The Role of Faith Healing in Mental Health Seminar
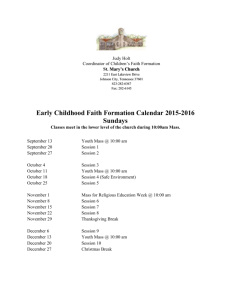
advertisement

The Role of Faith Healing in Mental Health Seminar Hosted by The Banyan Academy of Leadership in Mental Health (BALM) 12th November 2009 Su sh ru t, BALM ha s sse d th e n e xt Contents Page number 3. Background to the seminar 4. – 5. Mental health in India – Historical and Cultural Perspectives Dr. Anup Dar 6. Dava and Dua project ALTRUIST Project Founder Milesh Hanlai 7. - 8. Mental illness or Evil Spirits? Dr. Brigitte Sebastia 9. – 11. The Banyan – Community Mental Health Project (CMHP) Ms. Porkodi – Project Director 12. Faith Healing: Anthropological perspectives Professor Littlewood 13. – 14. Panel discussion: The role of faith healing in mental health care BALM would like to thank Anna Campbell for the compilation of this report. 2 Background India has a rich history of treatment of mental illnesses in traditional spiritual practices. Durgahs, temples and churches are just a few examples of places where people seek cure for various ailments. In addition to these remedies rooted in religion, there are several ancient medicine systems such as Ayurveda, Siddha and Homeopathy that provide treatment. Faith healing has been used extensively in India as a method of treatment of mental illness, especially in rural areas. Even though there might be no direct scientific proof for the effectiveness of faith healing, anecdotal evidence suggests that certain people benefit from faith healing, either in conjunction with allopathic medication or without. Several factors contribute to people resorting to faith healing as a means of psychiatric treatment. To begin with there is complete lack of awareness of mental illness being a treatable illness esp. in rural India and even where there is, there is a severe shortage of professional psychiatrists in the rural areas1, compelling people to access treatment by ‘faith-healing’ methods. Despite this however, faith healing is not always the last resort after seeking psychiatric treatment. It very often precedes other forms of treatment, since faith healing as a means of treatment is rooted in India’s cultural tradition and offers both reason and treatment for psychiatric ailments. This explains why faith healing is not just accessed by those in rural areas, but by the average urban Indian as well. Against this background, BALM organises a one day deliberation on ‘The Role of Faith Healing in Psychiatry.’ The seminar will provide a platform to a wide range of opinions and experiences on faith healing. Objective The objective of the seminar is to discuss the following topics: • • • What is faith healing? What are the operational aspects of faith healing? What are the factors that contribute to the popularity of faith healing as a treatment for mental illness? Topics • • • • Mental health in India – Cultural and historical perspectives Faith healing as a form of psychiatric treatment Case studies of people who have only accessed faith healing practices. Case studies of people who have accessed faith healing practices, as well as psychiatric treatment. 1 A recent article published in The Times of India on February 12, 09 ‘Just 3,300 shrinks for 13 crore with mental illness’ draws attention to the fact that India only has 3,300 trained practicing psychiatrist, out of which 3,000 practice in the four metros. 3 Mental health in India – Historical & Cultural Perspectives Dr. Anup Dhar Centre for Study of Culture and Society http://www.cscsarchive.org/irps/irp.2008-10-14.6748323572 Poses the question: is there space for faith-healing in the context of mental health in India? Dr. Anup proposed that historical and cultural perspectives of mental health in India must be contextualized within a geographical perspective. He uses the paradigm of maps to trace a journey through time and space and suggests that a ‘remapping’ is required to create a framework for mental health in India in which faith-healing works alongside a bio-medical model to form a true multi-disciplinary approach. Map 1: One dimensional Eurocentric map of bio-medicine In Map 1 he argues that time sets a particular frame distinguishing the ‘modern’ from the past. Biomedicine is considered modern and anything before this western medical revolution is considered pre-modern and is thus relegated conceptually and schematically to old. Faith healing falls into this category and is aligned with superstition, suggestive of lack in this model. He defines culture as the ‘difference that matters’ and suggests that within the first map there is no space for ‘cultural perspectives’ as all that is different is conceived as ‘pre’ or ‘prior’ and is therefore relegated to below and irrelevant. This perspective is ‘indifferent’ to culture and different perspectives and therefore allows no space for traditional healing methods. He suggests that the two main problems with this map are: - Space, in that none is made for faith healing and other cultural perspectives - Time, in that it is focused only on the period since the birth of the medical clinic and discounts all prior knowledge and practice Map 2: Stigma, pathology and the birth of the clinic The map addresses the beginnings of a multidisciplinary approach that begins to place psychiatry in a position in history and medical development rather holding it as the final ring on the ladder of development. The critical ideas here are interdisciplinarity and intradisciplinarity that emphasise the importance of placing studies and paradigms in their context in a scheme of development rather than at the pinnacle. Throughout history there has been suffering and methods of healing; psychiatry is one healing response to one kind of suffering. Dr. Anup then traced the birth of the clinic to