Cirrhosis ppt - print and bring to class
advertisement

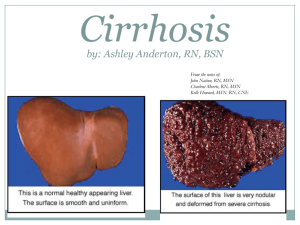
Cirrhosis Ashley Valentino Fall 2013 From the notes of: John Nation, RN, MSN Charlene Morris, RN, MSN Austin Community College Cirrhosis Facts: Progressive, leads to liver failure Insidious, prolonged course What does this mean? 9th leading cause of death in U.S. Twice as common in men Highest incidence between ages 40 and 60 What is Cirrhosis? • Extensive destruction of liver cells • Cells attempt to regenerate • Regenerative process is disorganized » Causes what? • Functional liver tissue is destroyed and scarring of liver occurs • Overgrowth of fibrous connective tissue, distorting liver structure; obstructing blood flow Four Types of Cirrhosis: • Alcoholic – formerly called Laennec’s • Post-necrotic • Biliary/obstructive • Cardiac Alcoholic cirrhosis: • Usually associated with alcohol abuse • Most common cause of cirrhosis • Causes metabolic changes in liver – fat accumulates in liver (fatty liver) • Fatty liver potentially reversible – How? • If alcohol abuse continues, widespread liver scar formation occurs What actually causes it? Post Necrotic cirrhosis: • Complication of: – viral infections – Toxicity • Which medications? – autoimmune hepatitis • 20% of of patient’s with chronic hepatitis C will develop cirrhosis • Broad bands of scar tissue form within the liver • Hep C + ___________= inc. the rate of cirrhosis? Biliary cirrhosis: Associated with chronic biliary obstruction and/or infection Primary sclerosing cholangitis? What is this? Diffuse fibrosis of liver Jaundice is main feature What actually causes it? www.humanillnesses.com Cardiac cirrhosis: • Develops from long-standing right sided heart failure • Results in patients with cor-pulmonale, constrictive • pericarditis, and tricuspid insufficiency What actually causes it? How do you treat this type? Diagnostic Studies: • Enzyme levels (AST, ALT) • initially elevated due to release from damaged liver cells • In end-stage liver disease • AST & ALT may be normal • Decrease: • • total protein albumin • Increase: • • serum bilirubin globulin levels • Prothrombin time prolonged – why? Early Signs of cirrhosis: Nausea and vomiting Anorexia Diarrhea or constipation Pain Where? Why? Fever Weight loss • • WHY? How do you know when cirrhosis begins? Later Manifestations: Jaundice Skin Lesions/Spider angiomas Palmer erythema Thrombocytopenia, Leukopenia, Anemia Coagulation disorders Endocrine disturbance Peripheral neuropathy & peripheral edema Jaundice • • • Results from functional derangement of liver cells, compression of bile ducts Liver’s decreased ability to excrete _________ + Biliary obstruction, obstructive jaundice may occur accompanied by pruritus (accumulation of bile salts) Skin Lesions aka:___________ • WHY? • Dilated blood vessels (spider angiomas) • Palmar erythema • What is this? Hematologic Problems Thrombocytopenia Why? Leukopenia Why? Anemia Why? What are some s/s to teach? Vitamin K deficiency Why is this significant? www.elements4health.com Endocrine Problems: Inactivation of adrenocortical hormones Which ones? Men What s/s will you see? Related to what? Women What s/s will you see? Related to what? Hyperaldosteronism Causes what? Peripheral Neuropathy & Peripheral Edema Neuropathies- from what? • Results in mixed nervous symptoms • Sensory symptoms are most common Edema • Caused by what? Complications: Portal Hypertension Esophageal & Gastric Varices Peripheral Edema & Ascites Hepatic Encephalopathy Complications: Portal Hypertension • Compression and destruction of portal & hepatic veins • How much blood carried by portal vein? To where? • Increased venous pressure in portal circulation • Characterized by: • What? • Collateral circulation develops • Why? • o Resulting in: • Varices? • Caput Medusae? What is the most serious complication of portal hypertension? Ascites & Caput medusae Complications: Esophageal & Gastric Varices: o Esophageal: • • complex of twisting veins