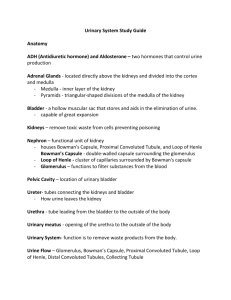
Renal Corpuscle
advertisement

CAL PROGRAM - IA MVST TEXT FOR CAL MODULE ON THE URINARY SYSTEM AND ADRENAL GLAND 1. URINARY SYSTEM The kidneys play a major role in the regulation of both the volume and the composition of the body fluids. This helps to maintain a relatively constant internal environment, critical for enabling the cells to perform their normal functions. The nephrons are the functional units of the kidney. Nephrons achieve the kidney's regulatory role by means of ultrafiltration of the plasma, reabsorption of water and specific molecules and ions from the ultrafiltrate, and secretion of selected solutes into the ultrafiltrate. The end product is the urine. All vertebrate kidneys consist of a large number of nephrons. There are about one million nephrons in each human kidney. The nephron is divided into various segments, each segment structurally and functionally different: 1) The renal or Malpighian corpuscle. 2) Proximal convoluted tubule. 3) Loop of Henle. Present in mammals but missing in fish, amphibians and reptiles. The loop of Henle is responsible for the formation of urine that is more concentrated than plasma. 4) Distal convoluted tubule. 5) Collecting tubules and collecting ducts. This CAL module will focus on mammalian kidney Renal Corpuscle The Malpighian or renal corpuscles are contained in the cortex. Renal corpuscles appear as round structures, surrounded by closely packed tubules of different diameters and staining properties. Each renal corpuscle consists of a glomerulus and Bowman's capsule. The glomerulus is a network of branching and anastomosing capillaries that orginates from an afferent arteriole. It drains into an efferent arteriole (not shown). The glomerulus is encased in Bowman's capsule, a structure resembling an invaginated sphere. Ultrafiltration of plasma takes place in the renal corpuscle. The mesangium is another component of the renal corpuscle. It consists of mesangial cells and extracellular matrix. The mesangium provides structural support to the glomerulus. Mesangial cells are contractile. They surround the glomerular capillaries and participate in the regulation of glomerular filtration. Mesangial cells show phagocytic activity. Extraglomerular mesangial cells are mesangial cells located outside the glomerulus. Vascular and urinary poles The area in which the blood supply enters and leaves the glomerulus is called the vascular pole. This LM shows the afferent arteriole entering Bowman's capsule at the vascular pole. The efferent arteriole, which leaves Bowman's capsule at the vascular pole, is not shown here. The urinary pole is where the proximal convoluted tubule (PCT) joins Bowman's capsule. It is located opposite to the vascular pole. Bowman’s capsule Bowman's capsule consists of two epithelial layers with a space between them (Bowman's space). The plasma filtrate accumulates in Bowman's space before its passage to the proximal convoluted tubule (PCT). The visceral layer, or inner epithelium of Bowman's capsule, is in close association with the glomerular capillaries. This layer turns back at the vascular pole (not shown here) to form the parietal layer. The parietal layer, or outer epithelium, is continuous with the PCT. The plasma ultrafiltrate flows into the PCT from Bowman's space. Podocytes Podocytes (P) are epithelial cells forming the visceral layer of Bowman's capsule. Podocytes have long cytoplasmic extensions called primary processes (P1) that give rise to secondary foot processes (P2), both of which embrace the capillary loops. The parietal layer of Bowman's capsule is made up of squamous epithelial cells. Ultrastructure of the filtration barrier (EM) The glomerular barrier through which plasma is filtered is made up of three components: 1) Capillary endothelium, which contains numerous large fenestrations about 50-100 nm in diameter. 2) Basement membrane, liying between the endothelial cell layer and the epithelial podocyte layer. 3) Podocyte layer. The podocytes foot processes are closely associated with the basement membrane. The foot processes are separated by gaps (filtration slits), bridged by a thin porous diaphragm. The basement membrane functions as a highly selective filter. It is a meshwork of specialised extracellular matrix composed mainly of type IV collagen, proteoglycans and glycoproteins. Removal of proteoglycans impairs the basement membrane filtering properties. Molecules to be filtered are selected based on their size and electrical charge. Negatively charged molecules are not easily filtered because of the electrostatic repulsion by the negatively charge proteoglycans of the basement membrane. Renal Tubules Renal Cortex The majority of tubular segments surrounding the renal corpuscles in the cortex are proximal convoluted tubules (PCT) and distal convoluted tubules (DCT). The sections of PCT are