illustrate this medical positioning and discussed medical paradigm changes in terms of what is ‘normal’ in the context of societal shifts in thinking. The birth of the clinic came 200 years ago as doctors’ anatomical understanding of the body increased. The clinical experience changed from a hearing experience (what is the matter with you?) to a seeing experience (where does it hurt?). Psychiatry however, remains in the hearing stage of this development and thus has something in common with older forms of healing. He talked about the notion of abnormal and how it has developed beginning as a large, ill-defined confusion of a definition that incorporates anything physically or sexually unlike ‘us’ for example Siamese twins or hermaphrodites. The definition was honed over time and now rests as more of a 4 ‘moral’ monster – a movement from the flesh to the mind that was developed in the context of Christianity. All these definitions place parameters by which a person is diagnosed and laid the foundations for diagnositic criteria for mental health disorders. Map 3: Places psychiatry in perspective as part of the CUSP map of mental health care. This map places all aspects of treatment on one plane demonstrating that the medical experience is just one option within a range that includes: • Medical experience • Non (A-) Medical Experiences o Formalised as in Ayurveda o Faith healing and cultural questions • Community mental health which sits in the middle and incorporates both, bridging the gap Here Dr. Anup also pointed out that the medical experience is an individual experience and also and institutionalized one – faith healing and other alternative treatments are more of a community based approach that needs to be accommodated in the model of care. Questions Lucie Potter, a volunteer at The Banyan asked: How can we practically achieve the integrated approach? The response was that the sector needs to assess how many different options there are available in the sector and how many different languages they are speaking. This would establish an understanding of compatibility. He also pointed out, continuing with the language metaphor, that if one language alone is adopted to speak for all options, it remains specific and uniform for such a diverse audience. A point was made by Dr. Lalit from Bangalore who suggested that it was perhaps not a common language, but a common space that is required for progression. He talked of the politics of engagement and raised the point that the way people engage with a power system is based on their context; creating a more neutral setting for engagement may have positive effects. A question was asked: Where does the map go from here? Where is CUSP going? Dr. Anup emphasized that the work of CUSP is respectful of all systems of care and is working towards an integrated, yet interrupted system of care that does not reduce differences in practices to lack (as per the first map). 5 ALTRUIST Founder – Dava-Dua Project Milesh Hamlai Milesh described his experiences in providing psychiatric services to a durgha in Gujarat. He described the Indian context where religion and health go hand in hand and traditionally medication and treatment has been sought from religious establishments. It is from this stand point that his team began their interactions with an 800 year old durgha that has a reputation of badly managing patients and of human rights issues. The project is a public-private partnership between the government, Altruist and the durgha designed to integrate psychiatric, bio-medicine into the religious practice at the site without questioning the religion itself in any way. To integrate the two practices they have trained the Priests to identify mental illness that would benefit from bio-medical treatment and then to direct those patients to the psychiatric services provided by Altruist. In the Indian context there is a missing link between health care services and the client. This could be due to a lack of understanding of mental illness, a lack of psychiatric services in Primary Health Centres or to the preventative costs associated with private practice; this gap is bridged in this instance by the faith healer who can identify and direct clients to the care they require. The project incorporates training of identification of mental illness with some therapeutic and counseling training so that Priests at the durgha can speak to devotees about their illness and their medication on using their language and in a setting in which the clients are comfortable. The project has achieved many of its aims and shown that the durgha was willing to work with psychiatric services in an integrated model of mental health. Questions: How long is such a collaboration possible before bio-medicine takes over in these circumstances? Milesh stated that this is a pilot-project with the objective of bringing the two together not for one to dominate. The project was started in response to human rights violations and its aim was to bring together and not to take over. A point was made about the acceptance of help – with the anecdote described of the common people that protested at the request for psychiatric services at a particular PHC because they did not want the integration of the two types of client. Jane Derges of the UCL team asked if any of the priests had left the durgha to become mental health professionals? Is it part of the aim of the project to get people from the durga to work as mental health professionals? Milesh answered that nobody had left the durgha as a result of this project, nor was that one of the aims of the project. These families have been healers for generations. However, through the partnership it was envisaged that the Priest’s children would have the opportunity to go to