aims of the study
advertisement
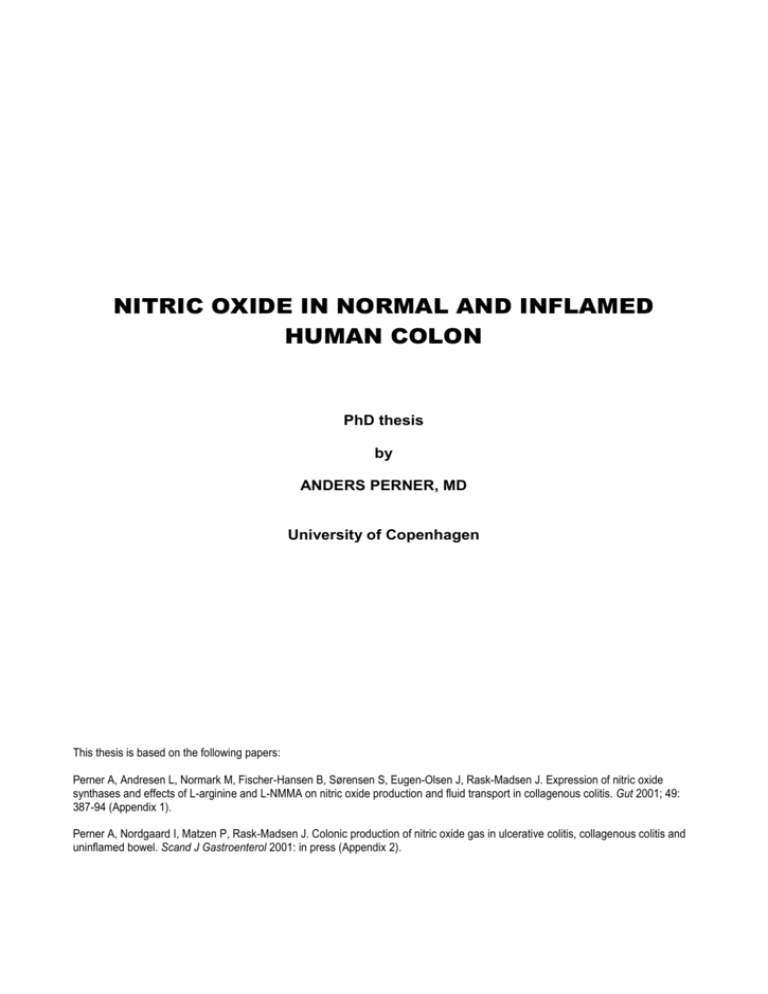
NITRIC OXIDE IN NORMAL AND INFLAMED
HUMAN COLON
PhD thesis
by
ANDERS PERNER, MD
University of Copenhagen
This thesis is based on the following papers:
Perner A, Andresen L, Normark M, Fischer-Hansen B, Sørensen S, Eugen-Olsen J, Rask-Madsen J. Expression of nitric oxide
synthases and effects of L-arginine and L-NMMA on nitric oxide production and fluid transport in collagenous colitis. Gut 2001; 49:
387-94 (Appendix 1).
Perner A, Nordgaard I, Matzen P, Rask-Madsen J. Colonic production of nitric oxide gas in ulcerative colitis, collagenous colitis and
uninflamed bowel. Scand J Gastroenterol 2001: in press (Appendix 2).
CONTENTS
PREFACE .......................................... 2
INTRODUCTION ............................... 3
AIMS OF THE STUDY ....................... 3
RESULTS .......................................... 3
PLASMA CONCENTRATIONS OF NOX............ 3
PERFUSION STUDIES ..................................... 4
Validation of the argon perfusion technique .. 4
Colonic output of NO ..................................... 4
Effects of L-NMMA and L-arginine on colonic
output of NOx and transfer of fluid ................. 4
EXPRESSION STUDIES .................................. 5
Expression of iNOS, eNOS and nNOS in
colonic mucosa .............................................. 5
Localisation of iNOS in colonic mucosa ........ 5
Localisation of nitrotyrosine in colonic
mucosa .......................................................... 5
DISCUSSION..................................... 6
METHODS ........................................................ 6
Participants .................................................... 6
Plasma NOx ................................................... 6
Endoscopy ..................................................... 6
Perfusion studies ........................................... 7
Expression studies ........................................ 8
Statistics ........................................................ 8
RELATED LITERATURE .................................. 8
Chemistry and biological activity of NO ......... 8
Potential physiological roles of NO in the
colon .............................................................. 9
Potential roles of NO in colonic inflammation 9
NO in experimental and human colitis......... 10
CONCLUSIONS AND PERSPECTIVES
....................................................... 10
SUMMARY ...................................... 11
DANISH SUMMARY ........................ 11
REFERENCES ................................. 11
ACKNOWLEDGEMENTS .................. 15
APPENDIX 1 ................................... 16
APPENDIX 2 ................................... 24
PREFACE
This study was carried out at the Department of Gastroenterology, Hvidovre Hospital during the years 1997 and
1998 and at the Department of Gastroenterology, Herlev
Hospital during 1999 and 2000.
I am deeply indebted to Professor Jørgen Rask Madsen.
Continuous engagement, friendship, loyalty and excellent
scientific guidance are the best covering words for his three
and a half years as my tutor.
To Lisa Rohbach, I wish to express my profound gratitude
for skilful secretarial work and assistance in solving any
practical problem.
I also want to express my gratitude to colleagues and
nurses at the above departments for assistance in patient
recruitment and care. Also the laboratory technicians at the
Department of Gastroenterology C-108, Herlev Hospital and
Departments of Clinical physiology, Herlev and Hvidovre
Hospitals are thanked for skilful contribution.
Anders Perner
Copenhagen
NO in normal and inflamed human colon
AIMS OF THE STUDY
The aims of the present study on colonic NO were to
compare plasma values of NOx in subjects with normal
colonic mucosa with those obtained in patients with
collagenous colitis and active ulcerative colitis (I).
determine colonic output of NO in subjects with normal
mucosa and to compare the results with those obtained
in patients with collagenous colitis and active ulcerative
colitis (II).
determine the effects on colonic NOx output and net fluid
transfer of manipulating colonic NOS activity in patients
with collagenous colitis (I).
compare the expression of NOS isoenzymes and
nitrotyrosine in colonic mucosal biopsies from normal
mucosa with that observed in patients with collagenous
colitis and active ulcerative colitis (I).
RESULTS
PLASMA CONCENTRATIONS OF NOx
Concentrations of NOx in plasma were three-fold higher
(p<0.001; Fig 1) in patients with collagenous or ulcerative
colitis than in patients with uninflamed colonic mucosa (I).
200
*
100
*
lit
co
iv
e
at
er
lc
U
C
ol
la
nf
ge
la
no
m
us
ed
co
l
on
co
lit
is
is
0
ni
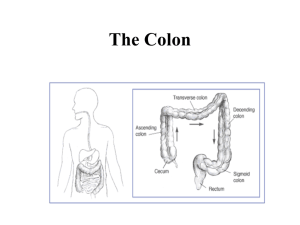
Nitric oxide (NO) is involved in the physiology and
pathophysiology of virtually all organ systems including the
gut.1 The physiological actions of NO are mainly mediated by
activation of the soluble guanylate cyclase,2 whereas the
reaction with metals and other free radicals is considered to
be prevalent in pathophysiological conditions.3
NO is generated by the enzyme, NO synthase (NOS),
which has three distinct isoforms: two constitutively
expressed forms (commonly designated cNOS) and an
inducible form (iNOS or NOS II). All isoforms require the
amino acid, L-arginine, and oxygen as substrates, in addition
to a variety of co-factors.4 NO metabolism is complex due to
its many potential reaction pathways, most of which yield
nitrite and nitrate (NOx).5,6
cNOS exists as neuronal (nNOS or NOS I) and endothelial
(eNOS or NOS III) NOS isoforms, which show considerable
structural similarities. While their names reflect the cell types
in which they were originally identified, these enzymes have
now been localised in a large number of cell types and
tissues and they are continuously expressed in the gut by
submucosal neuronal cell bodies present in the myenteric
plexus and in vascular endothelial cells. Physiologically,
cNOS generates low concentrations of NO, which may serve
as a nonadrenergic noncholinergic neurotransmitter and as a
vasodilator.1,7 While it is unknown whether nNOS is
expressed in colonic mucosa, eNOS has been demonstrated
in endothelial and epithelial cells.8 In the normal epithelium,
NO may modulate colonic ion transport and serve in host
defence.9,10
Expression of iNOS is induced in inflammatory cells and
enterocytes by various microorganisms, lipopolysaccharides
and proinflammatory cytokines, such as interleukin-1,
interferon- and tumour necrosis factor-.11 Production of
NO by iNOS has been considered a pathway of mucosal
damage in the intestine due to proposed cytotoxic effects of
NO,12,13 but the in vivo reactivity and toxicity of NO was
recently questioned.3 Moreover, the results of
pharmacological inhibition14,15 or genetic ablation16,17 of iNOS
in experimental colitis have provided conflicting data.