more numerous because the PCT is a much larger segment of the nephron than the DCT. Both the PCT and the DCT are made up of a single layer of cuboidal cells. The main difference is that PCT cells have a brush border that fills part of the lumen. DCT cells lack brush border (their lumen appears clearer), tend to be smaller in size, and stain less intensely with cytoplasmic dyes than PCT cells. Proximal convoluted tubule The brush border of the simple cuboidal epithelium of PCT cells is made up of numerous microvilli. Microvilli increase the plasma membrane surface area for reabsorption. About 70% of the plasma ultrafiltrate is reabsorb by the PCT cells and transported back into the general circulation. Supporting tissue provides a supporting framework for the different components of the renal parenchyma. EM of proximal tubule cell Under EM, the proximal tubule cell shows numerous microvilli on the luminal side. The microvilli plasma membrane contains many transport proteins responsible for the reabsorption of solutes across the luminal plasma membrane. Mitochondria are present in large numbers. They provide the ATP required for active transport processes. The cytoplasm contains endocytotic vesicles and lysosomes involved in the reabsorption and digestion of small proteins and peptides. Renal medulla - Loops of Henle and collecting ducts Loops of Henle, collecting tubules and collecting ducts extend down into the medulla, running in parallel with vasa recta. The descending thin limb of LH loops back to form the ascending thin limb. As the latter returns to the cortex, its wall becomes thicker to form the thick ascending limb of LH. The vasa recta form a parallel set of hairpin loops within the medulla. The thin limbs of loops of Henle are made up of flat epithelial cells with a nucleus protruding into the lumen. They run in close association with vasa recta which have a flat endothelium. Often, the blood content of vasa recta is the only feature that helps to distinguish vasa recta from thin limbs. The loops of Henle, operating as countercurrent multipliers, create a gradient of increasing osmolality in the medullary interstitium that is essential for the concentration of urine. In juxtamedullary nephrons with long loops that run deeply into the medulla, and long thin ascending limbs, the osmotic gradient is spread over a greater distance and the osmolalilty at the tip of the loops is greater. The vasa recta, operating as countercurrent exchangers, help to maintain the interstitial osmotic gradient. Collecting ducts result from the confluence of several collecting tubules, which are made of a single layer of cuboidal cells. Collecting duct cells are columnar, clearly delineated and with a poorly stained cytoplasm. Collecting ducts drain urine into the renal calyces. Antidiuretic hormone (ADH), or vasopressin, regulates the reabsorption of water by collecting duct cells, influencing the final volume and concentration of urine. Juxtaglomerular apparatus The juxtaglomerular apparatus (JGA) consists of the macula densa, the juxtaglomerular cells (JG cells) of the afferent arteriole and the extraglomerular mesangial cells. The macula densa is a specialised region of the distal convoluted tubule, as it passes through the angle formed by the afferent and efferent arterioles. The macula densa cells are in close association with the juxtaglomerular cells. Macula densa cells have a prominent nucleus and are closely packed together (as in this LM). The cells of the macula densa operate as chemoreceptors sensitive to the Na concentration in the tubular fluid. If Na concentration decreases (i.e. due to a decrease in blood pressure and in glomerular filtration rate), macula densa cells promote renin secretion by the JG cells. In the circulation, renin takes part in the formation of angiotensin II. Angiotensin II, among other actions, increases blood pressure by means of its vasoconstrictor effect on arterioles. Angiotensin II also stimulates aldosterone production by the adrenal gland. Aldosterone promotes Na reabsorption and K secretion. ------------------------------------------------------------------------------------The juxtaglomerular apparatus participates in the tubuloglomerular feedback mechanisms that regulate arterial blood pressure, renal blood flow and glomerular filtration. Juxtaglomerular cells, or granular cells, are specialised smooth muscle cells of the wall of afferent arterioles, as they enter the glomeruli. JG cells synthesize renin, which is stored in membrane-bound cytoplasmic granules. Extraglomerular mesangial cells, also called lacis cells, are flat, elongated cells, continuous with the glomerular mesangial cells. They are located in the junction between the afferent and efferent arterioles. Their role is unclear. Urinary Bladder Urine drains from the renal medulla to the lower urinary tract, before its expulsion