pulmonary development
advertisement

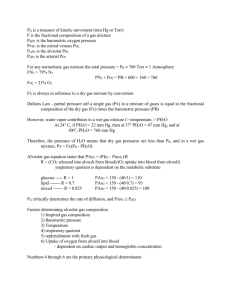
Any tissue allowing for gas exchange is respiratory in nature. By this definition, ALL tissues are respiratory tissues. Discussion restricted to specialized tissues allowing gas exchange exceeding that needed by the tissue. More similarities in lung structure than any other organ with respect to species differences. Organ engaged in chemical exchange with a gas mixture whose chemical composition varies within only very narrow limits in that small portion fo the atmosphere where mammals normally live. Most differences in amount and disposition of smooth muscle, cartilage, collagen and elastin (having to do with strength of forces acting on bronchi and peribronchial tissues). Remarkable similarities in respiratory lobules and alveoli. Lungs of larger and more active mammals have a larger number of primary and secondary lobules. Importance of understanding lung development during this period: respiratory distress syndrome, SIDS, asthma. The pharyngeal region is the one usually most intimately associated with development of respiratory tissue in most vertebrates. The embryonic endoderm forming the lining of the pharynx is characterized by the potential for a high degree of vascularization, as in embryonic endoderm elsewhere. During fetal development, placenta acts much like an elaborate external gill, allowing gas exchange between the fetus and the environment. Because of this, the fetal lung has no contact with the future external environment, and developing lungs have no function or immediate respiratory value to the fetus. The neonate, however, depends for survival on the rapid establishment of efficient gas exchange in the lungs. Fetal lung, however, does possess importance. Acts much like an exocirne gland in late gestation. Production of surfactant occurs prenatally. Development is proximodistal in nature in terms of differentiation and specialization. Alveoli are endodermal in origin and epithelial in nature. Newborns are obligate nose breathers, occlusion of the nasal passages will result in death by suffocation. Infants can inhale through the mouth only by extending the cervical spine and opening the mouth wide to retract the epiglottis. Oral and pharyngeal suction therefore does more harm than good by removing secretions that are unlikely to enter the laryngeal lumen, and potentially inducing laryngeal spasms. To prvent inhalation of mucus secretions with the first breath, compression of the thorax would be more helpful in cesarian-derived infants than suction. Three stages in fetal lung development: 1) a "bronchial" or "glandular" stage, where terminal bronchial tubes are seen to have a blind ending lined by cubical epithelial cells 2) a "duct" stage, where bronchioles end in wider ducts lined by a respiratory membrane which is capable of supporting gas exchanges in air 3) an "alveolar" stage, where alveoli develop in the walls of the ducts Lung developmental stages difficult to study in postmortem infants due to gasping causing inhalation of any materials in the respiratory system directly into the lungs. Gasping while glottis is closed or amniotic membrane covers nares will cause profound changes in appearance of lungs, capillary and venous engorgement, often heavy hemorrhage. Because of pliability and deformability of tissue, handling and fixing procedures will also alter microscopic appearance. Fixing agent MUST reach all areas rapidly AND uniformly or results are useless for descriptive purposes. Fetal breathing movements much debated. Stress may cause fetus to gasp in utero, and lumina will be shown to contain mucus and amniotic debris, possibly with vascular engorgement . Fetal lung fluid is produced by lung, and fluid in bronchi and trachea is maintained under pressure by the action of the laryngeal sphincter. Pulmonary arterial pressure high in fetus, as left and right ventricles about equal in thickness in fetus, as opposed to diffences of about three-fold in adult. Pulmonary walls and arteriolar walls are about three times thicker in fetus, and maintain that difference postnatally under conditions of persistant pulmonary arterial pressure postnatally (hypoxia). Pleural lymphatic vessels hard to see in normal fetal lung near term, due to high positive pressure in lobules. The first breath causes a dramatic reduction in the pressure outside the pleura, thus allowing lymph flow through the connective tissue matrix of alveolar walls. Under normal conditions in utero, there is a continuous cycle of expansion of alveoli, associated with an increase in fluid pressure, and passive contraction as fluid escapes through the bronchiole, venule, or lymph vessels. High glycogen content in early development in bronchial buds (first described by Claud Bernard in late 1800's). Importance never concluded. Glycogen in later development is always in walls of small bronchi, never in alveolar wall cells. Important in histochemical differentiation of cell types in lung. Can be found extruded in lumen during expansion phase, and may be utilized there. Lung fluid pH is as low as 6.4, which is optimal for activity of glucose-6-phosphatase. Surfactant production occurs late in fetal life. Produced cyclically by pneumocytes. At start of cycle, pneumocytes show accumulation of phospholipid intracellularly. Phosholipid exocytosed into lumen as cycle continues, and then allowed to enter bronchial tree as spincter relaxes. Appears to continue to be concentrated in lumen, as it has not been observed in blood and lymph of lung. During final phase, cell proliferation occurs, and phosholipid production temporarily ceases. Lung fluid escaping the laryngeal sphincter is immediately swallowed; the contribution of this acidic, high-fat fluid to the development of gastrointestinal function has not been investigated. At birth, changeover occurs from vagal to sympathetic neural dominance of respiratory tract. During normal birth, thorax is compressed, eliminatring some of the fluid from the tracheobronchial tree, especially the mucus in the upper portions of the tract. Thoracic recoil, together with the expansion by means of respiratory muscles, produces a pull on the lungs, which is transmitted, via the pleura and other connective tissue elements, to every component part of the lungs. In particular, lymphatic vessels and veins are opened up, increasing the flow of both lymph and blood and decreasing pulmonary arterial pressure. This results in a rapid removal of any components of lung fluid capable of resorption. Surfactant not resorbed, but becomes "plastered" on the walls of the lungs in high quantity at the air-fluid interface. Infants (and adults) use only small percentage of lung surface area for gaseous exchange at any particular time, as perfusiondiffusion gradients established. Any sympathetic stimulation (excitement, exercise) cannot cause extended use of whole lung. Positive-pressure respiration does and results in atelectasis. Regulation of cyclicity not determined.