination of the child. (Biochemistry, normal physiology, pathological physiology, roentgenology, Propedeutic pediatrics). 5. Pathogenetical and symptomatical treatment of neurotoxicose (pharmacology, infection diseases). Students’ Independent Study Program 1. Etiology, pathogenesis of neurotoxicose. 2. Classification of neurotoxicose. 3. Diagnostic criterions of different phases of neurotoxicose. 4. Interpretation of the laboratory and instrumental examination results. 5. Differential diagnostics of neurotoxicose between neuroinfection, toxicosis with exicosis. 6. Prehospital and hospital treatment of different phases of neurotoxicose, prognosis and prophylaxis. Result Level Students must know Etiology, pathogenesis of neurotoxicose. Classification of neurotoxicose. Diagnostic criterions of different phases of neurotoxicose. Differential diagnostics of neurotoxicose between neuroinfectons. Prehospital and hospital treatment of different phases of neurotoxicose, prognosis and prophylaxis. Students should be able to do: ask complaints, disease and epidemiologic history, examine the patient, interpret results of laboratory and instrumental examination of the child, perform differential diagnosis of neurotoxicose, Prescribe prehospital and hospital treatment of neurotoxicose. A real life situation to be solved 1. A boy, 3 years old, has been treated in the hospital from influenza. Next day has increased body temperature to 39,7о С, and head ache. Vomiting has appeared. During examination: stiff neck, positive Kernig’s and Brudzinsky signs. 1. What syndrome has developed? 2. How to differentiate it from meningitis? Answers: 1. Neurotoxicose, meningeal syndrome. 2. To perform CSF investigation. 2. A boy, 5.5 years old, entered the infectious department. The disease had acute beginning: fever 40.5 ºC, repeated vomiting. Objectively: skin pallor, tachycardia, tenderness of abdomen in the left inguinal region, spasms of the sigmoid colon. Feces are in a small amount, predominantly mucus and blood. In entrance room he became unconscious, tonico-clonic seizures has appeared. 1. Name main syndromes of disease. 2. What infection is suspected? Answers: 1. Neurotoxic, distal colitis. 2. Shigellosis, acute form. References: Main: 1. Current therapy in pediatric infectious diseases – 2 edited by John D. Nelson, M. D. – B.C. Decker inc. Toronto, Philadelphia, 1988, - P. 134-138, 285, 602-605, 611-615, 618-623, 753-755. 2. Ambulatory pediatric care (edited by Robert A. Derchewitz; - 2 nd ed. – Lippincot – Raven, 1992. – P. 38-40, 44-45, 49-51, 570-574; 255. Additional: 3. Textbook of Pediatric Nursing. Dorothy R. Marlow; R. N., Ed. D. –London, 1989.-661p. 4. Pediatrics ( 2nd edition, editor – Paul H.Dworkin, M.D.) – 1992. – 550 pp. Prepared by I.L.Goryshna Adopted at the chair sitting 22.01.04 Minutes No 6 Revised at the chair sitting Minutes No 1 August 29, 2006. The chair of hospital and faculty pediatrics, course of children infectious diseases Methodological instructions to self activities for the 5th course foreign students No 16 Curation of the patient, writing the case history. I. Y. GORBACHEVSKY TERNOPIL STATE MEDICAL UNIVERSITY PEDIATRICS DEPARTMENT The head of the department Doctor of Medicine, Professor O.Ye. Fedortsiv Manager of the group ____________________ MEDICAL CARD name, surname of the patient _______________ age of the patient Clinical diagnosis: basic diagnosis __________________________________________ __________________________________________ __________________________________________ Complication __________________________________________ __________________________________________ Concomitant disease __________________________________________ __________________________________________ __________________________________________ Mark for the writing of the case history ______________ Mark for the defense of the case history ______________ Curator ____________________________ The group __________, the course ______ TERNOPIL 2007 GENERAL INFORMATION ABOUT PATIENT Name _________________________________________________________________ Surname _______________________________________________________________ Date of birth ____________________________, age ___________________________ Home address __________________________________________________________ Preschool or school institution _____________________________________________ Date of admission to the hospital ___________________________________________ Institution which has directed patient to the hospital ____________________________ Pre-admission diagnosis __________________________________________________ ______________________________________________________________________ Patient’s department _____________________________________________________ I. COMPLAINTS Main: ________________________________________________________________ ______________________________________________________________________ ______________________________________________________________________ ______________________________________________________________________ ______________________________________________________________________ Additional: ____________________________________________________________ _______________________________________________________________________ ____________________________ ______________________________________________________________________ II. ANAMNESIS OF THE DISEASE The onset of disease acute, subacute, gradually (the necessary underline). The duration of the diseases is ______________. What preceded the disease (cooling, defects of nutrition, viruses infection, the contact with ill person, etc) ___________________________________ _______________________________________________________________________ ____________________________ ______________________________________________________________________ The development of disease _______________________________________________ ______________________________________________________________________ ______________________________________________________________________ The result of previous