FACTS ABOUT DENVER HEALTH: AN EFFICIENT, HIGH QUALITY
advertisement

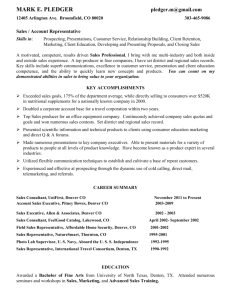
FACTS ABOUT DENVER HEALTH Denver Health separated from the city of Denver in 1997 and became Denver Health and Hospital Authority, a political subdivision of the state. Denver Health is Colorado and Region VIII’s largest safety net system, an essential health care provider and a major corporate contributor to the state’s well-being. Denver Health’s nine organizational components include: Ten community health centers (CHCs); 13 school-based clinics; A 349-bed hospital; Five dental health clinics; Managed care arrangements; Substance abuse and mental health treatment; A Public health department; Emergency (911) service; and A poison center and nurse advice line. Operating as a highly efficient major Colorado business, Denver Health employs 4,000 people and has an annual budget of more than $400 million. Payroll is $203 million. Recent construction projects totaling $109 million have created more than 1,000 construction jobs. Denver Health has many accomplishments. No health disparities exist based on ethnicity, despite Colorado being 49th in the nation in Medicaid funding and Denver Health having charges that are below average in most of the services measured by the Colorado Hospital Association. In 2003, the trauma center provided care for nearly 2,100 patients from 44 counties and eight states. The overall survival rate (96%) is one of the highest in the nation. In 2003, Denver Health served 160,000 patients, managed 400,000 outpatient visits, treated 14,000 inpatients, and took care of 35 percent of Denver’s children. Denver Health provided $240 million in services to the uninsured, with the City of Denver allocating $27 million to help cover costs, the State of Colorado allocating $1 million, and the federal government providing $39 million for the medically indigent. DSH payments have historically represented 14% of Denver Health’s budget. While only 19% of hospital patients are privately insured, 63% of Denver Health’s total services are for the uninsured and Medicaid patients. Denver Health has two governing boards. First, the hospital and other components are governed by a nine-member board appointed by the mayor and confirmed by the city council. Second, a separate mayor-appointed 13-member board governs the Neighborhood Health Program, which includes Denver Health’s ten CHCs and 13 school-based clinics.1 Fifty-one percent of this board is composed of Denver Health patients, fulfilling federal grant requirements. One member of the Denver Health board serves on this board. Denver Health is co-applicant with the Neighborhood Health Program on their federal CHC grant. While having two governing boards is complex, this co-applicant status has permitted integration of Denver Health’s CHCs and the other components of the system. Denver Health is a fully integrated system. First, functional integration occurs though common patient identifiers, medical records, and billing and information systems. A common pharmaceutical formulary is used for the CHCs and the hospital. Capital equipment for the entire Denver Health organization is prioritized by the senior executives during the budget process on the basis of need and strategic priorities. All full-time physicians at Denver Health 1 Even though it evolved as a separate primary care system, the Neighborhood Health Program is integrated with Denver Health. Facts about Denver Health Page 2 of 2 are salaried employees, have hospital admitting privileges, and are faculty of the University of Colorado School of Medicine. Second, horizontal integration is achieved through one administrative team and shared processes and care protocols across all CHC sites. Third, vertical integration is achieved since the system links the nine organizational components. The implications of integration have significant advantages. First, several patient and community benefits are achieved. Primary care is available within Denver’s medically underserved neighborhoods. In 1998, there were 164,800 (59%) primary care visits at the CHCs and school-based clinics and 113,700 (41%) primary care visits on the hospital campus. There were 18,100 dental visits in the CHCs and 17,800 dental visits on the hospital campus. Patients benefit by easy access to specialty care, with all adult and pediatric medical and surgical subspecialty services available at the hospital campus. In 1998, almost 50,000 specialty visits occurred. About 62% of patients seen in specialty clinics had another primary care CHC visit. Of the 2,700 newborns discharged in 1998, about 98% were scheduled for a CHC follow-up visit. A sophisticated information system technology has been deployed by linking billing, medical records, and patient scheduling across the system. A single-imaged medical record permits access to the medical record at any time at any location. Uninsured patients benefit by greater access to CHCs, with more than six of ten individuals served at Denver Health’s CHC sites were self pay in 1998. Denver Health CHCs receive Medicaid DSH revenues, which is reflected in the 45% Medicaid revenue compared to 35% nationally. Second, other benefits include patient access to a greater range of services and the development of Medicaid and commercial HMOs. The affiliation with the University of Colorado School of Medicine has provided access to certain subspecialties, research support, faculty status, and training programs. This affiliation allows residents the opportunity to gain experience in both safety net systems offered by the community health centers and the hospitals. In 1995, a Medicaid HMO, Colorado Access, was created by Colorado’s safety net providers, including Denver Health. As Colorado Access serves more than 50% of Medicaid HMO enrollees, Denver Health has the largest component, with 52% of enrollees. In 1985, Denver Health developed it own commercial HMO for Denver Health and Denver City and County employees, expanding to offer the Child Health Insurance Plan in 1998. Third, hospital benefits include a decline in the use of the emergency department for nonemergency conditions, discharge to appropriate follow up care and a corresponding minimizing of the average length of stay to 4.5 days, and having CHCs to feed patients into the hospital beds. Fourth, vertical integration benefits CHCs in several ways. The two most significant benefits are the availability of a diversification of funding streams and access to capital. From 2000 to 2002, Denver Health’s CHCs received more than $700,000 for capital equipment. In 1998, Denver Health issued revenue bonds, of which almost 30% went to expanding CHC capacity. Although Denver Health believes that benefits of integration outweigh the disadvantages, several challenges exist, such as administrative complexity, balance between autonomy of an individual CHC and uniformity of system process, and areas of competing focus from the needs of the tertiary trauma system to the needs of primary care and public health. However, the greatest challenge springs from the success of the system: the burden of uncompensated care falls disproportionately on Denver Health, which provides 30% of all uncompensated care in the state. The enormous growth of care to uninsured, which doubled from $1 million in 1990 to $2 million in 2001, is the greatest challenge for the future. As a percent of operating revenue, charity care and bad debt runs upward of 50%. Attempts to decrease cost while improving care hold some promise. However, federal, state, and local funding streams are not keeping pace with this growth, raising the question of sustainability. Sources: Gabow P., Eisert S., and Wright R. Denver Health: A Model for the Integration of a Public Health Hospital and Community Health Centers. Annals of Internal Medicine. 2003;138:143-149. Denver Health. Facts About Denver Health: An Efficient, High Quality Health Care System. 2004.