school. One participant noted that this is the introduction of psychiatry into religion and asked if religion would ever enter into psychiatry? The importance of the training of Priests was expressed in the light that people may discuss their issues more freely with the Priest rather than a counselor. Have the faith healing techniques changed? Milesh said he was not in the best position to answer this question but the durgha is 800 years old and in his opinion the techniques have been diluted over time and are perhaps not as intense or involved as in the past. 6 Mental illness or Evil Spirits? Dr. Brigitte Sebastia Dance of St. Anthony: Devotion, Affliction and Possession Puliyampatti The clients in this video fell into three categories: - Those suffering from severe mental illness (such as bipolar and schizophrenia) - Those affected by domestic violence (mainly women) - Those suffering from incurable diseases and rejected from the hospital The video drew particular attention to the rituals at St. Anthony’s – other activities also take place at the shrine aside from this. The community comes together here and moves fluidly between the shrine and the town outside. She explained that it was a system controlled by patients and posited that many of the behaviours exhibited were a mechanism for escaping tension; those that have deep family or personal problems become ‘possessed’ and those with other mental illnesses tend to behave very differently. She explained that many clients had visited Psychiatrists before coming to the shrine but discontinued because of: - Lack of money - Bad psychiatric practice She elaborated on the problems clients had with Psychiatrists: - They only addressed the care giver and not the client with their limited repertoire of questions - The prescription is given to the family member - No information is provided on illness or medication Questions Why do people visit the shrine of St. Anthony? 64% of 67 devotees had already accessed psychiatric treatment before visiting the shrine. In her opinion biomedical treatment had failed due to a combination of lack of money to fund treatment and individual cases of bad psychiatric practice. Examples included the psychiatrist talking only to the care giver and not the client and therefore not exploring the symptoms completely; sourcing of medication from only a small selection controlled by the psychiatrist; limited/ no information supplied to the client on their illness, medication or possible side effects. Together this lead clients to have little faith in government hospitals and bio-medical treatments. The high level of mental health issues in India is not a result of the lack of psychiatrists but of the failure of psychiatry as a discipline to engage with the community and address the needs of the people. Experience from a Delhi clinic of one participant working with psychiatrists demonstrated that a presenting patient’s current prescription was treated as evidence of a diagnosis and therefore a proper assessment was not undertaken. Dr. Anup posed the idea of spectacle - comparing the participants to those in wrestling for the nature of the reaction they spark in the audience. Is St. Anthony’s representative of faith healing? 7 Brigitte supplied the context for the shrine in terms of location and denomination and suggested that the video did not seek to be representative of all faith healing – just to show the practice at St. Anthony’s. How long did the performance last? The performance started slowly as devotees gathered in the space, slowly building up to a frenzy in time with the music and stimuli. The actual ritual lasted only 15 minutes in total; as the music died down, the devotees slowly recovered themselves, tied up their hair and walked away. 8 The Banyan – Community Mental Health Project (CMHP) Ms Porkodi – Project Director Other guests presented by The Banyan Gajalakshmi, Kavitha and Murthy – Community Workers at The Banyan - Mother of a client of The Banyan: - Daughter has Schizophrenia and lived in the durgha for 3 years - Resisted treatment at the health centre and eventually decided to take medication but not leave the durgha Sudha - Client of The Banyan - Predicted the Tsunami - Diagnosed with schizophrenia - Will not take medication Allahudin - Faith healer/ private - Informal referral relationship with The Banyan CMHP is a new experience for The Banyan which started as an institution-style home for mentally ill women in Chennai. CMHP was designed to provide accessible mental health care in a rural setting. Based on the same design as the District Mental Health Programme, CMHP integrates physical and mental healthcare in the same outlet. Mental health services include allopathic medicine, psychotherapy, family therapy, day care centre activities, awareness campaigns and other engagement practices. Referrals to CMHP come from various sources including Panchayat members and youth clubs alongside local faith healing sites: a temple, a durgh and independent faith healers. The philosophy behind all of The Banyan’s projects is the provision of healthcare for all in the format that is most accessible. The cultural context of India requires sensitivity when offering health care services that are not always respected and integrated by government bodies. The focus here is on the engagement of clients that need treatment in the manner most suited to themselves so as they achieve a level of health. The example was given of a man that receives a combination of treatment. He doesn’t know which helps him so he continues to receive treatment from all. One main issue is a lack of awareness. Clients either don’t know about psychiatric treatment or experience bad practice and then shift back to faith healing. The Banyan client experiences of faith