Physician Progress Note / Comprehensive Progress Note
advertisement
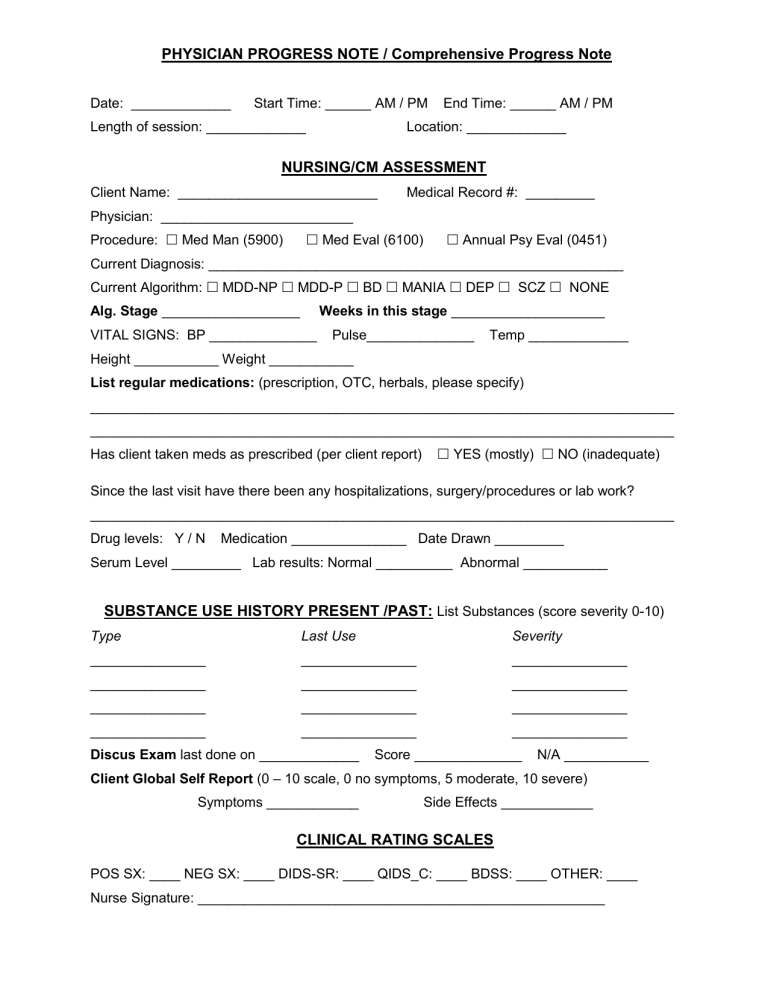
PHYSICIAN PROGRESS NOTE / Comprehensive Progress Note Date: _____________ Start Time: ______ AM / PM Length of session: _____________ End Time: ______ AM / PM Location: _____________ NURSING/CM ASSESSMENT Client Name: __________________________ Medical Record #: _________ Physician: _________________________ Procedure: Med Man (5900) Med Eval (6100) Annual Psy Eval (0451) Current Diagnosis: ______________________________________________________ Current Algorithm: MDD-NP MDD-P BD MANIA DEP SCZ NONE Alg. Stage __________________ Weeks in this stage ____________________ VITAL SIGNS: BP ______________ Pulse______________ Temp _____________ Height ___________ Weight ___________ List regular medications: (prescription, OTC, herbals, please specify) ____________________________________________________________________________ ____________________________________________________________________________ Has client taken meds as prescribed (per client report) YES (mostly) NO (inadequate) Since the last visit have there been any hospitalizations, surgery/procedures or lab work? ____________________________________________________________________________ Drug levels: Y / N Medication _______________ Date Drawn _________ Serum Level _________ Lab results: Normal __________ Abnormal ___________ SUBSTANCE USE HISTORY PRESENT /PAST: List Substances (score severity 0-10) Type Last Use Severity _______________ _______________ _______________ _______________ _______________ _______________ _______________ _______________ _______________ _______________ _______________ _______________ Discus Exam last done on _____________ Score ______________ N/A ___________ Client Global Self Report (0 – 10 scale, 0 no symptoms, 5 moderate, 10 severe) Symptoms ____________ Side Effects ____________ CLINICAL RATING SCALES POS SX: ____ NEG SX: ____ DIDS-SR: ____ QIDS_C: ____ BDSS: ____ OTHER: ____ Nurse Signature: _____________________________________________________ PHYSICIAN ASSESSMENT Time In____Time Out____--Length of session_____ Procedure code______Location__________ Core Symptoms: Mania Depression Positive Symptoms or Psychosis Negative Symptoms Other Symptoms: Irritability Mood Lability Agitation Anxiety Apathy Insomnia Energy Level ↑↓ _____ Appetite ↑↓ _____ Level of Interest ↑↓ _____ Sexual Dysfunction other (specify) __________________________ Is Client suicidal? YES / NO (specify in narrative progress note, including action taken). Is Client homicidal? YES / NO (specify in narrative progress note, including action taken). SUBJECTIVE FINDINGS Appetite: Normal Poor Good Overeating Fair Sleep: Normal Poor Good Fair Medication Efficacy: Excellent Good Fair Poor Minimal Medication Adherence: Excellent Good Fair Poor Minimal Comments: _____________________________________________________________________ ____________________________________________________________________________ Side Effects None Tremors Akathesia Involuntary Movements GI Sexual Appetite Sedation Other______________ Physician Report (0 – 10 scale, 0 no symptoms, 5 moderate, 10 severe) Symptom severity: ___________ Side effect Severity: ___________ OBJECTIVE FINDINGS Orientation: Person Place Time Situation Rapport: Appropriate Hostile Evasive Distant Inattentive Poor Eye Contact Appearance: Appropriately Dressed Appropriately Groomed Body Odor Poorly Dressed Poorly Groomed Disheveled Mood: Euthymic Depressed Anxious Angry Irritable Elated Affect: Appropriate Depressed Expansive