comp1_unit9d_audio_transcript

Introduction to Healthcare in the US: The Evolution and Reform of Healthcare in the US
Audio Transcript
Slide 1
Welcome to Introduction to Healthcare in the US: The Evolution and Reform of
Healthcare in the US . This is Lecture d.
The component, Introduction to Healthcare in the US, is a survey of how healthcare and public health are organized and services are delivered in the US.
Slide 2
By the end of this unit, The Evolution and Reform of Healthcare in the US , students will be able to:
describe evidence-based medicine, clinical practice guidelines, and quality indicators in medicine;
describe the patient-centered medical home model; and
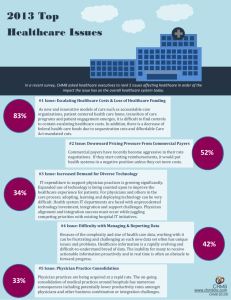
discuss the key issues driving healthcare reform in the US.
Slide 3
This lecture will discuss the patient-centered medical home.
The patient-centered Medical Home is a model of providing primary care that is comprehensive and takes into account the needs of the patient, as well as the clinician.
The concept has been around for many years. In 1967, the American Academy of
Pediatrics, or AAP [A-A-P] , initially introduced the medical home concept as a central location to archive a child’s medical records.
By 2002, the AAP [A-A-P] expanded the medical home concept to include specific characteristics of patient care - that patient care should be accessible, continuous, comprehensive, family-centered, coordinated, compassionate, and culturally effective.
Slide 4
Other organizations, such as the American Academy of Family Physicians (AAFP) and the American College of Physicians (ACP) have developed their own approaches for improving patient care. The AAFP calls it “the medical home model,” while the ACP calls it “the advanced medical home.”
Slide 5
In 2007, the American Academy of Family Physicians, the American Academy of
Pediatrics, the American College of Physicians, and the American Osteopathic
Association, combined their efforts and drafted “The Joint Principles of the Patient-
Health IT Workforce Curriculum
Version 3.0/Spring 2012
Introduction to Healthcare and Public Health in the US
The Evolution and Reform of Healthcare in the US
Lecture d
1
This material (Comp1_Unit9d) was developed by Oregon Health & Science University, funded by the Department of Health and
Human Services, Office of the National Coordinator for Health Information Technology under Award Number IU24OC000015.
Centered Medical Home”. They modeled the medical home as a method to provide comprehensive primary care for children, youth, and adults. They felt that the patientcentered medical home was a healthcare setting that would facilitate partnerships between individual patients, their physicians, and when appropriate, the patient’s family.
Slide 6
We are now going to look at some of the elements of the patient-centered medical home or PCMH.
The first characteristic is the concept of a personal physician. Each patient has an ongoing relationship with a personal physician. The physician is trained to provide continuous and comprehensive care and often acts as the first contact for the patient in the healthcare universe.
The patient-centered medical home embraces the concept of a physician-directed medical practice. The personal physician directs care for the patient by leading a team of individuals at the practice level, and while the team takes collective responsibility for patient care, the physician often coordinates the activities of the team.
Slide 7
Another characteristic of the patient-centered medical home is the concept of whole person orientation.
This suggests that the personal physician is responsible for providing all of the patient’s healthcare needs. The physician may seek assistance through consultation from other clinicians, if appropriate, but aims to provide care for the patient in all stages of life.
Care is provided in the acute, chronic, and end-of-life settings. Preventative services are emphasized and provided by the personal physician.
Slide 8
The patient-centered medical home mandates coordination of care. Coordinated or integrated care is provided to the patient across all elements of the healthcare system and within the patient’s community.
Care is facilitated by technology so that patients get appropriate care when and where they need it. Clinicians are trained to provide care that is culturally and linguistically appropriate.
In this setting, the healthcare system includes subspecialty care, hospitals, home health agencies, or nursing homes. The patient’s community includes family, public, or private community-based services; and the concept of technology includes electronic health records, health information exchange, information technology registries, and other means to provide appropriate care.