additional methods of investigation (if they were presence) _______ ______________________________________________________________________ ______________________________________________________________________ The previous treatment (if it was presence): _____________________________________ _______________________________________________________________________ _____________________________________________________________________ The effect of previous treatment ____________________________________________ ______________________________________________________________________ The reason of hospitalization _______________________________________________ ______________________________________________________________________ III. ANAMNESIS VITAE For children till 3 years The child from ____ (behind the account) pregnancy, _____ delivery. Age of the mother during the given pregnancy. The pregnancy proceeded (with, without) gestosis in ___ trimester, on a background (without) of the extragenital pathology ___________ ________________________, or inflectional diseases ___________________________ ___________________________________ or somatic illness ____________________ ________________________________________________ in _______ trimester. The mother used such medicines (to specify the trimester) _______________________________ ______________________________________________________________________ Harmful habits at the mother: ______________________________________________, at the father ___________________________________________________________. Conditions of work of the mother during pregnancy ____________________________ Conditions of life of the mother during pregnancy ______________________________ Delivery at timed or premature (the necessary underline), in ___ weeks of gestation. Labor via vaginal way or by cesarean section, with (without) medicamental stimulation _______________________ (the necessary underline). The child was mature or immature, according Apgar’s score _____ points at first min. and ____ points at 5 th min. Birth weight was ______ g, length of the body was ___ сm, head circumference was ___ сm, chest circumference was ___ cm. The umbilical stump (residual cord) has fallen off in ___ days. After the stump has fallen off, the state of cord base was dry, or was weeping during __________ weeks. The child discharged from maternity department on ____ day (when it was more than 56 days, specify the cause of delay) __________________________________________. During the firs year the child was at ___________________ feeding. The reason of artificial feeding was ____________________________________________________. Mother used to such ______________________________________________________ formulas. The term of introduction of fruit juice __________, fruit puree ______, egg yolk __________, cottage cheese ___________, meat ____________. The first addition food was __________________ at _______ mo. The second addition food was _______ ____________ at _____ mo. The third addition food was _____________ at _____ mo. The dynamics of body weight ______________________________________________ ______________________________________________________________________. Dynamics of body length _________________________________________________ ______________________________________________________________________. Dynamics of head circumference __________________________________________. Dynamics of chest circumference ___________________________________________. The psychomotor development of the child ___________________________________ _______________________________________________________________________ _____________________________________________________________________. For all children irrespective of age The child had such diseases (before admission) ________________________________ ______________________________________________________________________ ______________________________________________________________________ Housing conditions of the child is satisfactory or not satisfactory (the necessary underline and explain why) __________________________________________________________. Character of nutrition before present disease (character of meal, schedule of feeding) __ _______________________________________________________________________ _____________________________________________________________________. Allergological history Presence of allergy symptoms _____________________________________________. The intolerance of products _____________________________________________, that accompanied with ___________________________________________________, The intolerance of medicament (drug) _______________________________________ that accompanied with ___________________________________________________. Prophylactic vaccinations _________________________________________________. ______________________________________________________________________ The nearest relatives have such chronic somatic illnesses ________________________ _______________________________________________________________________ _____________________________________________________________________, genetical illnesses ______________________________________________________, allergic reactions _______________________________________________________. Epidemiological history The child didn’t contact with patients who suffered with inflectional diseases last 3 weeks. The symptoms of diarrhea were _______________ during last three days. Summery: ______________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ ______________________________________________________________ Objective examination of the child The patient’s general condition is extremely grave, grave, moderately grave, satisfactory, good (the necessary underline). The state of consciousness is clear, sopor, stupor, coma (the necessary underline). The mental state is (not) adequate or not adequate (the necessary underline). Position of the child in bed is active, passive, forced (attitude) (the necessary underline). The patient is asthenic, hyposthenic, hypersthenic