through the urethra. Renal calyces, ureters and urinary bladder are the components of the lower urinary system. Their surface, and that of the first portion of the urethra, is lined up by a special epithelium known as transitional epithelium, or urinary epithelium. Transitional epithelium is specially adapted to withstand various degrees of distension. For example, in the urinary bladder, which may contain variable volumes of urine. Transitional epithelium is impermeable to water. This prevents water from diffusing out of the cells to hypertonic urine and protects the cells from the potentially toxic effect of urine. Urinary or transitional epithelum The urinary bladder acts as a reservoir for the storage of urine. Its surface is lined up by transitional epithelium. Transitional epithelium is stratified, with several layers of cuboidal or columnar cells. The cell morphology and the number of cell layers changes with the degree of bladder distension. The cell layer number usually ranges from three to six. The luminal surface membrane is thick, has a scalloped appearance, and is impermeable to urine. 2. ADRENAL GLAND The adrenal gland is made of two different components, each with a characteristic type of endocrine tissue: 1. The outer adrenal cortex, which secretes steroid hormones, e.g. glucocorticoids, mineralocorticoids and sex hormones. 2. The inner medulla, which secretes catecholamines, e.g. adrenaline, noradrenaline and dopamine. A capsule of dense supporting tissue surrounds the adrenal gland. Delicate strands of supporting tissue extend from the capsule into the gland parenchyma, providing support to the secretory cells. Notice that the cortex and the medulla differ in appearance and staining properties. A large vein is typically found in the centre of the medulla. Adrenal cortex: The adrenal cortex is divided into three zones according to the type and arrangement of the secretory cells: 1. Zona glomerulosa 2. Zona fasciculata 3. Zona reticularis Two of the three areas of the cortex are shown in the micrograph: The outer zona glomerulosa (G), immediately under the capsule. It usually makes about 5 10% of the mass of the cortex. The intermediate zona fasciculata (F), which usually makes about 75% of the cortex. Collagenous tissue trabeculae (T, stained blue) extend from the capsule (C), providing support to the secretory cells. Zona glomerulosa: The cells of the zona glomerulosa are arranged in irregular whorls surrounded by wide diameter capillaries. The cells have a strongly stained round nucleus and poorly stained cytoplasm. Cells of the zona glomerulosa secrete mineralocorticoids, mainly aldosterone. Aldosterone acts on the kidney, promoting Na reabsorption. Zona fasciculata: The zona fasciculata consists of narrow cords of large cells, separated by sinusoid capillaries. The cytoplasm is very rich in sER and lipid droplets, giving the cells a foamy appearance. Glucocorticoids, mainly cortisol, are secreted by cells from the zona fasciculata. Zona reticularis: The zona reticularis consists of an irregular network of branching cords with numerous capillaries of wide diameter. The cells are smaller than those in the other two cortex layers. Cells of the zona reticularis secrete a small amount of androgenic steroids. Adrenal medulla: The adrenal medulla is arranged in clumps and cords of cells known as chromaffin cells. These are surrounded by fine collagenous supporting tissue containing numerous sinusoids. The cells have a large nucleus and a basophilic cytoplasm. The catecholamine hormones adrenaline and noradrenaline are secreted by the adrenal medulla. Numerous veins (V) draining blood from the cortex reach the central vein by passing through the medulla. The adrenal medulla shows a central vein. Blood from both sinusoid capillaries in the cortex and in the medulla drain into the central vein. EM of adrenal cortex: This EM of the adrenal cortex shows the characteristic features of steroid-secreting cells. The cytoplasm contains numerous lipid droplets, mitochondria (with tubular cristae) and an extensive smooth endoplasmic reticulum. Cholesterol, the common precursor of all steroid hormones, is stored within the lipid droplets. Enlargement of previous EM: The enlargement of the previous EM shows with more clarity the unusual tubular christae of the mitochondria and the extensive network of sER throughout the cytoplasm. Both mitochondria and sER play a major role in the synthesis of steroid hormones. Cholesterol, the common precursor of steroid hormones, is stored in the lipid droplets. EM of adrenal medulla: This EM illustrates the structure of cells from the adrenal medulla. The cells are surrounded by supporting tissue containing capillaries of large diameter. Catecholamines are stored in numerous cytoplasmic membrane-bound granules. The cytoplasm has an extensive endoplasmic reticulum and is rich in mitochondria.