HCB Objectives 18
advertisement
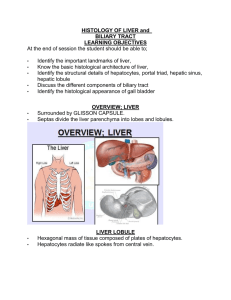
HCB Objectives 18 1. Liver functions: Bile synthesis/secretion, protein synthesis, glucose homeostasis, drug/toxin metabolism Endocrine gland specializations: enzyme synthesis (glucagon, insulin, somatostatin, etc.) Exocrine gland specializations: bile synthesis Blood regulation specializations: plasma protein synthesis 2. Anatomical relationships: a. Incoming vessels: hepatic artery (20%) and hepatic portal vein (80%) b. Outgoing vessels: central vein to sublobular hepatic vein c. Bile ducts: takes bile from bile canaliculi (between adjacent hepatocytes) and empties them through short bile ductules (simple cuboidal) into the bile duct. d. Sinusoids: takes incoming blood flow from portal tract (hepatic artery and hepatic portal vein) through the liver parenchyma to the central vein e. Liver cells: 1. Hepatocytes: bile canaliculi flow between adjacent hepatocytes 2. Sinusoidal endothelial cells: highly fenestrated cells composing the sinusoid endothelium 3. Stellate cells: fat storing cells which surround the external lumen to absorb lipid droplets and fat soluble vitamins 4. Kupffer cells: macrophages which live in the lumen of sinusoids and extend their processes through fenestrae Note: A portal tract is made up of a hepatic artery, portal vein, bile duct, and lymphatic vessel. Hepatic arteries and portal veins flow in the opposite direction of bile ducts and lymphatic vessels 3. Classic liver lobe: hexagonal structure with central vein in the center and portal tracts at the six vertices Pericentral microenvironment: smaller sinusoidal fenestrae, less endothelial surface area, better oxygenated, glucose uptake/release, urea formation, glutamine formation Periportal microenvironment: larger sinusoidal fenestrae, more endothelial surface area, poorly oxygenated, glycolytic enzymes, glutaminogenic enzymes Clinical significance of hepatic microenvironments: injuries prefer zones of the classic lobule; centrilobular environment is injured by carbon tetrachloride and acetaminophen, periportal environment is injured by allyl alcohol 4. Classic lobule: hexagonal structure with central vein in the center and portal tracts at the six vertices Portal lobule: hexagonal structure with portal tract in the center and alternating portal tracts and central veins as the vertices Hepatic acinus: amorphous distinction to describe areas of oxygenation/metabolic function; described by the closest area to the hepatic venules as 1 (most oxygenated) radiating out to the center being 3 (least oxygenated) 5. Hepatocyte: polyhedral epithelial cells composing the parenchyma of the liver. Relationships of apical, basal, lateral surfaces: a. Apical surface: face adjacent hepatocytes and enclose bile canaliculi b. Basal surface: face space of Disse/endothelial cells, microvilli extend through fenestrae to increase blood-parenchymal exchange c. Lateral surface: cell-cell junctions (gap junctions for exchange and tight junctions to seal blood supply from bile canaliculi Molecules being secreted/absorbed at surfaces: a. Bile: Absorbed through basal surface through cholesterol and bilirubin; secreted through apical surface into bile canaliculi b. Major plasma proteins: Secreted through basal surface into bloodstream c. Glucose, glycogen, drugs, toxins: Absorbed and secreted through basal surface into/out of bloodstream 6. Sinusoid cells: a. Sinusoidal endothelial cells: highly fenestrated cells composing the sinusoid endothelium b. Stellate cells: fat storing cells which surround the external lumen to absorb lipid droplets and fat soluble vitamins; synthesize collagen and are important in fibrotic scarring of cirrhosis c. Kupffer cells: macrophages which live in the lumen of sinusoids and extend their processes through fenestrae Note: the Space of Disse is the space between the basal membranes of hepatocytes and endothelial cells; it is important for the exchange of materials between hepatocytes and blood