constitution (the necessary underline). The child is of regular, irregular body build (the necessary underline) _________________ ______________________________________________________________________ Anthropometrical measurements Criterion In patient Norm according empirical formulas Deviation, cm Deviation, % Weight, kg Height (stature), cm Head circumference, cm Chest circumference, cm The index of fatness by Chulitska The index by Erismann - Summery: _____________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ ___________________________________________________________________ The Skin and mucous membranes Colour of a skin ________________________________________________________ ______________________________________________________________________, lip-nose triangle ___________________________________, cyanoses _____________ ______________________________________________________________________. Rashes (colour, characteristic lesions, localization, size, presence of warmth, itching, type of distribution) _____________________________________________________________ ______________________________________________________________________ Surface of a skin is (smooth, velvety, rough, dry, moist)__________________________________. The elasticity of the skin is ________________________________________________. Temperature of a skin ___________________________________________________. The dermographism is ___________________________________________________ Sensitivity of the skin: temperature ___________, pain ______________, tactile _____. Nails: (shape, colour, thickness, quality) _____________________________________, ______________________________________________________________________. Hair: (color texture, quality, distribution, and elasticity) _________________________ ______________________________________________________________________ ______________________________________________________________________ Mucous membranes of a mouth (colour, moisture, presents of lesions) ______________ ______________________________________________________________________ Gums: (colour, presents of lesions, ability to bleeding) __________________________ ___________________________. Conjunctiva and sclera of eyes _________________ ______________________________________________________________________. The subcutaneous fat is distributed _________________________________________. The skinfold thickness is _____ cm on abdomen, _____ cm under the scapula, _____ cm on the shoulder, _____ cm on thigh. The oedema ___________________________ _____________________________________________________________________. The skin turgor is kept, decreased, flabby (the necessary underline). Lymphatic system Such groups of lymph nodes are palpable (describe each group according their localization, quantity, size, shape, mobility, consistency (elastic or dense), temperature, tenderness and visible change of enlarged nodes) ____________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _________________________________________________________________ The tonsils. The stage of enlargement of the tonsils ____________________________ they are reddened, loose, and tender on palpation (the necessary underline). Presence of haemorrhages _______ , pus in the crypts _________, erosions ___________________ ulcers __________________, the tonsils are covered with a ___________ (colour) film in size ____ cm. Muscular system The development of muscles is satisfactory, well-developed; symmetric, asymmetric (the necessary underline), presence of atrophy on _______________________________. Muscular tone is _______________, hypotonia of _____________________________, atony of ______________________________________________________________, hypertonia _____________________________________________________________, presence of muscular dystonia _____________________________________________. The range of motions is ___________________________________________________ ______________________________________________________________________ The strength of muscles __________________________________________________. Presence of pain during palpation of the muscles ______________________________. Presence of infiltrations or consolidation of ___________________________________ groups muscles. Trousseau’s sign is _____________, Chvostek’s symptom _________, Lust’s symptom _____________. Bone system Head circumference is _______ сm, (normal, microcephalia, macrocepalia (the necessary underline)). The head is dolichocephalic, brachycephalic, mesocephalic (the necessary underline). form (shape). There is hyperplasia of ________________________________ skull’s bones, occipital bones is _____ flat. Anterior fontanel (presence, size, shape, mould of the skull bones and attitude against the skull bony edges (does it taut or depressed) and pulsation) _________________________________________________ ______________________________________________________________________ Posterior fontanel (fused, size, shape) _______________________________________. Lateral fontanels ______________________. Sutures __________________________. The tooth formula: pd permanent – deciduous * - caries O - growth disorder Chest is conical, cylindrical, asthenic, normosthenic, hypersthnic, symmetrical, asymmetrical, barrel, funnel, keeled, phthinoid, rachitic breast (the necessary underline). Beading of the ribs _________. An epigastric angle ______ degrees. Chest circumference is _______ cm (normal, abnormal). Spine (physiological curvatures, scoliosis and kyphosis) _________________________ ______________________________________________________________________ ______________________________________________________________________ The extremities are ___ symmetrical, ____ deformed with deformation _____________ ______________________________________________________________________, anomalies of development ________________________________________________, ______________________________________________________________________ The feet are ____ normal with deformations __________________________________ ______________________________________________________________________ Others bone are ________________________________________________________ ______________________________________________________________________ The joints (shape, size, temperature, the range of motion, tenderness, swelling, the change of the skin over them) ______________________________________________ _______________________________________________________________________ _______________________________________________________________________ ____________________________________________________________________ ______________________________________________________________________ Gluteal folds are ___symmetrical, ___________________________________________ Angle of hip abduction is _____ degrees. Cardiovascular system Inspection: During inspection of the chest bulging ________ noted on left side, visible pulsation ______ seen, in _______ intercostals space ____________ line, epigastric pulsation _____ visible. Distended and pulsated neck veins ______ visible during inspection of the neck. Cyanosis ____________________________________________ ______________________________________________________________________, edema _______________________________________________________________, ______________________________________________________________________ Palpation: The apical or cardiac trust (beat) (the necessary underline). is located in ______ intercostals space ______________ line, area _____ сm2, is positive or negative (the necessary underline). Systolic or diastolic vibratory thrills (the necessary underline) _________ palpable at __________________. Pericardial friction rubs _________________________. Pulse (rate) is _________ beats per minute; is rhythmic, arrhythmic; is synchronic asynchronic; is full, swift, galloping, large, small, soft, tense, thready; pulse deficit (the necessary underline). Blood pressure of upper extremities _____ mm Hg, of lower extremities _____ mm Hg. Border’s of hearts relative dullness Border Right In patient Norma Upper Left transversal size Border’s of hearts absolute dullness Border Right Upper Left transversal size In patient Norma Auscultation: the heart sounds strong, weakened, muffled, rhythmical, arrhythmic (the necessary underline), ________ beats per min. S1 is heard loudest at the _______ of the heart, S2 is heard loudest at the _______ of the heart. Presence of accent ____________ _____________________________. Presence of organic, functional, systolic, diastolic, holosystolic, (the necessary underline) murmurs, place of the best auscultation __________ ______________________________________________________________________ ______________________________________________________________________ duration ________________________________, intensity ________________, timbre __________________, conductance _________________________________________ evaluation of its intensity in relationship to the child’s position ___________________ ______________________________________________________________________. Extracardiac murmurs ___________________ (pericardial friction rubs, pleurocardiac), localization ____________________________. During auscultations of carotic, subclavicular, femoral arteries, abdominal aorta, jugular veins are heard ______sounds, ___________________ murmurs. Respiratory system Cyanosis of nasolabial triangle, perioral region, nails plates, acrocyanosis __________ in rest or during physical exercises (the necessary underline). Nasal breathing is free, difficult, absent (the necessary underline). Voice is normal, hoarse, soundless, snuffling, silent, aphonic (the necessary underline). Cough __________ present, dry, moist, troublesome, brassy paroxismal cough, pertussis-like, barking cough, constant, cough of mucus, cough of pus, blood spitting (the necessary underline), frequent in _________ time of day. Dyspnea, asphyxia ____________________ occurs in rest, during physical exercises (the necessary underline). Chest has cylindrical, conical, asthenic, normosthenic, hypersthnic, symmetrical, asymmetrical ______________________________, barrel, funnel, keeled, phthinoid, rachitic breast. The intercostal spaces are _______________, Harrison’s groove ______________. Movements of etch parts of the chest are symmetrical, asymmetrical (the necessary underline) ______________________________________________________________________ Marked retraction of intercostal, suprasternal supraclavicular (the necessary underline) muscles ___________ noted. Type of breathing is thoracic, abdominal, combined (the necessary underline). Dyspnea is absent, inspiratory, expiratory, mixed (the necessary underline). The respiration rate is _____ per minute (normal, tachypnea, bradypnea). The breathing is regular, irregular, deep, hard (difficult), paradoxical, periodic, shallow, interrupted, whistling, stridulous, stenotic, Kussmaul’s breathing, Cheyne-Stokes respirations, Biot’s breathing (the necessary underline). Palpation: Pain is __________ in maxillary and frontal sinuses. Pain in chest ________ during palpations. Vocal fremitus is normal, decreased, increased, absent ___________ ______________________________________________________________________ Pleural friction rubs, crepitation ____________________________________________. In comparative percussing of the chest is heard ________________________________ ______________________________________________________________________ The lower costal margin of the lungs according to topographic percussing Line right left midclavicular midaxillary vertebral The excursion of the low margin of the lung (at midaxillary line) is ___ cm on left, ___ cm on right. The location of the apex of the lung _______________________________ ______________________________________________________________________ The width of Crenig’s areas _______________________________________________ Auscultation of the lungs: the breathing is ___________________________________ ______________________________________________________________________ presence of