Studies in patients with active ulcerative colitis have
demonstrated raised concentrations of nitrite in rectal
dialysates,18 high levels of the co-product of NO, citrulline, in
rectal biopsies,19 increased activities of NO synthase in
colonic biopsies,20 and elevated levels of NO in gas aspirated
from the colonic lumen.21 The occurrence of excess
production of NO in colonic inflammation has been confirmed
by use of laser spectroscopy in rectal perfusion studies and
an NO-selective microelectrode for intramucosal
measurements.22,23 Upregulation of iNOS in the inflamed
epithelium appears to be the cause of enhanced generation
of NO in patients with ulcerative colitis.24 Moreover, iNOS
may be expressed in association with nitrotyrosine,24 which is
the stable end-product of the reaction between tyrosinecontaining proteins and reactive nitrogen species, such as
peroxynitrite, nitrous acid, nitryl chloride, and the nitrogen
dioxide radical.25 The demonstration of nitrotyrosineassociated iNOS activity supports the hypothesis that
reactive nitrogen species, rather than NO per se, may be
responsible for iNOS-mediated cellular injury.3
3
Collagenous colitis is a rare form of idiopathic colitis
characterised by chronic watery diarrhoea and microscopic
inflammation,26 whereas destructive inflammation never
occurs. Although the mediators responsible for secretion
remain undefined, a recent study in collagenous colitis
suggests that colonic NO is produced in excess.27
As NO donors induce secretion of fluid and electrolytes in
the uninflamed human colon,28 increased production of NO
may contribute to diarrhoea in colonic inflammation. On the
other hand, nitrotyrosine-associated NOS activity, but not NO
in itself, may add to mucosal damage.
NOx (µmol/l)
INTRODUCTION
U
A Perner, PhD thesis
Figure 1. Plasma concentrations of nitrite/nitrate (NOx) in patients with
uninflamed bowel, collagenous colitis or active ulcerative colitis. Plasma
was sampled after an overnight fast and concentrations of NOx were
measured by the Griess assay after conversion of nitrate to nitrite by
nitrate reductase. The y-axis denotes concentrations and individual values
are represented by dots and group means are given as horizontal lines.
*p<0.001 compared with patients with uninflamed colonic mucosa (Mann
Whitney U test).
NO in normal and inflamed human colon
PERFUSION STUDIES
Validation of the argon perfusion technique
During constant infusion of argon (50 ml/min) into the
caecum, stable concentrations of argon in samples of
perfusate collected at the rectum were reached after a 50minute equilibration period (Fig 2). 'Steady state' conditions
were defined to be from 50 to 70 minutes where
concentrations of argon were nearly constant (coefficient of
variation 5%, n=5) (II).
Argon infused into the caecum from 0 to 90 minutes was
almost completely recovered in gas collected from the rectum
(96 2%, mean SEM; n=5) (II).
In other validation experiments using decreasing rates of
perfusion (75, 50 and 25 ml/min) colonic output of NO was
nearly constant and thus independent of the perfusion rate
(coefficient of variation 21%; n=6) (II).
4
ulcerative colitis the output of NO was positively correlated to
the severity of disease as judged by a total inflammation
score (n=11, r=0.77, p<0.01).
A
10000
Nitric oxide (ppb)
A Perner, PhD thesis
1000
100
80
10
60
10
20
30
40
50
60
70
80
10
20
30
40
50
60
70
80
B
10000
40
20
0
10
20
30
40
50
60
70
80
90
Minutes
Figure 2. Rectal concentrations of argon during perfusion of whole colon.
Argon was infused into the caecum (50 ml/min) and the volume-% of argon
in gas sampled from the rectum was measured by neutron activation
analysis (mean SEM; n=5).
Colonic output of NO
The mean concentration of NO at 'steady state' was 28 5
ppb ( SEM) in twenty patients with uninflamed colonic
mucosa (Fig 3). This equals a calculated NO output of 0.07
0.01 nmol/min from the colon (II).
In patients with active collagenous colitis, colonic output of
NO was 50-fold higher than in subjects with uninflamed
colonic mucosa (3.4 0.6 vs 0.07 0.01 nmol/min,
p<0.001). At endoscopy, the mucosa was essentially normal,
but a remarkable dilation of submucosal vessels was
observed in all patients with active collagenous colitis (II).
In four patients with inactive collagenous colitis (i.e.
absence of diarrhoea at the time of investigation) the colonic
output of NO was significantly lower than in active disease
(0.4 0.1 vs 3.4 0.6 nmol/min; p=0.01), but still five-fold
higher than in subjects with uninflamed mucosa (p<0.01).
In patients with active ulcerative colitis, colonic output of
NO was ten-fold higher than in uninflamed bowel (0.7 0.2
vs 0.07 0.01 nmol/min, p<0.001), but significantly lower
than observed in patients with active collagenous colitis
(p<0.01). Even in patients with severe ulcerative pancolitis,
outputs of NO were below the mean value observed in active
collagenous colitis. Within the group of patients with
Nitric oxide (ppb)
Ar conc. (volume %)
100
1000
100
10
Minutes
Figure 3. Concentrations of nitric oxide in perfusates sampled from the
rectum during perfusion of whole colon with argon in patients with
uninflamed bowel, collagenous colitis or active ulcerative colitis. The
logarithmic y-axes denote concentrations in parts per billion (ppb) and
individual values are represented by dots: A. active collagenous colitis ()
or inactive collagenous colitis (O) and B. active ulcerative pancolitis or leftsided colitis () or distal ulcerative colitis (O). Patients with uninflamed colon
(◊, means SEM, n=20).
Effects of L-NMMA and L-arginine on colonic output of
NOx and transfer of fluid
In patients with uninflamed bowel, concentrations of NOx in
the perfusates were below the detection limit. Fluid was
absorbed and net transfer rates of fluid were unaffected by
the duration of perfusion in time-control experiments (-2.1
0.2 vs -2.1 0.2 ml/min, mean SEM; p=0.89).
In patients with collagenous colitis, the colonic output of
NOx was markedly higher than in patients with uninflamed
bowel (283 58 vs <37 nmol/min, p<0.01) and fluid was net
A Perner, PhD thesis
NO in normal and inflamed human colon
secreted into the colonic lumen (+0.7 0.2 vs -2.1 0.2
ml/min, p<0.001). L-NMMA reduced the output of NOx by 13
– 66 % (95% confidence interval) and net secretion of fluid by
25-109%, while L-arginine caused a 3 – 39% increase in the
output of NOx and a 15 – 93% increase in net secretion of
fluid (Fig 4).
NOx (nmol/min)
A
500
5
mucosa, but intense staining was observed only at the
luminal border (Fig 6). Less intense staining was observed in
some of the inflammatory cells in lamina propria.
In biopsy specimens from all patients with ulcerative colitis,
iNOS was localised within the epithelial cells. In general,
labelling was less intense in crypt cells, while the
inflammatory cells in the lamina propria produced only little
staining. In areas with less intense epithelial staining, this
was localised predominantly in the apical cytoplasm (Fig 6).
400
300
200
iNOS
100
0
GAPDH
1.5
1000
1.0
0.5
100
0.0
-0.5
Basal
L-NMMA
Basal
L-arginine
Figure 4. Effects of topical L-NMMA or L-arginine on colonic output of NOx
and transfer rates of fluid in patients with collagenous colitis during perfusion
of whole colon. After obtaining 'steady state' conditions, L-NMMA () or Larginine (O) was infused into the caecum and effects on NOx output and net
fluid transfer were observed after re-establishment of 'steady state'. Two
independent experiments were performed in each patient, but one patient
refused to participate in the second perfusion (L-arginine). Each line
represents data from a single patient. A. Colonic output of NOx during
perfusion of whole colon. B. Colonic net transfer of fluid during perfusion of
whole colon. Positive values represent net secretion and negative values net
absorption.
Optical density
Net fluid transfer (ml/min)
B
*
*
10
1
0.1
0.01
EXPRESSION STUDIES
Expression of iNOS, eNOS and nNOS in colonic mucosa
iNOS was detected in mucosal cell lysates from all subjects
by Western blot analysis (Fig 5). The values of banddensities were 102 - 103 higher (p<0.001) in the groups of
patients with collagenous colitis and ulcerative colitis than in
the group of patients with uninflamed colonic mucosa. There
were no statistically significant differences (p=0.27) in band
densities between the two groups of colitis patients (Fig 5).
eNOS was also detected in all samples, but there were no
differences in optical densities of the eNOS bands between
patients with uninflamed bowel and patients with collagenous
or ulcerative colitis (p=0.56 and p=0.91, respectively).
In contrast, nNOS was not detected in any subjects.
Localisation of iNOS in colonic mucosa
iNOS was observed in the crypt epithelium in six of ten
patients with uninflamed colon by immunohistochemistry
(Fig 6).
In biopsy specimens from all patients with collagenous
colitis, iNOS was localised in the epithelial cells of the colonic
Figure 5. Expression of iNOS in mucosal biopsies from patients with
uninflamed bowel, collagenous colitis or active ulcerative colitis. Expression
was analysed by Western blotting and quantified by densitometry relative to
a reference, which was defined as 1.0. For internal control of loading, the
samples were also blotted against an anti-GAPDH antibody. The logarithmic
y-axis denotes optical densities and individual values are represented by
dots and group means by horizontal lines. *p<0.001 compared with
uninflamed colon (t-test).
Localisation of nitrotyrosine in colonic mucosa
Nitrotyrosine was not observed in biopsies from patients with
uninflamed colonic mucosa and labelled only slightly in the
epithelium of a single patient with collagenous colitis. Intense
epithelial staining was observed in all biopsies from patients
with active ulcerative colitis (p<0.01; see Fig 7) and was
associated with the presence of neutrophils in the epithelium.