Blunted Flat Labile Speech: Coherent Appropriate Incoherent Loose Associations Circumstantial Tangential Poverty Thought Content/Process: Appropriate Goal-Directed Delusional Persecution Reference Thought Insertion Broadcasting Grandiose Obsessions Compulsions Phobias Suicidal Ideation Suicidal Plan Homicidal Ideation Homicidal Plan Hopelessness Worthlessness Loneliness Guilt Self Depreciation Hallucinations (Describe: Auditory Visual Command) Insight: Excellent Good Fair Poor Grossly Impaired Judgment: Excellent Good Fair Poor Grossly Impaired Cognitive: No Gross Cognitive Deficits Concentration Problems Concrete Abstract Easily Distracted Psychomotor Activity: Normal Restless Retardation MemoryImmediate: Good Fair Impaired Recent: Good Fair Impaired Past: Good Fair Impaired Comments: _______________________________________________________________________________ _______________________________________________________________________________ _______________________________________________________________________________ _______________________________________________________________________________ _______________________________________________________________________________ Any new physical problems? (pain, sleep, sexual ) ___________________________________ _______________________________________________________________________________ LMP:______ Pregnancy: __________________________________________________________ ASSESSEMENT DIAGNOSTIC IMPRESSION: Psychiatric (DSM-IV): Axis I: __________________________________________________________________ Axis II: __________________________________________________________________ Axis III: __________________________________________________________________ Axis IV: __________________________________________________________________ Axis V: GAF (0 -100) = _____________________ PLAN: Continue current meds? YES / NO If no, change meds as follows: _______________________________________________________________________________ _______________________________________________________________________________ If, meds are being changed, rationale for change: Insufficient improvement Client preference Side effects intolerable Symptoms worsening Diagnosis change Critical decision point indicates change is necessary Other Risks and benefits of meds were discussed with client? YES / NO If no, give reason: ______________________________________________________________________________ Client consented to taking medication: YES / NO If no, give reason: ______________________________________________________________________________ Is Client capable of administering own meds? YES / NO If not, who will administer? _____________________________________________________________________________ Labs ordered? YES / NO If yes, please see lab order form. ______________________________________________________________________________ SUMMARY ( Additional information only if indicated) _______________________________________________________________________________ _______________________________________________________________________________ _______________________________________________________________________________ _______________________________________________________________________________ _______________________________________________________________________________ Progress Note: check here if note was dictated ________. Date of Dictation ______________. Schedule follow-up in ____________ weeks. _________ month(s) SIGNATURE _____________________________________ Date: ___________________