Health IT Workforce Curriculum
Version 3.0/Spring 2012
Introduction to Healthcare and Public Health in the US
The Evolution and Reform of Healthcare in the US
Lecture d
2
This material (Comp1_Unit9d) was developed by Oregon Health & Science University, funded by the Department of Health and
Human Services, Office of the National Coordinator for Health Information Technology under Award Number IU24OC000015.
Slide 9
Quality and safety are important characteristics of the model. Quality and safety measures are incorporated as an essential component of patient care. Patients are encouraged to achieve patient-centered outcomes and are assisted by a care planning process a nd a strong partnership between the physician, the patient, and the patient’s family.
Clinicians use evidence-based medicine and clinical decision support tools to guide their decision making in order to ensure a standard of quality and safety that is acceptable.
Slide 10
The patient-centered medical home emphasizes quality and safety of care. The model uses information technology to support patient care and makes use of tools such as performance measurement, patient education, and enhanced communication to improve quality and safety.
Further, practices go through a voluntary recognition process by an appropriate nongovernmental entity (for example, by NCQA's PPC-PCMH recognition program) to demonstrate that they have the capabilities to provide patient-centered services consistent with the patient-centered medical home (PCMH) model.
Slide 11
Participation is an important aspect of maintaining quality and safety in the PCMH model. Physicians participate in continuous quality improvement and performance measurement.
Patients participate in decision making and are able to provide feedback if their expectations are being met, or if they are not, both patients and their families participate in quality improvement activities.
Slide 12
The patient-centered medical home also enhances access to care. It specifies improvement in the current model of care access and facilitates the availability of clinical services for patients by using innovative methods of scheduling, such as open access scheduling in the outpatient setting, by expanding hours for clinician/patient contact, and by offering new options for communication between the patient, their personal physician, and the practice staff.
These options may be implemented using methods such as secure online messaging between clinicians and patients, and the use of personal health records.
Slide 13
In the traditional model of medical care, payment for healthcare services typically reflects face-to-face services provided by the clinician to the patient. In the patient-
Health IT Workforce Curriculum
Version 3.0/Spring 2012
Introduction to Healthcare and Public Health in the US
The Evolution and Reform of Healthcare in the US
Lecture d
3
This material (Comp1_Unit9d) was developed by Oregon Health & Science University, funded by the Department of Health and
Human Services, Office of the National Coordinator for Health Information Technology under Award Number IU24OC000015.
centered medical home, the payment model is enlarged to appropriately recognize the added value provided to patients who select the patient-centered medical home. It also reflects the value of physician and non-physician staff, and patient-centered care management work that falls outside of the face-to-face encounter.
Payment for coordination of care includes care provided within a given practice, as well as care provided between consultants, ancillary providers, and community resources.
These options include payments for face-to-face visits, and also for services associated with coordination of care.
Slide 14
So, the payment model associated with the patient-centered medical home recognizes the value of physician work that is not necessarily delivered in a face-to-face environment with the patient. For example, if the physician remotely assesses patient clinical data, then there is a methodology of payment for these services.
There is also a methodology for payment reimbursement for enhanced patient communication access to clinicians, including secure email, telephone consultations, and consultations between an interdisciplinary team that provides care.
Additionally, the model also recognizes case mix differences in the practice patient population. A practice that has a larger number of more complex patients has payment options that are weighted to reflect the complexity of their population.
The model also allows for additional payments when measurable and continuous quality improvements are achieved and surpassed. It also covers enhanced patient communication, access to clinicians, and supports the adoption and use of health information technology for quality improvement.
Slide 15
This concludes Lecture (d) of The Evolution and Reform of Healthcare in the US . In summary, this lecture described features of the patient-centered medical home including having a relationship with a personal physician; a team approach to care; a whole person, integrated approach to care; care that includes quality and safety measures; enhanced access to care for patients; and payment that recognizes the added value of the patient-centered medical home.
Slide 16 (Reference slide)
No audio end
Health IT Workforce Curriculum
Version 3.0/Spring 2012
Introduction to Healthcare and Public Health in the US
The Evolution and Reform of Healthcare in the US
Lecture d
4
This material (Comp1_Unit9d) was developed by Oregon Health & Science University, funded by the Department of Health and
Human Services, Office of the National Coordinator for Health Information Technology under Award Number IU24OC000015.