In areas of the epithelium with less intense staining,
neutrophils were fewer or absent. Nitrotyrosine was also
detected in clusters of mononuclear cells from three patients
with collagenous colitis and in lamina propria inflammatory
cells, which were predominantly neutrophils, in six of the nine
patients with ulcerative colitis, see Fig 7.
A Perner, PhD thesis
NO in normal and inflamed human colon
A
B
DISCUSSION
METHODS
Participants
For the study of NO in normal colonic mucosa, patients
referred to endoscopy to exclude colorectal cancer were
included. All had symptoms of irritable bowel syndrome or
haematochaezia, and all had a normal colonoscopy (I & II)
and an uninflamed mucosa at histopathological examination
(I). Moreover, there was a low variability of the results
obtained in spite of differences in the tentative clinical
diagnosis and variations in age and sex. It cannot be
excluded, however, that the results obtained in 'normal' colon
in the present studies were a result of functional changes
without detectable pathology in the patient-controls included.
Thus it has been assumed that iNOS is only expressed in
pathological conditions, but iNOS was detected in 'normal'
mucosa in the present study (I). On the other hand,
preliminary data show that iNOS is expressed also in the
colonic epithelium in healthy subjects (data not shown).
Plasma NOx
NO metabolism and dietary NOx are the only known sources
of NOx in vivo. Thus, an NOx-low diet for 48 hours is ideal for
evaluation of endogenous NO production.29 In the present
study (I), samples for determination of plasma NOx were
taken after an overnight fast, as it was not feasible to
postpone treatment of patients with active ulcerative colitis
for two days to allow optimum preparation. It is unlikely,
however, that dietary NOx has influenced the marked
6
C
Figure 6. Localisation of iNOS in mucosal biopsies from the human
colon analysed by immunohistochemistry and counterstained with
haematoxylin. A. Uninflamed mucosa stained with an iNOS IgG
antibody. No reaction is observed. B. Biopsy section from a
collagenous colitis patient showing a thickened collagenous band
beneath the epithelium (open arrow). The reaction product (red) of the
iNOS antibody is localised at the luminal border of epithelial cells (see
arrows at surface and crypts) and to a minor degree in mononuclear
cells of the lamina propria (arrowhead). C. Biopsy section from a
patient with severe ulcerative colitis at endoscopy showing disturbed
mucosal architecture and pronounced infiltration of inflammatory cells.
The reaction product of the iNOS antibody is localised primarily in the
surface epithelial cells (arrow). A discrete reaction is observed in
adjacent neutrophils and in mononuclear cells of the lamina propria. In
areas with less intense reaction, this is primarily localised in the apical
cytoplasm (arrowheads).
differences observed between the two groups of patients with
colitis and the group of controls. Moreover, plasma levels of
NOx in patients with collagenous colitis and controls, who had
been on an NOx-low diet,27 were comparable to the those
observed in the present study.
The method for determination of NOx has been evaluated
previously.30 The impression of a valid method was
confirmed in the present study by the finding of a low
detection limit and minimal interassay variation.
The colonic mucosa is the most likely source of raised
plasma concentrations of NOx in patients with colitis, who
were all free of manifestations of extraintestinal disease. In
patients with collagenous colitis, which may be associated
with celiac disease,31 normal histology of the small intestine
was ensured prior to study.
Endoscopy
All participants were studied following routine endoscopy,
which was preceded by colonic preparation with docusate
sodium and sorbitol or bisacodyl and polyethylene glycol.
The colonic preparation may have confounded the results,
as bisacodyl have been shown to act, at least in part, through
promotion of NO synthesis.32 It is unlikely, however, that
bisacodyl-induced NO or iNOS have contributed significantly
to the results obtained in colitis, as extremely low values
were observed in the normal colon. Furthermore, preliminary
results obtained in healthy subjects suggest that iNOS is
expressed in colonic epithelium also in unprepared bowel
(data not presented).
A Perner, PhD thesis
NO in normal and inflamed human colon
A
B
Perfusion studies
The technique of 'steady state' perfusion was used because
it allows quantification of NO output from whole colon in
vivo.33
The intubation of the caecum during colonoscopy was
more convenient than the tedious oral intubation previously
used.34 The position of the tube was checked fluoroscopically
before and after perfusion and the tip of the tube shown to be
anchored safely in the caecum in all experiments.
The perfusion of a prepared colon minimises potential
confounding by luminal bacteria, which may metabolise NO
and NOx,35 and the low output from the normal bowel makes
it unlikely that bacteria contribute significantly to the high
values observed in patients with colitis.
Argon perfusion. Gas perfusion was applied to allow direct
measurements of colonic output of NO. The technique has
previously been used to estimate intestinal production of N2,
CO2, H2 and CH4.36 Argon was used as a non-absorbable
marker to avoid interference with the analysis of NO.
Interestingly, a resent study reported the generation of a
stable argon compound (HArF),37 making reservations
necessary in the traditional view of argon as a noble gas.
The present findings of high recovery of infused argon and
flow-dependent 'steady state' concentrations of NO justify the
use of argon as a non-absorbable marker in perfusion
studies, even though the accuracy of the perfusion method
cannot be assessed directly. However, colonic output of NOx
was 60-fold higher than that of NO gas in comparable
patients (I, II). The difference may in part be explained by
back-diffusion and/or by the reaction of NO with mucosal or
7
C
Figure 7. Localisation of nitrotyrosine in mucosal biopsies from
human colon analysed by immunohistochemistry and
counterstained with haematoxylin. A. Uninflamed mucosa stained
with a nitrotyrosine antibody. No reaction is observed. B. Biopsy
section from a patient with collagenous colitis. The reaction
product (red) of the nitrotyrosine antibody is observed within
mononuclear cells of the lamina propria (arrowheads). C. Biopsy
section from a patient with ulcerative colitis showing disturbed
mucosal architecture and pronounced infiltration of inflammatory
cells. The reaction product of the nitrotyrosine antibody is
localised in the epithelium (arrows) in association with neutrophils
and in lamina propria inflammatory cells (arrowheads).
luminal components resulting in the formation of NOx.5,6 On
the other hand, the observed association between colonic
output of NO gas and indices of clinical disease activity in
ulcerative colitis and collagenous colitis (II) shows that NO
output is a sensitive marker of mucosal NO synthesis. It
remains to be established, however, which of the two
methods is the better estimate of mucosal NO synthesis.
Fluid perfusion. The single lumen technique used for
perfusion in the present study (I) does not allow aspiration of
ileal secretions for correction of colonic flow rates. On the
other hand, the ileocaecal valve is left intact and ileal
secretions (below 1 ml/min)38 and perfusate back-flow (0.5
ml/min)33 is negligible compared to the perfusion rate applied
(15 ml/min). Moreover, the paired study design minimises
potential systematic errors.
The colonic mucosa is the most likely source of enhanced
output of NOx in collagenous colitis. The use of perfusion
technique controls for confounding factors, such as NOx of
dietary or bacterial origin. Moreover, the observed responses
to topical L-NMMA and L-arginine indicate that luminal NOx
acts as a marker of mucosal NO synthesis.
The intervention with L-NMMA and L-arginine was designed
to ensure concentrations in the colonic mucosa sufficiently
high to cause sustained modulation of NOS activity during
the experimental period, as it has previously been done in
comparable animal studies exploring the role of NO in
intestinal fluid and electrolyte transfer using parenteral or
luminal arginine analogues.9,39 The initial concentration of LNMMA was far greater, therefore, than the ID50 for NOS
(100 mM vs 7-10 µM)40 to ensure that all colonic segments
A Perner, PhD thesis
NO in normal and inflamed human colon
were exposed to concentrations greater than ID50, at least
during part of the equilibration period, in spite of immediate
dilution of L-NMMA (approx. 300 ml in the perfused colon)33
and further dilution by the volume of test solution infused
during equilibration. Nevertheless, concentrations of the nonabsorbable marker (Cr51-EDTA) and NOx were constant in
perfusates collected at the rectum during the experimental
period. Moreover, the observed opposite effects of L-NMMA
and L-arginine indicate that these occurred through
modulation of NOS.
As L-NMMA is considered to have little selectivity for the
various NOS isoforms,41 the relative contribution of cNOS
and iNOS to the observed output of NOx cannot be defined.
With reference to the abundance of iNOS in collagenous
colitis it seems unlikely, however, that cNOS contributes
significantly to the enhanced generation of NO.
Expression studies
To identify the source of NO in normal and inflamed colon
expression studies were performed (I). Protein expression of
NOS isoforms was preferred over mRNA as iNOS in
particular is subjected to posttranscriptional regulation.42
The immunochemical methods applied in the present study
rely on the quality of the antibodies used, which is why
appropriate control experiments were performed (I). The
iNOS antibody used has previously been validated.24
Unspecific reactions, observed in preliminary experiments of
the present study (I), were avoided through IgG purification of
the original serum batch. Also the nitrotyrosine antibody has
previously been validated,24 and appropriate control
experiments in the present study (I) confirm a highly specific
reaction. For the eNOS and nNOS antibodies, the
immunogens were not available, so blocking experiments
could not be performed. It is unlikely, however, that the
observed reaction products were unspecific as single bands
of correct molecular weight were observed in the Western
blot analysis of patient samples and control lysates supplied
by the manufacturer. For the nNOS antibody, reaction
against human nNOS was confirmed using lysates from a
biopsy of human cerebellum, which express nNOS.43
Clearly, detection of NOS protein does not imply enzyme
activity, but a valid quantitative method to differentiate NOS
activity does not exist. A widely used method is to assess
Ca2+-dependent (cNOS) and -independent (iNOS) NOS
activities in vitro by measuring formation of the co-product of
NO, citrulline, in tissue-lysates. However, the assay
measures maximal synthase capacity, as substrates and cofactors are added in excess. Another criticism against this
assay is that Ca2+-independent NO synthesis has been
shown by cNOS,44 why Ca2+-independent generation of
citrulline cannot be considered a specific marker of iNOS
activity.