healing at sites local to CMHP Durgha: Porkodi explained that although the practices at Durgha (chaining etc…) appear disturbing to an outsider, after speaking to the client you can understand that there is nothing else to be done with the limited resources of a poor family and the challenging behaviours exhibited by the client. The durgha provides a safe environment, stopping the client from running away and being a danger to themselves. The durgha provides a space for clients to express themselves and for all to make contact with those in a similar position. Temple: Porkodi described the performance in the temple that is orchestrated by those that stay in the temple. The atmosphere and behaviours build up as the gathering waits for the Deity. The ‘performance’ only occurs at certain times of the day – not during all of the pujas that are performed. Porkodi commented that the openness of faith healing centres is admirable. In this environment, people are free to express themselves however they want – unlike in an institution. There is no judgment. 9 The system in the local Gunasheelam Temple is such that all devotees are those that have recovered as a result of their treatment at the temple. They continue to follow the systems of the temple that helped them recover. In The Banyan’s experience, it is possible to rehabilitate patients only once they are in tune with reality – the connection to everyday life required. The temple offers a setting for this as it provides routine, functions and people that are based in reality. The culture provides a support system for a the mental health issue. Guest experiences Faith healer He explained that he addresses the whole problem, from the root cause, to its symptoms. He said that he felt that seeking out biomedical treatment is a case of money; if a client has paid for some treatment then it feels strange to then accept that free treatment can work. In order to become a healer it requires austerities, everyone has the ability but takes great dedication to use it. He questioned why we give medication for the body when it is the spirit that is the problem? Medicines reach out to the spirit. In his experience the fight is between the spirit and the deity – injury is to the spirit and not the individual. How do you decide who to refer to The Banyan? Can decide when he sees the client individually. 11 days intense therapy then 3 months of connection via photo and durgha. Doesn’t distinguish mental health problems and can cure most problems. The clients 1 = Mother client, 2 = Sudha How did the change come about within you/ your daughter? Can you pinpoint how the change happened? 1. Both the centre and the durgha – both helped a bit 2. Medication helped her sleep. Have you faced stigma? 1. Her daughter behaved very badly but no one said anything derrogatory in front of her. The question was asked, ‘did they look at you differently?’ and she replied that she was never ostracized. 2. Her symptoms were withdrawal and not aggressive, therefore the community felt sad for her. She felt that nature was speaking to her heart. Does the healer have special power or is it knowledge that can be learnt from a book? 2. God is there in every individual and it’s about how you realize the God. The healer will have read something and learnt things that can be used to heal in combination with the power. God provides the way Does the doctor work in the same way as a faith healer? 2. Same in a way; doctor gets rid of illness and the faith healer treats the spirit. God is love and out of love both the doctor and the faith healer practice. Neither are God. Why did you feel that you were well/ not well? 10 10 2. She always felt connected to God (a particular Goddess) and had a dream that instructed her not to get married or lose her virginity – the dream explained that if she followed this it would be good for others. At that time she felt some witchcraft that was done against her – someone fell in love with her. The thoughts of this person were caused by witchcraft. She has experience the fusing of the evil spirit with her body. This was her illness. What does she think of the diagnosis of Schizophrenia? 2. Her symptoms included lack of sleep and a delusion of pregnancy along with obsessive thoughts of God. These symptoms were reduced by medication. She said that she was never mentally ill, just lack of sleep that was the problem – witchcraft caused this symptom. Mother client: How does she feel about the temple and about The Banyan? 1. Both just as good as each other. Sudha: Does she have other things to give to people? 2. She stayed longer at CMHP because she liked helping the people around her. The doctor told her to stay and help and she stayed because she wanted to help. 11 11 Anthropological perspectives on faith healing Professor Roland Littlewood, University College London Professor Littlewood posed that the description ‘faith healer’ is misleading; he used the term traditional/ alternative healer. Is faith healing universal? Societies have desired and undesired states of being. Methods to turn client back to desired state. This is universal definition. The term can include all sorts of activities including hypnotherapy and counseling. Symbolic healing has properties that are in common around the world. 1. Experience of the healer and the to be healed explained by the term myth – both sides come from the same culture and share these myths. Experience is explained by this. The two share a mythical culture. 2. The sufferer defines the problem in terms of the myth (cultural explanation) and the therapist fully explains the problem in terms of the myth to be understood by both sides. Representation of the myth – stethoscope, couch puts the myth in context (non verbal). The healer provides a verbal or non verbal explanation by making assumptions on the interactions shared by the two sides. 