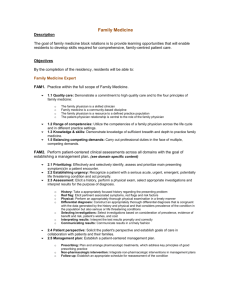
Dr_Wild_Engaging_Physicians_in_Patient_Centered_Care_Final
advertisement

Engaging Physicians and Patients in Patient-Centered Care Dorothea Wild, MD, MPH, Dr. med. Griffin Hospital Overview • • • • Explore barriers to physician engagement in patientcentered care Evidence supporting effective patient-centered communication Discuss strategies to engage physicians at all levels in patient-centered care: – Motivate – Activate – Monitor Why is “weigh yourself every day” so hard? Engaging patients in managing their disease Why is it so hard to bring the MDs around? • • “I have many patients who would like nothing more than to spend 23 hours with me to go over every news report they have heard about a rare disease. I have patients who would like me to mediate the problems between their daughter and son-in-law, and those that just want to discuss politics and religion with me.” “Why should a patient bother to consult a physician if the patient does not want professional care? (…) It is important to distinguish between a poor bedside manner and the expertise that develops from many years of training and experience. (…) Dr. Berwick is totally out of touch with clinical medicine and one wonders if he has ever been in medical practice.” New York Times responses to Don Berwick article about patient-centered care Physician Barriers… The Problem • Perceived contradiction between evidence based care versus patient centeredness • • • • • Time constraints Fear that engaging patients would lead to overwhelming demands on time Lack of knowledge and skills No incentives for communication/coordination Impression that Institution/Medical staff does not value communication How to Motivate Physicians Motivate: Make it important Make it evidence-based Make it about their patients Activate: Show them where they are Give them actionable things to do Monitor: Monitor the data Give regular feedback Good News: Communication Improves Outcomes Good physician communication: • Increases patient adherence • Increases satisfaction • Decreases anxiety • Leads to more accurate recall • Improves management • Decreases inappropriate utilization of resources • Decreases litigation Bartlett et al. J Chron Dis 1984;37:755-764; Stewart 2002 Patient-Centered Communication is More Scientific “History-taking, the most clinically sophisticated procedure of medicine, is an extraordinary investigative technique: in few other forms of scientific research does the observed object talk.” Alvan Feinstein, Clinical Judgement 1967 “A successful dialogue between patient and physician is at the heart of working scientifically with patients.” George L. Engel, 1995 Used with permission from Auguste Fortin III It’s hard to be a patient… Patients’ recall of their discharge info: • • • • 27.9% were able to list all their meds 37.2% were able to recount the purpose of all their meds 14.0% were able to state side effects 41.9% were able to state their diagnosis Makaryus & Friedman Mayo Clin Proc 2005;80(8):991-994 Motivate: Speak With the Voice of the Patient Survey Patients while hospitalized, there is technology available to help (www.howsyourcare.org) Patient call backs 48 hours after discharge Focus groups Call fall-outs on HCHAPS scores to elicit more data Patient Call Backs • • • • • • • How are you feeling since the discharge? Are there any new or worsening symptoms? Did you understand what you were treated for? Did you get all your medication filled? Do you have concerns or questions about your medication? Do you know the doctor who was in charge of your care? Did you get a follow-up appointment scheduled? HCAHPS Call-Backs When you were asked “how often did your doctors explain things well, you said usually. What would it have taken for you to say always?” Answer: “I was actually thinking about Dr. X, when I answered those questions. He seemed so aloof and very cold. He did a colonoscopy on me and when I woke up, he quickly told me I had a mass and went away. He did not stay back to explain to me what it means and what would be the next steps.” Activate: Show the Data • • • • Analyze HCAHPs MD scores: – Attending – Nursing unit – HCAHPs question BUT: Patients aren’t the only ones who observe MD communication! Survey house staff/midlevel providers regarding attending teaching behavior and hidden curriculum Survey nurses regarding physician behavior Survey Items from hidden Curriculum Survey • How often do faculty/residents/interns: – Encourage patients’ participation in their care – Take seriously patients’ concerns – Develop good rapport with patients – Explore emotional aspects of patients’ illnesses – Communicate interest in the patient as a person Adapted from: Beckman, : Haidet P, Kelly PA, Chou C, et al. Characterizing the patientcenteredness of the hidden curriculum. Acad Med 2005;80:44-50 Survey Items from Nursing Survey How often does this provider (resident/faculty): Communicate concern in patients as unique persons Encourage patients’ participation in their own care Explore emotional aspects of patients’ illness Provide patients with a clear understanding of their plan of care Handle demanding interpersonal situations in a respectful and effective manner Listen to you and considers what you have to say about patients’ care and concerns Respond in a timely manner when notified Adapted from: Wooliscroft et al. Acad Med 1994;69:216-224 Ask for concrete things to do: “Say: What Else?” Physician Centered: MD: What brings you here today? Pt: I have headaches. MD: Where are the headaches? How long do they last? What do you do to relieve them? Patient Centered: MD: What brings you here today? Pt: I have headaches. MD: What else? Pt: Well, I have trouble sleeping MD: What else? Pt: I am very worried about my son. He is using drugs. Barrier et al. Mayo Clin Proc 2003;78:211-214 OSCE (Objective Structured Clinical Exam): Tool to provide feedback Resident script: It is morning and you are about to visit a patient in her room. (…) you received sign-out that this patient is coming in for pancreatitis, possibly alcoholic. Your goal for the next 6 minutes is: - establish a therapeutic relationship and assess her understanding of her admission diagnosis. Patient script: You are upset because you think that people are accusing you of being an alcoholic. You are convinced that your pain is from eating bad food. Taped and viewed with chief hospitalist/external expert During Rounds • Model patient-centered behavior • Discuss evidence for patient-centered care • • during rounds Instill the habit to end each encounter with “can you explain the plan for the day?” Use the teach back method – “So, Mrs. X. What do you understand about what brought you in here?” Monitor: Track Data • Track patient-centeredness as performance metric in resident and hospitalist files • Track HCHAPs score, How’s Your Care scores for groups and individual physicians • Periodically repeat hidden curriculum, nurses survey for improvement Monitor: Provide Feedback • Provide direct observation • Provide patient comments • Provide concrete behaviors to implement • Example: Sit down, ask a question, smile, and listen for 2 minutes without interrupting • Example: Patient said “all my friends smoke” – how could you respond in an empathetic way? Why is “weigh yourself every day” so hard ? Barriers to self-management • • • • Multiple barriers to patient adherence – Financial and practical – Motivational – Cultural competency and health literacy – Health beliefs, external locus of control Relationship with provider crucial to identifying and overcoming those barriers Tools to activate patients and communicate in culturally and linguistically appropriate manner Consistent monitoring and coaching Expanding the partnership outside the hospital • Accountable care will require hospitals, SNF’s, VNA’s, and PCP’s to engage patients • Building partnerships across continuum of care • Putting patients and care partners at the center of care transitions • Holding each other accountable