at lower end of esophagus enlarged & swollen o Gastric: • • upper portion of stomach may occur alone or in combination with esophageal o Tolerate high pressure poorly, bleeding easily with distention o Rupture in response to irritation- factors? o What will we teach? o Most life threatening complication!! Treatment for Varices: o Stop bleeding, manage airway, prevent aspiration of blood!! • How will you prevent aspiration? o Drug Therapy: • Propranolol, Sandostatin, Vasopressin, NTG • How do these work? o Band ligation of varices o Endoscopic sclerotherapy • Thromboses and obliterates distended veins o Balloon tamponade-mechanical compresson of varices • Sengstaken-Blakesmore o Avoid: • alcohol & irritating foods • What common drugs should be avoided? Band Ligation Sclerotherapy: • A sclerosant solution (ethanolamine oleate or sodium tetradecyl sulphate) is injected into the bleeding varix or the overlying submucosa • Complications can include fever, dysphagia and chest pain, ulceration, stricture, and (rarely) perforation. SengstakenBlakesmore Sengstaken-Blakemore Tube Three Lumens: • Esophageal balloon inflation • Gastric balloon inflation • Gastric aspiration • What are some interventions related to this tube? Acute Bleed Supportive Measures: o o o o FFP, PRBC’s, Vitamin K – why? Antibiotics Protonix, Zantac – why? Propanolol • How does it work? o Prevent factors that may increase intra-abdominal pressure!! • Like what? What are some interventions? o Higher incidence of recurrent bleeds, so continued therapy is necessary!! Shunting Procedures: Used more after 2nd major bleeding episode TIPS shunt is placed between systemic and portal venous systems redirect’s portal blood flow reduces portal venous pressure decompresses varices contraindicated in patient’s with hepatic encephalopathy • WHY? TIPS: Transjugular intrahepatic portosystemic shunt Complications: Ascites & Peripheral Edema o Results from impaired liver synthesis of albumin = hypoalbuminemia o Occurs as ankle and presacral edema o Ascites: • • accumulation of serous fluid in periotoneal or abdominal cavity Spontaneous bacterial peritonitis (SBP) o Hyperaldosteronism • Results in what? Four Factors Lead to Ascites Hypoproteinemia Increased Na+ & Increased capillary permeability H2O retention Portal Hypertension Accumulation of high protein fluid in the abdomen Nursing Management of ASCITES: o Assess for respiratory distress • Fowler’s position helps ease work of breathing o Daily weights o Measure abdominal girth o Accurate I&O Medical Management of Ascites: o Na+ and Fluid restriction • How much? o Albumin • Why? o Diuretic therapy: • Aldactone, HCTZ, Lasix • • What is the difference between these? Which do you think would most appropriate? o Paracentesis • • needle puncture of abdominal cavity to remove ascitic fluid- temporary have patient void before procedure o What may be given IV prior to procedure? o Nursing care post procedure? Management of Ascites: o Peritoneovenous Shunt • • • • surgical procedure provides continuous reinfusion of ascitic fluid into venous system Not 1st line in therapy due to high # of complications – such as? Does not improve survival rates Hepatic Encephalopathy: o Terminal complication of liver disease o Disorder of protein metabolism and excretion o Ammonia • • enters the systemic circulation without liver detoxification crosses blood-brain barrier, causing neurologic toxic manifestations o Four stages of manifestations • Review Table 44-12 (page 1077) http://chemistry.about.com Where does ammonia come from? • A by-product of protein metabolism • Protein and amino acids are broken down by bacteria in GI tract, producing ammonia. • Liver converts this to urea which is eliminated in the urine Hepatic Encephalopathy Early Stages 0-1 • • • • • • • • Insomnia Sleep disturbances Short attention span Tremors, incoordination Personality changes Depression Disturbances of awareness Forgetfulness, irritability, & confusion • Trouble writing • Asterixis Hepatic