Taken together, the above results indicate that iNOS
activity is upregulated in the colonic epithelium of ulcerative
and collagenous colitis, but this has to be confirmed by
results of the application of iNOS-selective pharmacologic or
genetic tools in vivo.
Nitrotyrosine is presently considered a marker of reactive
nitrogen species,25 such as peroxynitrite, nitrous acid, nitryl
chloride, and the nitrogen dioxide radical. The named
compounds may depend on NO produced by iNOS, because
8
the induction of colitis in iNOS-deficient mice caused no rise
in the expression of nitrotyrosine, as it was observed in their
wildtype littermates.17 Therefore, nitrotyrosine may be a
marker of iNOS-mediated tissue injury.
Statistics
In the present study, results were analysed by parametric
methods, which implies that the data are sampled from a
population with 'normal' or Gaussian distribution. For
unpaired variables, an equal variance in the test groups is
required for proper use of parametric methods.
To ensure that the above assumptions were fulfilled, the
data were analysed for normality (Kolmogorow-Smirnov test)
and equal variance (Levine test) prior to the parametric
analysis test.45 Although sample numbers were small, the
assumptions of normality or equal variance were met except
for NO output, eNOS density, and plasma NOx. For these
end points, a non-parametric test, which makes no
assumptions about distribution or variance, was performed to
corroborate the parametric analysis test.
RELATED LITERATURE
Chemistry and biological activity of NO
NO has an unpaired electron in the outer shell and is thus by
definition a free radical, which is why NO generally has been
considered highly reactive. NO is both water and lipid
soluble,2 and in physiological models the molecule travels
freely through cells and most tissues, only limited by its rate
of diffusion and its degradation in the presence of
oxyhaemoglobin.3 These observations support the notion that
NO has high reactivity only against other free radicals and
transitional metals,3 including heme of guanylate cyclase and
haemoglobin, through which NO mediates many biological
actions and its own degradation.1
The reaction of NO with other free radicals, such as
reactive oxygen species, may result in the formation of
reactive nitrogen species, including peroxynitrite, nitrous
acid, nitryl chloride, and the nitrogen dioxide radical. The
finding of nitrotyrosine in the colonic mucosa suggests that
the reaction occurs in vivo (I),24,46 and may explain the lower
colonic output of NO in ulcerative colitis than in collagenous
colitis, as observed in the present study (II).
The most studied reactive nitrogen species is peroxynitrite,
which is formed by the kinetically favoured reaction of NO
with the superoxide anion. At physiologic pH, peroxynitrite
will be protonated to yield peroxynitrous acid and then rapidly
decay to form the nitrogen dioxide and hydroxyl radicals,
both of which are potent oxidising agents.47 Hence
peroxynitrite can induce both nitrosative and oxidative stress
(i.e. an imbalance between the formation and scavenging of
reactive nitrogen or oxygen species, respectively)48 through
lipid peroxidation,49 breaking of DNA strands,50 depletion of
intracellular ATP stores,50 and nitration of tyrosine residues.51
In addition to being a marker of nitrosative stress, nitration of
tyrosine may lead to protein dysfunctioning as shown for
cytoskeleton proteins in epithelial cells,52,53 and superoxide
dismutase obtained in biopsy specimens from inflamed
human kidney.54 The latter reaction may contribute to a
vicious circle, where reduced dismutation of superoxide
results in increased formation of peroxynitrite.54
A Perner, PhD thesis
NO in normal and inflamed human colon
NO's potential interaction with molecular oxygen has linked
chronic inflammation to neoplasia via the formation of
carcinogenic nitrosamines.55 On the other hand, collagenous
colitis was not observed to be associated with an increased
risk of colorectal cancer in a recent study,56 but the mean
follow-up of the cases included was limited to seven years. It
may be speculated that the anaerobic environment in the
colon minimises the generation of nitrosamines in spite of
high levels of NO. Alternatively, carcinogenesis induced by
NO may be mediated through reactive nitrogen species,
which may induce DNA damage, at least in cultured intestinal
epithelial cell.50
Potential physiological roles of NO in the colon
There are several studies on the functional role of NO in the
large bowel, most of which were performed in rodents using
pharmacologic or genetic manipulation of NO bioavailability.
The present study confirms that NO is produced by normal
human colon (II),21,57 where it has been proposed to
contribute to the regulation of transepithelial transport,
motility, microcirculation, barrier functioning and host
defence.58 The critical role of NO in normal bowel function is
illustrated by the effects of NOS inhibition, which mimics
several features of acute inflammation, including enhanced
recruitment of neutrophils,59 mast cell degranulation,60 and
increased vascular and epithelial permeability.61,62
The present study demonstrates that iNOS is expressed in
the epithelium of normal human colon. This finding is
inconsistent with the general view that iNOS is induced only
in pathophysiological conditions. On the other hand, it agrees
with results obtained in normal epithelium of human airway
and mice colon,63,64 where iNOS is constitutively expressed,
suggesting that epithelial iNOS and NO contribute to the
unspecific host defence. This concept is further supported by
the observation that NO has direct anti-microbial activity,10
and that enteroinvasive bacteria directly upregulate iNOS in
the apical cytoplasm in monolayers of colonic epithelial
cells.65 Moreover, normal colonic epithelium also releases
superoxide,66 and the interaction between the two may
produce nitrosative and oxidative stress in invading
microorganisms,67 although this has yet to be demonstrated
in vivo.
In addition to the contribution to the chemical barrier of the
colon, NO may stimulate secretion of mucus via guanylate
cyclase as observed in gastric mucosal cells of rats.68
Potential roles of NO in colonic inflammation
Experimental and clinical evidence suggests that colonic
inflammation is associated with a hyperdynamic circulation of
the large bowel.69,70 However, the mechanisms responsible
for the inflammation-induced hyperaemia remain speculative.
Enhanced production of NO by the inflamed mucosa may
result in inflammation-induced hyperaemia,1 seen as marked
submucosal vasodilation in collagenous colitis (II).
Secretion or reduced absorption of fluid and electrolytes
across the epithelium is another hallmark of colonic
inflammation, which may be mediated by NO. Experiments in
rodents have often shown that NO donors act as secretory
agents to promote net secretion of fluid and electrolytes into
the colonic lumen. Thus, inhibitors of NOS are proabsorptive
9
when used in established colonic secretion induced by
various secretagogues9 or by inflammatory mediators, such
as interleukin-1 and lipopolysaccharides.71,72 This agrees
with observations made in Ussing chamber studies of
uninflamed human colon using NO donors,28 and in the
present perfusion studies in collagenous colitis by use of
pharmacological manipulation of NOS (I). Therefore, it is
reasonable to believe that NO acts as a secretagogue in
colonic inflammation. Whether fluid secretion and diarrhoea
protects the mucosa against bacteria and toxic compounds of
inflammation remains, however, speculative.
NO-mediated relaxation of the gut is facilitated by its
peripheral action as the primary nonadrenergic
noncholinergic transmitter.7 Enhanced generation of NO may
also contribute to the development of toxic megacolon, where
acute hypotonic dilation of the colon is associated with
increased activity of NOS both in the mucosa and the
muscularis propria.73
Active inflammation of the colonic mucosa is associated
with increased production of cytokines, such as tumour
necrosis factor-, interleukin-1 and interferon-, all of which
are capable of inducing iNOS in enterocytes and endothelial
cells.1,11 Thus, the induction of iNOS in intestinal epithelial
cells may represent a pathway for mucosa damage.12 The
results of the present study suggest, however, that injury
associated with excess production of NO only occurs when
conditions for nitrotyrosine formation are present. In
agreement with this, colonic mucosa from patients with
ulcerative colitis has been shown to generate reactive
oxygen species in excess.74 Because the reaction between
NO and superoxide is kinetically favoured over the
decomposition of superoxide by superoxide dismutase,3
ulcerative colitis might create favourable conditions for the
formation of peroxynitrite. The process may be further
enhanced by simultaneous suppression of superoxide
dismutase activity, as observed in experimental colitis.75
In the present study (I), nitration of tyrosines was
associated with the presence of neutrophils. Infiltrating
phagocytes may, therefore, contribute to the formation of
reactive nitrogen species in the colonic mucosa through
release of NADPH oxidase-mediated superoxide or directly
via a myeloperoxidase-dependent pathway.25 Also, a NADPH
oxidase of epithelial cells may contribute to oxidative stress
in gut mucosa, as suggested by lipopolysaccharide-mediated
upregulation of superoxide output from gastric pits cells.76
It is generally assumed that peroxynitrite is formed when
NO reacts with exogenous superoxide, but a recent study
suggests that iNOS only elicits cytotoxicity when limited Larginine availability causes the formation of superoxide and
peroxynitrite by iNOS.77 The hypothesis implies that Larginine as well as inhibitors of iNOS may be protective by
reducing the formation of peroxynitrite in states of L-arginine
depletion. Supplementation of L-arginine may further reduce
oxidative stress through the non-enzymatic conversion of
hydrogen peroxide to NO.78
Following inflammation, healing of colonic mucosa may
involve NO in activated mucosal myofibroblasts through
increased synthesis of collagen.79 This notion is supported by
the effective treatment of NSAID-induced gastric ulcers with
NO donors,80 but accelerated healing by NO has yet to be
demonstrated in the colonic mucosa. It is noteworthy that the
A Perner, PhD thesis
NO in normal and inflamed human colon
collagen band, which denotes collagenous colitis, is formed
from activated myofibroblasts located close to the NO
producing epithelium.81
NO in experimental and human colitis
Experimental colitis. Chemical induction of experimental
colitis in rodents results in enhanced colonic generation of
NO.75,82 Also in spontaneous colitis of rhesus monkeys, NOS
activity is increased in the inflamed mucosa.15 In these
models, iNOS is upregulated mainly in the inflammatory cells
infiltrating the colonic mucosa,15,64 which is in contrast to
human colitis where iNOS is expressed primary in the
epithelial cells (I). Moreover, the circumstances required for
release of NO from human inflammatory cells remain
controversial,83 because iNOS in macrophages displays
hyporesponsiveness to bacterial lipopolysaccharides both
with and without co-stimulation by interferon-.84 The above
models may, therefore, have low predictiveness for the role
of NO in human colitis.
