Objectives 47 - U
advertisement

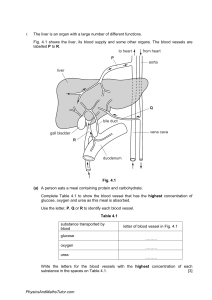
Pathology Lecture 47 Normal and Abnormal Liver 1) Recognize the dual vascular supply and massive reserve potential of the liver. Approximately 25% of total cardiac output arrives via the portal vein (60-70% of hepatic blood flow) and the hepatic artery (30-40%). The vast expanse of hepatic parenchyma is serviced via approximately 450,000 terminal branches of the portal tract system, blood traverses the sinusoids and exits into the terminal hepatic vein. This enormous functional reserve masks the clinical impact of early liver damage. 2) Recognize individual functions of hepatocytes, endothelial cells and Kupffer cells in the liver. Hepatocytes make up 60-80% of the cytoplasmic mass of the liver. These cells are involved in protein synthesis, protein storage and transformation of carbohydrates, synthesis of cholesterol, bile salts and phospholipids, and detoxification, modification and excretion of exogenous and endogenous substances. They also initiate the formation and secretion of bile. Endothelial cells are thin, flat cells that line the interior surface of blood vessels, forming an interface between circulating blood in the lumen and the vessel wall. Kupffer cells are specialized macrophages located in the liver attached to the luminal face of endothelial cells that form part of the mononuclear phagocyte system. Like other macrophages they are important in fighting infection. 3) Understand the normal biliary drainage and its insidious mode of initial biliary passages. Bile canaliculi, channels (1-2 µm in diameter), are located between abutting hepatocytes. Microvilli and microfilaments (actin and myosin) surround the canaliculus and help propel biliary fluid. Channels drain into the canals of Hering in the periportal region, which contain the first epithelial lining. Biliary fluid is then conveyed to bile ductules, which empties into the terminal bile ducts within the portal tracts. 4) Recognize the distinction between central necrosis and infarct. Centrilobular necrosis can be secondary to right heart failure (ischemic hepatitis) or due to hepatic vein thrombosis (acute). It occurs around the terminal hepatic vein and is characteristic of ischemic injury and a number of drug and toxic reactions. In ischemic coagulative necrosis, the liver cells are poorly stained and "mummified" and often have lysed nuclei. Infarcts are rare due to the dual blood supply. Nonetheless, thrombosis compression of an intrahepatic branch of the hepatic artery by embolism, neoplasia, polyarteritis nodosa trauma or sepsis may result in a localized infarct that is usually anemic and pale-tan or sometimes hemorrhagic. An infarct of Zahn (a misnomer), resulting from a portal vein branch occlusion, appears as a reddish-blue discoloration of sharply marked area. Microscopically no necrosis is seen, only hepatocyte atrophy and sinusoidal congestion is present. 5) Recognize the differences between Budd-Chiari Syndrome, venoocclusive disease and abnormalities of portal vein circulation. Budd-Chiari syndrome is obstruction of two or more major hepatic veins due to thrombi or polycythemia (anabolic steroids and oral contraceptives are contributing factors) producing liver enlargement, pain, and ascites due to increased intrahepatic blood-pressure and an inability of the massive hepatic blood flow to shunt around the blocked outflow tract. Sudden, often fatal, acute disease requiring surgery. Venoocclusive disease (sinusoidal obstruction syndrome) occurs primarily in the immediate weeks following bone marrow transplantation, but may also occur secondary to hepatotoxic alkaloids such as Jamaican bush tea, radiation therapy and chemotherapy. It is characterized by obliteration of hepatic vein radicals by varying amounts of subendothelial swelling and fine reticulated collagen. In acute disease, there is striking centrolobular congestion with hepatocellular necrosis and accumulation of hemosiderin-laden macrophages. Portal vein obstruction may be insidious and well tolerated or may be catastrophic and potentially lethal. Occlusion results in abdominal pain and ascites, and other manifestations of portal hypertension, mainly esophageal varices which are prone to rupture. Extrahepatic obstruction may arise from cancer in abdominal organs, peritoneal sepsis, and acute pancreatitis (initiates thrombosis and splenic vein). Intrahepatic obstruction may arise from primary and secondary tumors in the liver, sarcoidosis and tuberculosis of the liver.