Encephalopathy Stages 2nd & 3rd Lethargy, drowsiness Slow and slurred speech Disorientation Asterixis Impaired judgement Hyperactive reflexes Violent behavior Slow, deep respirations + Babinski reflex Fetor hepaticus – what is this? Hepatic Encephalopathy Stage 4 Impending Coma • + Babinski • Not rousable • May be responsive to painful stimuli • Decerebrate • Possible seizures Treatment: Hepatic Encephalopathy o Reduce ammonia formation • Lactulose • • How does this work? How is it given? o Control GI bleeding – why? o Decreasing protein in intestine o Neomycin • What is this? How does it work? o Electrolyte replacement • Which ones? o Possible liver transplant • depends on a number of factors Hepatorenal Syndrome: o Serious complication o Functional renal failure with advancing azotemia, oliguria, and ascites • what will we see in regards to labs? o Portal hypertension + liver decompensation = decreased arterial blood volume & renal vasoconstriction o May be reversed by liver transplantation Nutritional Therapy: High calorie/High Carb diet Low protein diet – when? Parenteral nutrition of tube feedings may be required Low-sodium diet – when? Dietary education on reading labels at home Overall Goals: Relief of discomfort Minimal to no complications • ascites, varices, hepatic encephalopathy Return to normal as possible lifestyle Liver Dialysis o Bridge to transplant (introduced in 1999) • Utilizes charcoal as detoxifying agent o Dialyze 2-5 days in a row o Dialyze 4- 6 hours at a time Liver Transplantation o Blood type and body size are critical factors in determining who is an appropriate donor. o Potential donors evaluated for: • • • • liver disease, alcohol or drug abuse, cancer, or infection. hepatitis, AIDS, and other infections. matched according to blood type and body size. Age, race, and sex are not considered. o Cadaver vs. live donor livers Donors: • Live donor liver transplants are an excellent option • Liver regenerates to appropriate size for their individual bodies • Survival rates increase / shorter wait time • The donor - a blood relative, spouse, or friend, will have extensive medical and psychological evaluations to ensure the lowest possible risk Liver Transplant complications o Rejection. About 70% of all liver-transplant patients have some degree of organ rejection prior to discharge • Anti-rejection medications are given to ward off the immune attack o Infection • Most infections can be treated successfully as they occur o Cancer http://www.google.com/imgres?imgurl=http://1.bp.blogspot.com/_huyc4ygeN9o/SERUOrRU07I/AAAA AAAAAcI/zwWQfN0Q9jM/s320/x_scar.gif&imgrefurl=http://mrcppreview.blogspot.com/2008/06/scarag ain.html&h=221&w=320&sz=39&tbnid=GpI65e7ofQWymM:&tbnh=90&tbnw=130&zoom=1&usg=__nk4 4z547W0qi8k6hFUZkjF291QI=&docid=5Vu2gOCl3TOdM&hl=en&sa=X&ei=CiIQUdr3O6PE2gXxnoCQDw&ved=0CDUQ9QEwAQ&dur=44 http://www.organdonor.gov/about/transplantationprocess.html Organ Hearts Lungs Livers Kidneys Pancreata Intestine Median national waiting time 113 days 141 days 361 days 1,219 days 260 days 159 days Review Questions: 1. A priority of care for a client having a paracentesis is to? A. Force fluids, instruct patient to keep bladder full prior to procedure B. Instruct patient on how to cough during procedure C. Assist patient into supine position with feet elevated D. Monitor patient’s BP during and after procedure 2. After receiving shift report, which of the following patients would you see first? A. 56 year old with Hepatitis B and D B. 58 year old male, recently diagnosed with hepatic cancer C. Patient with esophageal varices treated with sclerotherapy this AM. D. Patient with splenomegaly, anemia, and PLT count of 60,000 3. A client with cirrhosis is receiving lactulose (Cephulac). During the assessment, the nurse notes increased confusion and asterixis. The nurse should: A. Assess for GI bleeding B. Hold the lactulose (Cephulac) C. Increase protein in the diet D. Monitor serum billirubin levels http://www.murketing.com/journal