Exceptions to the above are spontaneous colitis in
interleukin-10 deficient mice and lethal colitis in mice induced
by trinitrobenzene sulphonic acid, where iNOS is highly
expressed in the colonic epithelium.17,85 It remains to be
established, however, whether these models have a better
predictive value for human colitis.
Conflicting data about the therapeutic properties of NOS
inhibitors and L-arginine in experimental colitis may, at least
in part, be explained by differences in experimental design,
the specificity of the compound applied, timing of the
experiment, choice of dose, and route of administration.82,86-90
Still, a majority of these studies have shown a beneficial
effect of NOS inhibition, whereas the few studies on Larginine supplementation have provided conflicting results.8991 Theoretically, selective inhibitors of iNOS offer the
advantage of leaving the physiological output of NO from
cNOS unaffected, but their use in experimental colitis have
not yet settled the controversy.14,15 While the enhanced antiinflammatory effects of an NO-releasing derivative of
mesalamine suggest a protective role of NO in experimental
colitis,92 conflicting results obtained in iNOS deficient mice
emphasise the need for human studies.16,17,64,85
Human colitis. The present and numerous other studies
show that output of NO is enhanced in human colitis,
including ulcerative,21-23,93,94 collagenous,27 and infectious
colitis.57 The common finding of high expression of iNOS in
the colonic mucosa makes it likely that this isoform induces
NO in colitis (I),24,46,95-98 but direct evidence is lacking. Raised
activity of a calcium-independent NOS has been observed in
the colonic mucosa from patients with active ulcerative
colitis,20,95,99 but as mentioned above, this does not
differentiates iNOS and eNOS activity.44
There are only few studies on cNOS expression in human
colitis, but it has been observed repeatedly that eNOS is
expressed at equal levels in mucosal biopsies from
uninflamed colon and ulcerative colitis (I),96,100 whereas
nNOS is undetectable (I).100 Therefore, it seems unlikely that
cNOS contributes significantly to enhanced generation of NO
in human colitis.
In ulcerative colitis, there is convincing evidence that iNOS
is expressed predominantly in the inflamed colonic epithelium
and only to a lesser extent in adjacent inflammatory cells
10
(I),24,46,95-98 Also in patients with collagenous colitis, iNOS was
observed in the epithelium (I). The findings of intense
expression at the luminal border in collagenous (I) and
ulcerative colitis (I),97 suggest that iNOS is upregulated in
response to a luminal insult. This impression is substantiated
by the observations of iNOS expression in the epithelium
also in Shigella and Salmonella colitis.98,101
In addition to bacteria, colonic output of NO may be
enhanced by bile acids, as shown in perfusion studies of
intact sigmoid colon.102 But several more luminal compounds
may act alone or in combination to induce iNOS, so no
hypothesis can be made about the contribution of specific
luminal agents to the pathogenesis of the above forms of
idiopathic colitis.
The induction of iNOS shares the transcriptional pathway
with a variety of proinflammatory mediators through the
activation of nuclear factor-B (NF-B).42 In active ulcerative
colitis, NF-B appears to be activated in the inflamed
epithelium,103 and iNOS seems to be co-expressed in the
colonic mucosa with NF-B-dependent mediators.104 It is
currently unknown whether NF-B activity is upregulated
also in collagenous colitis, but if this is the case, the
expectations from inhibitors of NF-B as a potential
therapeutic option in ulcerative colitis may be dampened.105
NO-associated mucosal damage may occur through the
formation of reactive nitrogen species, as suggested by
marked expression of nitrotyrosine only in patients with
ulcerative colitis (I).24 In support of this, iNOS and
nitrotyrosine were also co-expressed in the epithelium in
infants with necrotizing enterocolitis.106 As nitration of
tyrosine was associated with infiltration of neutrophils in the
present study, the observed differences between ulcerative
and collagenous colitis may reflect different degrees of
neutrophil infiltration, which is rarely seen in the colonic
mucosa in patients with collagenous colitis.107 Moreover, the
observations add to the hypothesis that neutrophils have a
central role in the development of mucosal injury in patients
with ulcerative colitis.108
CONCLUSIONS AND PERSPECTIVES
Several steps in the biosynthesis of NO are responsive to
manipulation and several compounds act in vivo by
generating NO, such as glyceryl trinitrate and sodium
nitroprusside. Furthermore, modulation of the supply of NOS
co-factors may change the formation of NO, and direct
manipulation of the guanylate cyclase may modulate effects
of NO.41
A rationale for safe manipulation of NO bioavailability in
chronic inflammatory bowel disorders has not yet been
defined. Administration of L-arginine or its analogues seem to
influence the output of NO by colonic mucosa and may prove
to be a valuable tool for studying the pathophysiological roles
of NO in patients with inflammatory bowel disorders.
In ulcerative colitis, there is evidence to suggest that
reactive nitrogen species, rather than NO per se, contribute
to mucosal injury. Any therapeutic intervention against iNOS
may, however, be anticipated to reduce nitrotyrosineassociated damage at the expense of decreased blood flow,1
impaired anti-microbial defence,10 and increased recruitment
of neutrophils.59 In contrast, supplementation of antioxidant
A Perner, PhD thesis
NO in normal and inflamed human colon
defence systems may reduce nitrosative and oxidative stress
without affecting potential protective properties of NO. This
might also be achieved by compounds that inhibits the
mucosal invasion of neutrophils. Also L-arginine may cause
reduced nitrosative and oxidative stress in the colonic
mucosa in ulcerative colitis, in addition to enhanced colonic
microcirculation and secretion of fluid.
In collagenous colitis, inhibitors of iNOS may be expected
to reduce watery diarrhoea, but again the effects on host
defence and neutrophil infiltration is difficult to predict. Thus
further experimental work is needed before inhibitors of iNOS
can be tested in this disorder.
On the other hand, comparative studies of the signalling
pathway(s) involved in the regulation of iNOS in collagenous
colitis and ulcerative colitis may provide new valuable insight
into the pathophysiology of mucosal inflammation.
In conclusion, the present study has demonstrated
production of NO and expression of eNOS and iNOS by the
normal human colon. A highly increased production of NO
was demonstrated in patients with collagenous colitis and
ulcerative colitis, in addition to marked upregulation of iNOS
in the colonic epithelium. Enhanced generation of NO may
contribute to secretion of fluid in human colitis, while
nitrotyrosine-associated NO synthesis may be a cause of
mucosal damage.
SUMMARY
In human colitis, the production of nitric oxide (NO) and the
expression of inducible NO synthase (iNOS) is greatly
increased in the inflamed mucosa, but the pathophysiological
role of NO remains speculative. The purpose of this review is
to discuss the finding of extreme colonic output of NO in the
absence of mucosal injury in patients with collagenous colitis.
In patients with collagenous colitis and severe ulcerative
colitis, there were no differences in colonic output of NO or
expression of iNOS in biopsy specimens from the colonic
mucosa. Nitrotyrosine, which is a marker of nitrosative stress,
was markedly expressed only in ulcerative colitis, suggesting
that reactive nitrogen species, rather than NO per se,
contribute to mucosal injury.
The high expression of iNOS at the luminal border of the
colonic epithelium in patients with colitis is compatible with
the notion that a luminal factor may be responsible for the
induction of iNOS.
In the inflamed colon, NO may act as a secretagogue,
because output of NO and secretion of fluid were reduced by
topical inhibition of NOS by L-NMMA in perfusion studies of
whole colon in patients with collagenous colitis.
While therapeutic actions against iNOS may reduce
nitrotyrosine-associated damage and diarrhoea in colonic
inflammation, the consequences for mucosal microcirculation, recruitment of neutrophils and host defence are
difficult to predict. Further experimental work needs to be
done before testing modulators of NO bioavailability in
patients with chronic inflammatory bowel disorders.