3. Dowl: Healer transfers the patient’s story into symbols. Symbols suggest they are experiencing something and form a link between the myth and the personal experience in their mind. 4. The healer manipulates the myth further. Problems with the model: - Does technological transformation also take place in the medical model - Is this only anthropological or is it in the patient’s experience? Do individuals have to be aware of the symbols? - Single healer - How can we measure efficacy? Example: Levi-Strauss studied a woman in obstructed labour in an Indian community in Panama. Resolution involves the myth provided by the Shaman. The explanation: the power is located in the womb, the Mu (mythical goddess) is jealous of the mother and will not allow the baby out. Together both the mother and the healer engage in the myth linking the physical with the cognitive. The shaman creates figures and tells the story. The figurines are used to indicate a visual journey up the vagina of the woman to confront Mu and to release the baby. - Different levels of the myth – the shaman links the levels together in a language that she his experience of to relax the woman in order that she can deliver Collective healing Where healing slides into ritual – for example at Carnival time when everyone comes together and releases their problems. Turning things upside down. Cultural schemas that have developed around ailments: Chief Ship of the Scrotal Hernia – Congo: in this culture the hernia would be very debilitating and those that suffered from it would not be able to go out and hunt. As a result of this they became political figures, earning the title the Chief Ship of the Scrotal Hernia. In Rwanda in 1950s there was a drum society for people that experienced bad dreams about Europeans. Alcoholics anonymous - displacement of agency for illness onto God. This is an example of symbolic healing forming a part of biomedicine. 12 12 Panel discussion Dr. O. Somasundaram, psychiatrist Dr. Sushrut Jadhav , University College London Dr. Roland Littlewood, University College London Dr. Harish Naraindas, Jawaharlal Nehru University, Delhi Dr. Brigitte Sebastia, French Institute of Pondicherry Mr. Allahudin, Traditional healer, Kovalam Moderator: Dr. K.S. Jacob, CMC, Vellore Dr. O. Somasundaram pointed out that mental diseases are brain diseases, but that medicines do not work in all people. So additional help from other traditional ways of healing is very necessary. For example, very old form of healing such as Jainism etc. treated people with mental illness with compassion. Temple treatment is very popular Gunasilum temple reduces aggression Routine in temple habits are trained at these places What contributes to the popularity of faith healing? - Dr. Sushrut: Attributed it to the failure of established psychiatry to provide the services it should do. - Prof. Harish: Referred to the client of The Banyan whose daughter was chained at the durgha. He highlighted that the durga provides a sanctuary with activity not available elsewhere. - Prof Littlewood: Is money an issue? Are middle class people going to a traditional healer because they want something a bit different and non-medical? Insights from hospital ethnographies suggest that the outside culture is represented inside the hospital (with temples and other structures finding their place). Perhaps hospitals should be made more permeable and more open to the outside world. Part of this includes the dismantling of structures and colonial concepts of the mind. The significance of Jerome Frank’s work on ‘non specific issues in psychotherapy’ was raised highlighting that it is a series of activities that cannot be directly controlled or predicted that contribute to recovery. Faith healing is one such factor. One issue is that there is no dialogue at the moment between different methods of healing. We are all trapped in our own frameworks and difficult to see other’s point of view. The points of view are diverse and one framework may be more useful than others; and yet no one perspective provides complete solution or even an understanding. This point was developed and it was posited that experts are trapped in the framework but people hold a variety of beliefs and models. Professionals cannot integrate everything or often even fully appreciate because they are stuck in their background. How can we provide a package that includes all perspectives? Can we talk across disciplinary frameworks? There are no exclusive solutions for mental illness and therefore people are open to seeking various treatments. 13 13 The biomedicine perspective is happy to incorporate things that are understood (e.g. yoga) but religion is not studied and understood well enough yet in a scientific way in order that it can be accepted. The faith healer crossed the divide by incorporating various myths from various religions. If he can bridge the gap, why can’t others? Why do people go to the faith healer? Because the hospital has failed! Are there levels of faith healing care as in biomedical care? Charges are based on the individual and therefore it has the benefit of affordability. These arethe only levels to consider. It was posed that faith healing has a role in neurotic disorders but not in psychotic. This was dismissed as too simplistic an explanation to account for all the factors involved. The fact is that there is no generic solution, only individual solutions for problems based on cultural perspectives. Faith healing brings in the larger meaning making layer that therapists often try and encourage clients to access. Both sides are perhaps treating symptomatically and in this case have more in common that we think. 14 14