rales, rhonchi and crepitations ____________________________________ ______________________________________________________________________ Bronchophony is ______________________________________________________. Digestive system Inspection: The colour of mucous membranes of oral cavity is ____________, dry or moist (the necessary underline), incrustation (coating) _____________, fissure and aphtha _____________________________, colour of the tongue is _______________, coated with _______________ fur, state of papillas of tongue _______________________, dry, moist, atrophic, smooth, enlarged, normal size (the necessary underline). Colour of tonsils is ____________, coating ______________________, moisture _________ fissure and aphtha ______________. The odour from oral cavity __________________ In vertical position the abdomen has normal shape, distended, scaphoid, pendulous symmetrical or asymmetrical (the necessary underline) enlarged because of _________________________, abdominal circumference _____ cm, moves or doesn’t move with breathing, visible peristalsis ___________________, the umbilicus is centrally located, is flatten, inverted, everted, displased upwards (the necessary underline). In horizontal position the abdomen has ___________ shape, moves or doesn’t move with breathing, abdominal circumference _____ cm, the umbilicus is centrally located, is flatten, inverted, everted, displased upwards (the necessary underline). Distended veins of the anterior abdominal wall ______________, “caput Medusae” _________________. In superficial palpation there is soft, mild, moderate, demonstrable, board-like muscular tension of anterior abdominal wall (the necessary underline). Hyperesthesias ___________, the divergence of straight muscles _____ present, the tumour _______ present in region _____________________________. Blumberg’ sign is positive or negative; painless, extreme tendernees in McBurney’s point (the necessary underline). Deep palpation according to Obraztsov-Strazhesko Sigmoid colon is localized in ________________________, _______________ shape, ________ size (cm in diameter), _______________ consistence, ___________________ character of surface, _________ painfulness, _____ movable, _________ murmurs. Caecum is localized in ________________________, _______________ shape, ________ size (cm in diameter), _______________ consistence, ___________________ character of surface, _________ painfulness, _____ movable, _________ murmurs. Colon transversum is localized in ________________________, _______________ shape, ________ size (cm in diameter), _______________ consistence, ___________________ character of surface, _________ painfulness, _____ movable, _________ murmurs. Colon ascendens: is localized in ________________________, _______________ shape, ________ size (cm in diameter), _______________ consistence, ___________________ character of surface, _________ painfulness, _____ movable, _________ murmurs. Colon descendens is localized in ________________________, _______________ shape, ________ size (cm in diameter), _______________ consistence, ___________________ character of surface, _________ painfulness, _____ movable, _________ murmurs. Mendel’s symptom is positive or negative (the necessary underline). The liver ______ palpable, ______ tender, is extended ____ cm below the costal margin, shape of edge is sharp, rounded, smooth, elastic, firm (the necessary underline). Ortner’s symptom is _________, Ker’s symptom is _________, Murphy’s symptom is _________, Mussi-Georgievsky’s symptom is _________. The spleen ______ palpable, ______ tender, is extended ____ cm below the costal margin, shape of edge is sharp, rounded, smooth, elastic, firm (the necessary underline). Meyo-Robson’s symptom is _________. The pancreas _____ palpable, _________ consistency, ______ tender, smooth, elastic, firm (the necessary underline). In auscultation intestinal peristalsis is absent, sluggish, increased, not impaired, (the necessary underline). Stool is _____ time per day, formed, liquid, semi-liquid, regular, irregular (the necessary underline), _________ colour, with or without an admixing _______________________. Urinary system Inspection: _________ oedema on legs ___________, face, sacral part, on the lower part of abdomen. The colour of lumbar region is ________. The odour of urine is _____ Examination of sacral area, lower abdominal part (changing of the color of the skin ___________________, protrude ______________________, edema______________, asymmetry_______________________). Examination of the external sex organs: stage of development ____________________. Presence of excretion from urinal channel _____________________. In boys: asymmetric, symmetric development of the scrotum (the necessary underline). Testes _________ present in the scrotum; presence of inflammation of penis, _________ anomalies of penis development, phimosis, paraphimosis (the necessary underline). In girls: colour of mucous membranes of external sex organs is __________________, presence an excretions from vagina _________________________________________. Kidneys ______ palpable in vertical or horizontal position, _______________shape, _________________ consistency, _______ movable, ______ tender, smooth, firm (the necessary underline). Pasternatsky’s symptom is _____ on right , ________ on left side. Urinary frequency _____ per day, Daily urine flow _________ ml, proportion between day and night diuresis ____________. Presence of uncontrolled urinations _________. Endocrine system Examination: face expression __________________, presence of the eyes symptoms ____________________________________________________________________, changes of anterior cervical surface __________________. The level of development subcutaneous fat is ____________________________________________________. Thyroid gland _____ palpable, of _______ stage, ___________surface, ___________ consistence, ____________ pain. Sex development (according formulas F, L, Ax, P, V for boys and for girls - Ma, Ax, P, Me) __________________________________________________________________ Nervous system The consciousness is kept, stupor, sopor, is absent (the necessary underline). The mental development ______ corresponds to the age of child. Reaction on environmental is does not adequate (the necessary underline). Dream is isn’t quiet (the necessary underline). Expression of the face is ___________________. There are some minor abnormalities ______________________________________________________________________ ______________________________________________________________________. Nystagmus is ___________ horizontal, vertical. Pupils are (un)equal in size; presence of mydriasis, miosis (the necessary underline). The light reflex is retained (absent). The coordination of movement _______ kept. The pain sensitivity is kept, (is absent, hyperesthesia, hypoesthesia) (the necessary underline). Tactile sensitivity is kept (is absent, pathologic) (the necessary underline). Thermoesthesia is kept (is absent, pathologic) (the necessary underline). Vibration sensation is kept (is absent, pathologic) (the necessary underline). Newborn reflexes (the necessary underline): Sucking - is normal, hypoactive, hyperactive; Rooting - is normal, hypoactive, hyperactive; Defence - is normal, hypoactive, hyperactive; Lip or trunk reflex - is normal, hypoactive, hyperactive; Grasp - is normal, hypoactive, hyperactive; Babinski's - is normal, hypoactive, hyperactive; Moro - is normal, hypoactive, hyperactive; Supporting - is normal, hypoactive, hyperactive; Dance or step - is normal, hypoactive, hyperactive; Perez - is normal, hypoactive, hyperactive; Crawling - is normal, hypoactive, hyperactive; Bauer's - is normal, hypoactive, hyperactive; Galant - is normal, hypoactive, hyperactive. Upper Brudzinski’s reflex - is normal, hypoactive, hyperactive; middle Brudzinski’s reflex - is normal, hypoactive, hyperactive; low Brudzinski’s reflex - is normal, hypoactive, hyperactive. Tendon reflexes brisk, (equally marked on both sides, more hyperactive on the ______ than on ______ side, equally diminished, increased) (the necessary underline). Karniga’s sing positive, negative (the necessary underline). The paralyses (palsy) ______________________________________________________________________ The hyperkinesias _____________________________________________________ The dermographism is red, white, stria with ____ см in wide, appears in ____ second, disappears in ____ second, arises over surface of a skin (the necessary underline). Substantiation of the provisional diagnosis On the establishment of the patient’s complaints _______________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ ______ Anamnesis morbi ________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ ______ Epidemiological history _____________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ ____ Anamnesis vitae __________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ ___ Data of objective examinations ______________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _________________ It possible to make provisional diagnosis : ____________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ Results of additional methods of examination Rooting blood analysis date Нb Eryth. CI Leuc eos bas juv. band seg. lym mon E S R х1012 х109 Bloo d clotti Blee ng ding time time _______________________________________________________________________ ____ The plan of examination of the patient 1) ___________________________________________________________________ 2) ___________________________________________________________________ 3) ___________________________________________________________________ 4) ___________________________________________________________________ 5) ___________________________________________________________________ 6) ___________________________________________________________________ 7) ___________________________________________________________________ 8) ___________________________________________________________________ 9) ___________________________________________________________________ 10) __________________________________________________________________ 11) __________________________________________________________________ 12) __________________________________________________________________ Urinal examination according to Nechepurenco _______________________________ Biochemical analysis of blood date protein total glucose total bilirubin creatinine conjugated urea ALT AST Amylase Mucous Cristals: Casts Erythrocy tes Leucoc ytes Epitheliu m ketonuria Protein uria Glucos uria pH Amoun t Spesific gravity date The general examination of urine Urinal examination according to Zymnitzky Portion Quantities of urine specific gravity 1 2 3 4 5 6 7 8 Stool test ______________________________________________________________ ______________________________________________________________________ ______________________________________________________________________ Analysis of feces on worm ova _____________________________________________ ______________________________________________________________________ Test on enterobiosis ______________________________________________________ ______________________________________________________________________ Bacteriological examination ________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _____ _______________________________________________________________________ _______________________________________________________________________ __ ECG: _________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _ USD __________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _____ Endoscopies examination of ______________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ __ X-ray examination ______________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ ___ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ ____ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _____ Differential the diagnosis _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ ________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ ________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ ________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ ________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ ________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _____ Clinical diagnosis On the establishment of the patient’s complaints _______________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ ______ Anamnesis morbi ________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______ Epidemiological history ____________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ ____ Anamnesis vitae ________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ __ ______________________________________________________________________ Data of objective examinations _____________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ ________________ _______________________________________________________________________ _ Data of additional methods of examination ___________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _____________ _______________________________________________________________________ _ _______________________________________________________________________ _______________________________________________________________________ __ It possible to make clinical diagnosis: basic diagnosis __________________________________________ __________________________________________ __________________________________________ Complication __________________________________________ __________________________________________ __________________________________________ Concomitant disease __________________________________________ __________________________________________ __________________________________________ The temperature list data B P T ME ME ME ME ME ME ME ME ME ME ME ME ME ME P Stool Weight diuresis Treatment of the patient Regimen ____________________________________________________________ ______________________________________________________________________ Diet № ___ _______________________________________________________ _______________________________________________________________________ _____________________________________________________________________ The menu for infant: _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ ________________________________________________________________ Medicamental treatment: _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ ________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ ___ _______________________________________________________________________ _ Prevention (primary and secondary) _________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ __________ Epicrisis The patient ____________________________________________________________ _______ age, __________ date of birth, home address __________________________ _______________________________________________________________________ _______________________________________________________________________ _ received treatment in _____________________________________________________ _______________________ from ________ 200_ on _______ 200_ with the diagnosis of: ______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _____ The general state and data of objective examination of the patient on admission (shortly) _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ х1012 Bloo d clotti Blee ng ding time time _______________________________________________________________________ ____ Rooting blood analysis date Нb Eryth. CI Leuc eos bas juv. band seg. lym mon E S R х109 Mucous Cristals: Casts Erythrocy tes Leucoc ytes Epitheliu m ketonuria Protein uria Glucos uria pH Amoun t Spesific gravity date The general examination of urine Urinal examination according to Nechepurenco _______________________________ Biochemical analysis of blood date protein total glucose total bilirubin creatinine conjugated Urinal examination according to Zymnitzky Portion 1 2 3 4 urea 5 ALT 6 AST 7 Amylase 8 Quantities of urine specific gravity Stool test ______________________________________________________________ ______________________________________________________________________ ______________________________________________________________________ Analysis of feces on worm ova _____________________________________________ ______________________________________________________________________ Test on enterobiosis ______________________________________________________ ______________________________________________________________________ Bacteriological examination _________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ ____ ECG: _________________________________________________________________ _______________________________________________________________________ _____________________________________________________________________ USD __________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ ____ Endoscopies examination of ________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ ___ X-ray examination ________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ ___ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ ___Prescribed treatment ______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _____ Dynamic of the main syndromes during treatment; the objective state of the patient at the moment of his discharge from the hospital _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ ______ Recommendations: 1. Diet № ______________________________________________________________ 2. Regimen _____________________________________________________________ 3. Medical measures _____________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ ___ _______________________________________________________________________ _ Literature _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ _______________________________________________________________________ ___________________________________________________ The curator (signature) __________________ Prepared by: assistant of professor Nataliya I. Balatska The methodological instruction was discussed and confirmed at the session of the department Minutes No 1 August 29, 2006.