11
DANISH SUMMARY
Ved inflammation i tyktarmen øges slimhindens produktion af
nitrogenoxid (NO), og ekspressionen af inducérbar NO
syntase (iNOS) er øget i biopsier fra colonslimhinden, men
betydningen af disse fund er endnu uafklaret. Denne oversigt
diskuterer betydningen af øget NO produktion ved kollagen
colitis, som er karakteriseret ved vandig diaré uden destruktiv
inflammation.
I kvantitative studier af NO produktionen i colon og
ekspressionen af iNOS i colonbiopsier observeredes
forhøjede værdier både hos patienter med kollagen colitis og
svær colitis ulcerosa. Endvidere fandtes øget ekspression af
nitrotyrosin ved colitis ulcerosa. Det er derfor sandsynligt at
nitrotyrosin og reaktive nitrogen radikaler, men ikke NO i sig
selv, bidrager til slimhinde beskadigelse i den inflammerede
colon.
Ekspressionen af iNOS observeredes i colonepitelet tæt
ved den luminale membran hos patienter med colitis. Fundet
er foreneligt med hypotese om, at luminale faktorer inducerer
iNOS i colonslimhinden. Endvidere er det sandsynligt, at NO
bidrager til øget sekretion af væske fra den inflammerede
slimhinde, da både produktionen af NO og sekretionen af
væske reduceredes ved hæmning af NO syntase med LNMMA i den væskeperfunderede colon hos patienter med
kollagen colitis.
Mens hæmning af iNOS må forventes at reducere
nitrotyrosin-associeret slimhinde destruktion og diaré i den
inflammerede colon, er det vanskelige at forudsige
konsekvenserne for slimhindens gennemblødning, infiltration
af neutrofile granulocytter og barriere funktion. Klinisk
afprøvning af NO modulerende lægemidler i behandlingen af
patienter med kronisk inflammatorisk tarmsygdom må derfor
afvente resultaterne af yderligere eksperimentelle
undersøgelser.
REFERENCES
I.
Perner A, Andresen L, Normark M, Fischer-Hansen B,
Sørensen S, Eugen-Olsen J, Rask-Madsen J.
Expression of nitric oxide synthases and effects of Larginine and L-NMMA on nitric oxide production and
fluid transport in collagenous colitis. Gut 2001; 49: 38794 (Appendix 1).
II.
Perner A, Nordgaard I, Matzen P, Rask-Madsen J.
Colonic production of nitric oxide gas in ulcerative
colitis, collagenous colitis and uninflamed bowel. Scand
J Gastroenterol 2001; in press (Appendix 2).
1.
Moncada S, Palmer RM, Higgs EA. Nitric oxide:
physiology, pathophysiology, and pharmacology.
Pharmacol Rev 1991; 43: 109-42.
Henry Y, Lepoivre M, Drapier JC, Ducrocq C, Boucher
JL, Guissani A. EPR characterization of molecular
targets for NO in mammalian cells and organelles.
FASEB J 1993; 7: 1124-34.
2.
A Perner, PhD thesis
3.
4.
5.
6.
7.
8.
9.
10.
11.
12.
13.
14.
15.
16.
17.
18.
19.
NO in normal and inflamed human colon
Beckman JS, Koppenol WH. Nitric oxide, superoxide,
and peroxynitrite: the good, the bad, and the ugly. Am J
Physiol 1996; 271: C1424-37.
Nathan C, Xie QW. Nitric oxide synthases: roles, tolls,
and controls. Cell 1994; 78: 915-8.
Ignarro LJ, Fukuto JM, Griscavage JM, Rogers NE,
Byrns RE. Oxidation of nitric oxide in aqueous solution
to nitrite but not nitrate: comparison with enzymatically
formed nitric oxide from L-arginine. Proc Natl Acad Sci
USA 1993; 90: 8103-7.
Lewis RS, Tamir S, Tannenbaum SR, Deen WM.
Kinetic analysis of the fate of nitric oxide synthesized
by macrophages in vitro. J Biol Chem 1995; 270:
29350-5.
Boeckxstaens GE, Pelckmans PA, Herman AG, Van
Maercke YM. Involvement of nitric oxide in the
inhibitory innervation of the human isolated colon.
Gastroenterology 1993; 104: 690-7.
Moochhala S, Chhatwal VJ, Chan ST, Ngoi SS, Chia
YW, Rauff A. Nitric oxide synthase activity and
expression in human colorectal cancer. Carcinogenesis
1996; 17: 1171-4.
Izzo AA, Mascolo N, Capasso F. Nitric oxide as a
modulator of intestinal water and electrolyte transport.
Dig Dis Sci 1998; 43: 1605-20.
Fang FC. Mechanisms of nitric oxide-related
antimicrobial activity. J Clin Invest 1997; 99: 2818-25.
Salzman AL, Denenberg AG, Ueta I, O'Connor M, Linn
SC, Szabó C. Induction and activity of nitric oxide
synthase in cultured human intestinal epithelial
monolayers. Am J Physiol 1996; 270: G565-73.
Tepperman BL, Brown JF, Whittle BJ. Nitric oxide
synthase induction and intestinal epithelial cell viability
in rats. Am J Physiol 1993; 265: G214-8.
Whittle BJR. Nitric oxide - a mediator of inflammation or
mucosal defence? Eur J Gastroenterol Hepatol 1997;
9: 1026-32.
Grisham MB, Specian RD, Zimmerman TE. Effects of
nitric oxide synthase inhibition on the pathophysiology
observed in a model of chronic granulomatous colitis. J
Pharmacol Exp Ther 1994; 271: 1114-21.
Ribbons KA, Currie MG, Connor JR, Manning PT, Allen
PC, Didier P, Ratterree MS, Clark DA, Miller MJ. The
effect of inhibitors of inducible nitric oxide synthase on
chronic colitis in the rhesus monkey. J Pharmacol Exp
Ther 1997; 280: 1008-15.
McCafferty DM, Mudgett JS, Swain MG, Kubes P.
Inducible nitric oxide synthase plays a critical role in
resolving intestinal inflammation. Gastroenterology
1997; 112: 1022-7.
Zingarelli B, Szabó C, Salzman A. Reduced oxidative
and nitrosative damage in murine experimental colitis
in the absence of inducible nitric oxide synthase. Gut
1999; 45: 199-209.
Roediger WE, Lawson MJ, Nance SH, Radcliffe BC.
Detectable colonic nitrite levels in inflammatory bowel
disease - mucosal or bacterial malfunction? Digestion
1986; 35: 199-204.
Middleton SJ, Shorthouse M, Hunter JO. Increased
nitric oxide synthesis in ulcerative colitis. Lancet 1993;
341: 465-6.
20.
21.
22.
23.
24.
25.
26.
27.
28.
29.
30.
31.
32.
33.
34.
35.
36.
12
Boughton-Smith NK, Evans SM, Hawkey CJ, Cole AT,
Balsitis M, Whittle BJ, Moncada S. Nitric oxide
synthase activity in ulcerative colitis and Crohn's
disease. Lancet 1993; 342: 338-40.
Lundberg JON, Hellström PM, Lundberg JM, Alving K.
Greatly increased luminal nitric oxide in ulcerative
colitis. Lancet 1994; 344: 1673-4.
Reynolds PD, Middleton SJ, Hansford GM, Hunter JO.
Confirmation of nitric oxide synthesis in active
ulcerative colitis by infra-red diode laser spectroscopy.
Eur J Gastroenterol Hepatol 1997; 9: 463-6.
Iwashita E. Greatly increased mucosal nitric oxide in
ulcerative colitis determined in situ by a novel nitric
oxide-selective microelectrode. J Gastroenterol Hepatol
1998; 13: 391-5.
Singer II, Kawka DW, Scott S, Weidner JR, Mumford
RA, Riehl TE, Stenson WF. Expression of inducible
nitric oxide synthase and nitrotyrosine in colonic
epithelium in inflammatory bowel disease.
Gastroenterology 1996; 111: 871-85.
Halliwell B. What nitrates tyrosine? Is nitrotyrosine
specific as a biomarker of peroxynitrite formation in
vivo? FEBS Lett 1997; 411: 157-60.
Lindström CG. 'Collagenous colitis' with watery
diarrhoea - a new entity? Pathol Eur 1976; 11: 87-9.
Lundberg JON, Herulf M, Olesen M, Bohr J, Tysk C,
Wiklund NP, Morcos E, Hellström PM, Weitzberg E,
Järnerot G. Increased nitric oxide production in
collagenous colitis and lymphocytic colitis. Eur J Clin
Invest 1997; 27: 869-71.
Stack W, Filipowicz B, Hawkey C. Nitric oxide donating
compounds stimulate human colonic ion transport in
vitro. Gut 1996; 39: 93-9.
Jungersten L, Edlund A, Petersson AS, Wennmalm A.
Plasma nitrate as an index of nitric oxide formation in
man: analyses of kinetics and confounding factors. Clin
Physiol 1996; 16: 369-79.
Moshage H, Kok B, Huizenga JR, Jansen PL. Nitrite
and nitrate determinations in plasma: a critical
evaluation. Clin Chem 1995; 41: 892-6.
Bohr J. A review of collagenous colitis. Scand J
Gastroenterol 1998; 33: 2-9.
Gaginella TS, Mascolo N, Izzo AA, Autore G, Capasso
F. Nitric oxide as a mediator of bisacodyl and
phenolphthalein laxative action: induction of nitric oxide
synthase. J Pharmacol Exp Ther 1994; 270: 1239-45.
