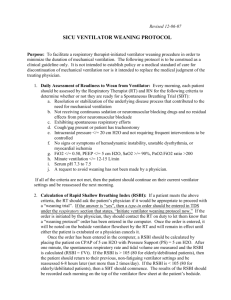
Appendix K: Definitions and Techniques for Spontaneous
advertisement

Appendix K: Definition and Techniques for Spontaneous Awakening (SAT) and Spontaneous Breathing Trial (SBT) Protocol Introduction - Reducing the number of days a patient is on mechanical ventilation has been shown to reduce the risk of VAP. 1-4 Strategies for weaning patients off of mechanical ventilation are often not handled well as the spontaneous awakening (SAT) and spontaneous breathing trials (SBT) are viewed separately. A wake up and breathe protocol using both the SAT and SBT can significantly reduce the number of days patients are on mechanical ventilation. Girard et. al.5 showed that paired, the SAT and SBT reduced the number of days patients were on mechanical ventilation (3.1 mean difference, 95% CI 0.7-5.6; p=0.02), with a concomitant reduction in the length of hospital stay (4 day difference) when compared to SBT alone. This same technique, often called a readiness-to-wean or sedation protocol, has been used in other institutions with much success. 4, 6, 7 We are using the model Girard et. al. developed in 2008 for this project. The SAT consists of two parts, a safety screen and the trial. (Please see flow diagram below.) The safety screen attempts to assure the trials will not be used when contraindicated. Patients pass the screen unless: 1. 2. 3. 4. 5. They are receiving a sedative infusion for active seizures or alcohol withdrawal They are receiving escalating doses of sedative for agitation They are receiving neuromuscular blockers They have evidence of active myocardial ischemia in prior 24 hours They have evidence of increased intracranial pressure If the patient passes the safety screen, all sedatives and analgesics used for sedation are stopped. Analgesics used for pain are continued. The goal is that the patient can open their eyes to verbal stimuli or can go without sedation for 4 hours or more without the following: 1. 2. 3. 4. 5. 6. 7. sustained anxiety agitation pain a respiratory rate of 35 breaths/minute for >= 5 minutes an SpO2 of less than 88% for >=5 minutes an acute cardiac dysrhythmia two or more signs of respiratory distress a. tachycardia b. bradycardia c. use of accessory muscles d. abdominal paradox e. diaphoresis f. marked dyspnea If a patient fails the SAT, sedatives are started at one half the prior dosage and titrated up as needed. If a patient passes the SAT, the patient is assessed for the SBT safety screen. Patients pass if: 1. 2. 3. 4. 5. they have adequate oxygenation (SpO2 >=88% on an F1O2 of <=50% and a PEEP <=8 cm H2O) any spontaneous inspiratory effort in a 5-min period no agitation no significant use of vasopressors or inotropes no evidence of increased intracranial pressure 1 If a patient fails, he is reassessed for SAT the following day. If the patient passes, they undergo the SBT. Ventilatory support is removed. Patient is allowed to breathe through either a T-tube circuit of a ventilatory circuit with CPAP of 5cm H2O or pressure support ventilation of less than 7cm H2O. Patients pass the trial if they don’t develop any of the following failure criteria for 120 minutes. 1. 2. 3. 4. 5. respiratory rate of more than 35 or less that 8 breaths per min for 5 min or longer hypoxemia (SpO2 < 88% for >=5 min) abrupt change in mental status an acute cardiac arrhythmia two or more signs of respiratory distress a. tachycardia b. bradycardia c. use of accessory muscles d. abdominal paradox e. diaphoresis f. marked dyspnea If a patient fails the SBT, he is reassessed for SAT the following day. If a patient passes, the patient’s physicians are notified for possible extubation. 2 3 Bibliography 1. Ely EW, Baker AM, Dunagan DP, et al. Effect on the duration of mechanical ventilation of identifying patients capable of breathing spontaneously. N Engl J Med. 1996;335(25):1864-1869. 2. Brook AD, Ahrens TS, Schaiff R, et al. Effect of a nursing-implemented sedation protocol on the duration of mechanical ventilation. Crit Care Med. 1999;27(12):2609-2615. 3. Kress J, Pohlman A, O'Connor M, Hall J. Daily interruption of sedative infusion in critically ill undergoing mechanical ventilation. N.Engl.J.Med. 2000;342:14711477. 4. Girard TD, Kress JP, Fuchs BD, et al. Efficacy and safety of a paired sedation and ventilator weaning protocol for mechanically ventilated patients in intensive care (awakening and breathing controlled trial): A randomised controlled trial. Lancet. 2008;371(9607):126-134. 5. Blackwood B, Alderdice F, Burns K, Cardwell C, Lavery G, O'Hallaran P. Use of weaning protocols for reducing duration of mechancal ventilatoin in critically ill adult patients: Cochran systematic review and meta-analysis. BMJ. 2011;Jan 13. 6. Quenot J, Ladoire S, Devoucoux F, et al. Effect of a nurse-implemented sedation protocl on the incidence of ventilator associate penumonia. Crit Care Med. 2007;35(9):2031-9.