Devroede GJ, Phillips SF. Studies of the perfusion
technique for colonic absorption. Gastroenterology
1969; 56: 92-100.
Rask-Madsen J, Grove O, Hansen MG, Bukhave K,
Nielsen HR. Colonic transport of water and electrolytes
in a patient with secretory diarrhea due to collagenous
colitis. Dig Dis Sci 1983; 28: 1141-6.
Brittain T, Blackmore R, Greenwood C, Thomson AJ.
Bacterial nitrite-reducing enzymes. Eur J Biochem
1992; 209: 793-802.
Levitt MD. Volume and composition of human intestinal
gas determined by means of an intestinal washout
technic. N Engl J Med 1971; 284: 1394-8.
A Perner, PhD thesis
37.
38.
39.
40.
41.
42.
43.
44.
45.
46.
47.
48.
49.
50.
51.
52.
NO in normal and inflamed human colon
Khriachtchev L, Pettersson M, Runeberg N, Lundell J,
Rasanen M. A stable argon compound. Nature 2000;
406: 874-6.
Phillips SF, Giller J. The contribution of the colon to
electrolyte and water conservation in man. J Lab Clin
Med 1973; 81: 733-46.
Turvill JL, Mourad FH, Farthing MJ. Proabsorptive and
prosecretory roles for nitric oxide in cholera toxin
induced secretion. Gut 1999; 44: 33-9.
Faraci WS, Nagel AA, Verdries KA, Vincent LA, Xu H,
Nichols LE, Labasi JM, Salter ED, Pettipher ER. 2Amino-4-methylpyridine as a potent inhibitor of
inducible NO synthase activity in vitro and in vivo. Br J
Pharmacol 1996; 119: 1101-8.
Moncada S, Higgs EA. Molecular mechanisms and
therapeutic strategies related to nitric oxide. FASEB J
1995; 9: 1319-30.
Linn SC, Morelli PJ, Edry I, Cottongim SE, Szabo C,
Salzman AL. Transcriptional regulation of human
inducible nitric oxide synthase gene in an intestinal
epithelial cell line. Am J Physiol 1997; 272: G1499-508.
Schmidt HH, Murad F. Purification and characterization
of a human NO synthase. Biochem Biophys Res
Commun 1991; 181: 1372-7.
Dimmeler S, Fleming I, Fisslthaler B, Hermann C,
Busse R, Zeiher AM. Activation of nitric oxide synthase
in endothelial cells by Akt-dependent phosphorylation.
Nature 1999; 399: 601-5.
Kuo J, Fox E. Sigma Stat® manual. Microcomputer
tools for scientist. Revision SSD-1.0. Microcomputer
tools for scientist ed. Augsburg: Jandel Scientific, 1992.
Kimura H, Hokari R, Miura S, Shigematsu T, Hirokawa
M, Akiba Y, Kurose I, Higuchi H, Fujimori Y, Tsuzuki Y,
Serizawa H, Ishii H. Increased expression of an
inducible isoform of nitric oxide synthase and the
formation of peroxynitrite in colonic mucosa of patients
with active ulcerative colitis. Gut 1998; 42: 180-7.
Beckman JS, Beckman TW, Chen J, Marshall PA,
Freeman BA. Apparent hydroxyl radical production by
peroxynitrite: implications for endothelial injury from
nitric oxide and superoxide. Proc Natl Acad Sci USA
1990; 87: 1620-4.
Grisham MB, Jourd'heuil D, Wink DA. Nitric oxide.
Physiological chemistry of nitric oxide and its
metabolites: implications in inflammation. Am J Physiol
1999; 276: G315-21.
Radi R, Beckman JS, Bush KM, Freeman BA.
Peroxynitrite-induced membrane lipid peroxidation: the
cytotoxic potential of superoxide and nitric oxide. Arch
Biochem Biophys 1991; 288: 481-7.
Kennedy M, Denenberg AG, Szabó C, Salzman AL.
Poly(ADP-ribose) synthase activation mediates
increased permeability induced by peroxynitrite in
Caco-2BBe cells. Gastroenterology 1998; 114: 510-8.
Beckman JS. Oxidative damage and tyrosine nitration
from peroxynitrite. Chem Res Toxicol 1996; 9: 836-44.
Banan A, Fields JZ, Decker H, Zhang Y, Keshavarzian
A. Nitric oxide and its metabolites mediate ethanolinduced microtubule disruption and intestinal barrier
dysfunction. J Pharmacol Exp Ther 2000; 294: 9971008.
53.
54.
55.
56.
57.
58.
59.
60.
61.
62.
63.
64.
65.
66.
67.
13
Eiserich JP, Estevez AG, Bamberg TV, Ye YZ,
Chumley PH, Beckman JS, Freeman BA. Microtubule
dysfunction by posttranslational nitrotyrosination of
alpha- tubulin: a nitric oxide-dependent mechanism of
cellular injury. Proc Natl Acad Sci USA 1999; 96: 636570.
MacMillan-Crow LA, Crow JP, Kerby JD, Beckman JS,
Thompson JA. Nitration and inactivation of manganese
superoxide dismutase in chronic rejection of human
renal allografts. Proc Natl Acad Sci USA 1996; 93:
11853-8.
Magee PN. Nitrosamines and human cancer:
introduction and overview. Eur J Cancer Prev 1996; 5:
7-10.
Chan JL, Tersmette AC, Offerhaus GJ, Gruber SB,
Bayless TM, Giardiello FM. Cancer risk in collagenous
colitis. Inflamm Bowel Dis 1999; 5: 40-3.
Herulf M, Svenungsson B, Lagergren A, Ljung T,
Morcos E, Wiklund NP, Lundberg JO, Weitzberg E.
Increased nitric oxide in infective gastroenteritis. J
Infect Dis 1999; 180: 542-5.
Wallace JL, Miller MJ. Nitric oxide in mucosal defense:
a little goes a long way. Gastroenterology 2000; 119:
512-20.
Kubes P, Suzuki M, Granger DN. Nitric oxide: an
endogenous modulator of leukocyte adhesion. Proc
Natl Acad Sci USA 1991; 88: 4651-5.
Gaboury JP, Niu XF, Kubes P. Nitric oxide inhibits
numerous features of mast cell-induced inflammation.
Circulation 1996; 93: 318-26.
Kubes P, Granger DN. Nitric oxide modulates
microvascular permeability. Am J Physiol 1992; 262:
H611-5.
Kubes P. Nitric oxide modulates epithelial permeability
in the feline small intestine. Am J Physiol 1992; 262:
G1138-42.
Guo FH, De RH, Rice TW, Stuehr DJ, Thunnissen FB,
Erzurum SC. Continuous nitric oxide synthesis by
inducible nitric oxide synthase in normal human airway
epithelium in vivo. Proc Natl Acad Sci USA 1995; 92:
7809-13.
McCafferty DM, Miampamba M, Sihota E, Sharkey KA,
Kubes P. Role of inducible nitric oxide synthase in
trinitrobenzene sulphonic acid induced colitis in mice.
Gut 1999; 45: 864-73.
Witthoft T, Eckmann L, Kim JM, Kagnoff MF.
Enteroinvasive bacteria directly activate expression of
iNOS and NO production in human colon epithelial
cells. Am J Physiol 1998; 275: G564-71.
Perner A, Andresen L, Pedersen G, Saermark T,
Brynskov J, Rask-Madsen J. Superoxide production in
DLD-1 and HT-29 epithelial cell lines and in primary
epithelial cells from normal human colon.
Gastroenterology 2000; 118: A98.
De Groote MA, Ochsner UA, Shiloh MU, Nathan C,
McCord JM, Dinauer MC, Libby SJ, Vazquez-Torres A,
Xu Y, Fang FC. Periplasmic superoxide dismutase
protects Salmonella from products of phagocyte
NADPH-oxidase and nitric oxide synthase. Proc Natl
Acad Sci USA 1997; 94: 13997-4001.
A Perner, PhD thesis
68.
69.
70.
71.
72.
73.
74.
75.
76.
77.
78.
79.
80.
81.
82.
NO in normal and inflamed human colon
Brown JF, Keates AC, Hanson PJ, Whittle BJ. Nitric
oxide generators and cGMP stimulate mucus secretion
by rat gastric mucosal cells. Am J Physiol 1993; 265:
G418-22.
Húlten L, Lindhagen J, Lundgren O, Fasth S, Ahren C.
Regional intestinal blood flow in ulcerative colitis and
Crohn's disease. Gastroenterology 1977; 72: 388-96.
Bacaner MB. Quantitative measurement of regional
colon blood flow in the normal and pathological human
bowel. Gastroenterology 1966; 51: 764-77.
Eutamene H, Theodorou V, Fioramonti J, Bueno L.
Implication of NK1 and NK2 receptors in rat colonic
hypersecretion induced by interleukin 1 beta: role of
nitric oxide. Gastroenterology. 1995; 109: 483-9.
Closs EI, Enseleit F, Koesling D, Pfeilschifter JM,
Schwarz PM, Forstermann U. Coexpression of
inducible NO synthase and soluble guanylyl cyclase in
colonic enterocytes: a pathophysiologic signaling
pathway for the initiation of diarrhea by gram-negative
bacteria? FASEB J 1998; 12: 1643-9.
Mourelle M, Casellas F, Guarner F, Salas A, Riveros
MV, Moncada S, Malagelada JR. Induction of nitric
oxide synthase in colonic smooth muscle from patients
with toxic megacolon. Gastroenterology 1995; 109:
1497-502.
Simmonds NJ, Allen RE, Stevens TR, Van Someren
RN, Blake DR, Rampton DS. Chemiluminescence
assay of mucosal reactive oxygen metabolites in
inflammatory bowel disease. Gastroenterology 1992;
103: 186-96.
Seo HG, Takata I, Nakamura M, Tatsumi H, Suzuki K,
Fujii J, Taniguchi N. Induction of nitric oxide synthase
and concomitant suppression of superoxide
dismutases in experimental colitis in rats. Arch
Biochem Biophys 1995; 324: 41-7.
Teshima S, Rokutan K, Nikawa T, Kishi K. Guinea pig
gastric mucosal cells produce abundant superoxide
anion through an NADPH oxidase-like system.
Gastroenterology 1998; 115: 1186-96.
Xia Y, Zweier JL. Superoxide and peroxynitrite
generation from inducible nitric oxide synthase in
macrophages. Proc Natl Acad Sci USA 1997; 94: 69548.
Nagase S, Takemura K, Ueda A, Hirayama A, Aoyagi
K, Kondoh M, Koyama A. A novel non-enzymatic
pathway for the generation of nitric oxide by the
reaction of hydrogen peroxide and D- or L-arginine.
Biochem Biophys Res Commun 1997; 233: 150-3.
Powell DW, Mifflin RC, Valentich JD, Crowe SE, Saada
JI, West AB. Myofibroblasts. II. Intestinal subepithelial
myofibroblasts. Am J Physiol 1999; 277: C183-201.
Elliott SN, McKnight W, Cirino G, Wallace JL. A nitric
oxide-releasing nonsteroidal anti-inflammatory drug
accelerates gastric ulcer healing in rats.
Gastroenterology 1995; 109: 524-30.
Aigner T, Neureiter D, Muller S, Kuspert G, Belke J,
Kirchner T. Extracellular matrix composition and gene
expression in collagenous colitis. Gastroenterology
1997; 113: 136-43.
Rachmilewitz D, Karmeli F, Okon E. Sulfhydryl blockerinduced rat colonic inflammation is ameliorated by
83.
84.
85.
86.
87.
88.
89.
90.
91.
92.
93.
94.
95.
96.
14
inhibition of nitric oxide synthase. Gastroenterology
1995; 109: 98-106.
Albina JE. On the expression of nitric oxide synthase
by human macrophages. Why no NO? J Leukoc Biol
1995; 58: 643-9.
Zhang X, Laubach VE, Alley EW, Edwards KA,
Sherman PA, Russell SW, Murphy WJ. Transcriptional
basis for hyporesponsiveness of the human inducible
nitric oxide synthase gene to lipopolysaccharide /
interferon-gamma. J Leukoc Biol 1996; 59: 575-85.
McCafferty DM, Sihota E, Muscara M, Wallace JL,
Sharkey KA, Kubes P. Spontaneously developing
chronic colitis in IL-10/iNOS double-deficient mice. Am
J Physiol 2000; 279: G90-9.
Pfeiffer CJ, Qiu BS. Effects of chronic nitric oxide
synthase inhibition on TNB- induced colitis in rats. J
Pharm Pharmacol 1995; 47: 827-32.
Rachmilewitz D, Karmeli F, Okon E, Bursztyn M.
Experimental colitis is ameliorated by inhibition of nitric
oxide synthase activity. Gut 1995; 37: 247-55.
Hogaboam CM, Jacobson K, Collins SM,
Blennerhassett MG. The selective beneficial effects of
nitric oxide inhibition in experimental colitis. Am J
Physiol 1995; 268: G673-84.
Dobosz M, Mionskowska L, Dobrowolski S, Dymecki D,
Makarewicz W, Hrabowska M, Wajda Z. Is nitric oxide
and heparin treatment justified in inflammatory bowel
disease? An experimental study. Scand J Clin Lab
Invest 1996; 56: 657-63.
Neilly PJ, Kirk SJ, Gardiner KR, Anderson NH,
Rowlands BJ. Manipulation of the L-arginine-nitric
oxide pathway in experimental colitis. Br J Surg 1995;
82: 1188-91.
Di Lorenzo M, Bass J, Krantis A. Use of L-arginine in
the treatment of experimental necrotizing enterocolitis.
J Pediatr Surg 1995; 30: 235-40.
Wallace JL, Vergnolle N, Muscara MN, Asfaha S,
Chapman K, McKnight W, Del-Soldato P, Morelli A,
Fiorucci S. Enhanced anti-inflammatory effects of a
nitric oxide-releasing derivative of mesalamine in rats.
Gastroenterology 1999; 117: 557-66.
Rachmilewitz D, Stamler J, Bachwich D, Karmeli F,
Ackerman Z, Podolsky D. Enhanced colonic nitric oxide
generation and nitric oxide synthase activity in
ulcerative colitis and Crohn's disease. Gut 1995; 36:
718-23.
Herulf M, Ljung T, Hellström PM, Weitzberg E,
Lundberg JON. Increased luminal nitric oxide in
inflammatory bowel disease as shown with a novel
minimally invasive method. Scand J Gastroenterol
1998; 33: 164-9.
Godkin AJ, AJ DB, Villa L, Wong A, Beesley JE, Kane
SP, Martin JF. Expression of nitric oxide synthase in
ulcerative colitis. Eur J Clin Invest 1996; 26: 867-72.
Dijkstra G, Moshage H, Van-Dullemen HM, De-JagerKrikken A, Tiebosch AT, Kleibeuker JH, Jansen PLM,
Van-Goor H. Expression of nitric oxide synthases and
formation of nitrotyrosine and reactive oxygen species
in inflammatory bowel disease. J Pathol 1998; 186:
416-21.
A Perner, PhD thesis
97.
98.
99.
100.
101.
102.
103.
NO in normal and inflamed human colon
Leonard N, Bishop AE, Polak JM, Talbot IC.
Expression of nitric oxide synthase in inflammatory
bowel disease is not affected by corticosteriod
treatment. J Clin Pathol 1998; 51: 750-3.
Kolios G, Rooney N, Murphy CT, Robertson DA,
Westwick J. Expression of inducible nitric oxide
synthase activity in human colon epithelial cells:
modulation by T lymphocyte derived cytokines. Gut
1998; 43: 56-63.
Kimura H, Miura S, Shigematsu T, Ohkubo N, Tsuzuki
Y, Kurose I, Higuchi H, Akiba Y, Hokari R, Hirokawa M,
Serizawa H, Ishii H. Increased nitric oxide production
and inducible nitric oxide synthase activity in colonic
mucosa of patients with active ulcerative colitis and
Crohn's disease. Dig Dis Sci 1997; 42: 1047-54.
Tomobuchi M, Oshitani N, Matsumoto T, Kitano A, Seki
S, Arakawa T. In situ generation of nitric oxide by
myenteric neurons but not by mononuclear cells of the
human colon. Clin Exp Pharmacol Physiol 2001; 28:
13-8.
Islam D, Veress B, Bardhan PK, Lindberg AA,
Christensson B. In situ characterization of inflammatory
responses in the rectal mucosae of patients with
shigellosis. Infect Immun 1997; 65: 739-49.
Casellas F, Mourelle M, Papo M, Guarner F, Antolin M,
Armengol JR, Malagelada JR. Bile acid induced colonic
irritation stimulates intracolonic nitric oxide release in
humans. Gut 1996; 38: 719-23.
Rogler G, Brand K, Vogl D, Page S, Hofmeister R,
Andus T, Knuechel R, Baeuerle PA, Schölmerich J,
Gross V. Nuclear factor kappaB is activated in
macrophages and epithelial cells of inflamed intestinal
mucosa. Gastroenterology 1998; 115: 357-69.
15
104. Nielsen OH, Rask-Madsen J. Mediators of
inflammation in chronic inflammatory bowel disease.
Scand J Gastroenterol 1996; 31: 149-59.
105. Neurath MF, Pettersson S, Meyer zum Buschenfelde
KH, Strober W. Local administration of antisense
phosphorothioate oligonucleotides to the p65 subunit of
NF-kappa B abrogates established experimental colitis
in mice. Nat Med 1996; 2: 998-1004.
106. Ford H, Watkins S, Reblock K, Rowe M. The role of
inflammatory cytokines and nitric oxide in the
pathogenesis of necrotizing enterocolitis. J Pediatr
Surg 1997; 32: 275-82.
107. Lazenby AJ, Yardley JH, Giardiello FM, Jessurun J,
Bayless TM. Lymphocytic ('microscopic') colitis: a
comparative histopathologic study with particular
reference to collagenous colitis. Hum Pathol 1989; 20:
18-28.
108. Fiocchi C. Inflammatory bowel disease: etiology and
pathogenesis. Gastroenterology 1998; 115: 182-205.
ACKNOWLEDGEMENTS
This study was supported by grants from the University of
Copenhagen, the Danish Colitis-Crohn Foundation, the
Research Council of the Copenhagen Hospital Association,
the Novo Nordisk Foundation, Kathrine & Vigo Skovgaard’s
Foundation, LF Foght’s Foundation, the Danish Hospital
Foundation for Medical Research, Region of Copenhagen,
the Faeroe Islands and Greenland, Astra Denmark, Eli Lilly
Denmark, and Pharmacia-Upjohn, Uppsala, Sweden.