Diabetes Mellitus Type II Treatment
advertisement

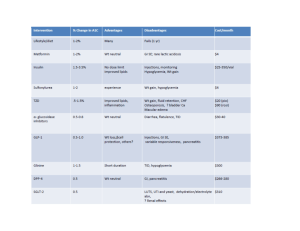
Diabetes Mellitus Type 2 Treatment Table 1. Diagnosis criteria Table 2. Treatment goals Table 3. Oral diabetic medications Clinical judgment may supersede the use of this treatment algorithm Diagnosis of Type 2 DM Provide Medical Nutrition Therapy (MNT) & Diabetes Self Management Training (DSMT). Promote physical activity, SMBG and risk reduction education. FPG 200 mg/dl with or without symptoms FPG < 200 with symptoms FPG < 200 mg/dl without symptoms Continue MNT and exercise without medication for 4-8 weeks HgbA1C < 7.0 % HgbA1C 7.0 % Reassess in 3 months HgbA1c 8.5% HgbA1C 7.0 - 8.5% *May consider initiation of monotherapy when HgbA1C 6.6% - 7.0% if symptoms or risk factors present for end organ damage Monotherapy Initiate Secretagogue OR Insulin Sensitizer Dual Therapy Initiate Secretagogue AND Insulin Sensitizer Consider a sulfonylurea if BMI < 25 kg/m2 OR metformin* if BMI 25 kg/m2 Consider a miglitnide if FPG at goal, but post-prandial blood glucose elevated Consider initiation of oral agent plus bedtime basal insulin if symptoms of polyuria, polydipsia, weight loss or end organ damage present Reassess every 1-2 weeks; if fasting blood glucose remains elevated see table 3 for dose titration * Do not use metformin if SCr > 1.5 in males, SCr > 1.4 in females, CHF or COPD, liver disease or current alcoholics If contraindications; see additional therapy below Reassess every 1-2 weeks; if fasting blood glucose remains elevated see table 3 for dose titration Initiation of insulin therapy also acceptable at this time No Yes; Reassess in 3 months Glycemic goals met within 4 - 12 weeks Glycemic goals met within 4 - 12 weeks No Additional Therapy Insulin Therapy (Appendix A) with bedtime NPH or Glargine Insulin Yes; Reassess in 3 months Thiazolidinediones* (rosiglitazone or pioglitazone) - Do not use in liver disease or CHF Consider using if FPG at goal, but post-prandial blood glucose remains elevated Meglitinide* (repaglinide or naglitanide) - Do not combine with sulfonylurea OR Alpha glucosidase inhibitors* (acarbose or miglitol) *Reassess every 1-2 weeks; if fasting blood glucose remains elevated see table 3 for dose titration Yes; Reassess in 3 months Glycemic goals met within 4 - 12 weeks No Insulin Therapy (Appendix A) Table 1. Criteria for diagnosis of diabetes* Fasting Plasma Glucose 126 mg/dl Casual Plasma Glucose 200 mg/dl plus symptoms (polyuria, polydipsia, unexplained weight loss) Oral Glucose Tolerance Test 2 hour PG 200 mg/dl (75 g anhydrous glucose) Hyperglycemia not diagnostic for diabetes Impaired fasting glucose (IFP) FPG 110 and < 126 mg/dl Impaired glucose tolerance (IGT) 2 hour PG 140 and < 200 mg/dl * Verify on subsequent day if no symptoms present Table 2. Treatment recommendations and goals for diabetes Clinical Practice Recommendations. Diabetes Care;26 suppl 1: January 2003. Glycemic Control HgbA1c <7% Monitor baseline, q 3 months until goal met then q 6 months Plasma blood glucose Whole blood glucose Blood Pressure Lipids LDL Triglycerides HDL Visual Foot Inspection Monofilament Foot Exams Dilated Eye Exams Urine Protein Testing Vaccinations Fasting 90-130 mg/dl Post-prandial < 180 mg/dl Fasting 80-120 mg/dl Post-prandial < 170 mg/dl < 130/80 mmHg < 125/75 mmHg for proteinuria (> 1gram/day) Monitor at least yearly; Q 3-6 months if treatment needed < 100mg/dl < 150 mg/dl > 40 mg/dl Quarterly Annually Annually Annually Flu vaccine yearly Pneumonia vaccine ONCE (repeat once > 65 yo. if previous vaccine was > 5 years prior) Table 3. Oral Diabetes Medications (Bolded are UPMC Health Plan preferred agents) Agent & Strength Initial dose Dose titration Maximum dose Contraindications/ Special Considerations 40 mg/day: give in two divided doses when doses reaches 15 mg/day 20 mg: give in one or two doses Renal dysfunction: do not use if ClCr < 10 ml/min Hepatic dysfunction: use conservative dosing Administer 30 minutes before meals Monitor for s/sx hypoglycemia Secretagogues Sulfonylureas (do not use if hypersensitivity to sulfonamides) Glipizide - short-acting (Glucotrol) 5 mg, 10 mg 2.5 mg/day Increase by 2.5 - 5 mg/day every 1-2 weeks Glipizide – ext. release (Glucotrol XL) 2.5 mg, 5 mg, 10 mg Glimepiride (Amaryl) 1 mg, 2 mg, 4 mg 5 mg/day (2.5 mg if elderly or liver disease) 1-2 mg daily with breakfast or first main meal Increase dose by 2.5 - 5 mg/day no more often than every 1-2 weeks Increase at 1-2 mg/day increments every 1-2 weeks 8 mg daily Renal dysfunction: use with caution if ClCr < 20ml/min Elderly: use conservative dosing Take with breakfast or first main meal Monitor for s/sx hypoglycemia NOTE: Glyburide is not recommend as first line sulfonylurea. Glyburide offers no benefit over Glipizide or Glimepiride and may cause more hypoglycemia as well as an increase in potential drug-drug interactions. Glyburide 2.5 mg/day Increase by 2.5 mg/day every 20 mg; give in one or Renal dysfunction: do not use if (1.25 mg/day if 1-2 weeks two divided doses (Diabeta, Micronase) ClCr < 50ml/min elderly or liver (elderly/liver disease increase by 1.25 mg, 2.5 mg, 5mg Hepatic dysfunction use disease) 1.25-2.5 mg/day every 1- 3 weeks) conservative dosing Glyburide microcrystalline 1.5 mg/day Increase by 1.5 mg/day every 12 mg; If taking more Administer with meals (0.75-1.5 mg/day 1-2 weeks than 6 mg daily give in (Glynase Prestab) Monitor for s/sx hypoglycemia if elderly or liver two divided doses 1.5 mg, 3 mg, 4.5 mg, 6 mg disease) Agent & Strength Initial dose Dose titration Maximum dose Contraindications/ Special Considerations Adjustment based on fasting blood glucose response. Double preprandial dose until 4 mg reached for single dose. Allow at least one week between dose adjustments. 16mg daily; no more than 4 mg per dose (4mg qid with meals) 60-120 mg tid 30 minutes before meals If started on 60 mg tid may increase to 120 mg tid after 2-4 weeks of therapy 120 mg tid Patient should skip dose if meal is skipped to avoid hypoglycemia Take 15 minutes before meals, (effectiveness if taken > 30min prior) Renal dysfunction: CrCl < 40ml/min begin with 0.5 mg and titrate cautiously Hepatic dysfunction: use with caution Monitor for s/sx hypoglycemia Patient should skip dose if meal is skipped to avoid hypoglycemia Elderly: start at 60mg dose Monitor for s/sx hypoglycemia 500 mg with breakfast 500 mg/day at weekly intervals, adding a dose at dinner and then at lunch as tolerated 2550 mg/day (850 mg tid) Meglitinides (no benefit in combination with sulfonylureas) Repaglinide (Prandin ) 0.5 mg, 1 mg, 2 mg HgA1c < 8% 0.5 mg bid or tid with meals HbA1c > 8 % 1 mg or 2 bid or tid with meals Nataglinide (Starlix) 60 mg, 120 mg Insulin Sensitizers Biguanide Metformin (Glucophage) 500 mg, 850 mg, 1000 mg Elderly will not likely tolerate high doses (Glucophage XR ) 500 mg Doses > 2000 mg may increase side effects with little benefit on blood glucose Contraindications: SCr > 1.5 mg/dl (males) OR SCr > 1.4 mg/dl (females) Acute or chronic metabolic acidosis Hepatic dysfunction or known current alcohol abuse COPD or CHF (moderate/severe) Monitoring: GI intolerance Diffuse muscle weakness Thiazolidinediones Rosiglitazone (Avandia) 2 mg, 4 mg, 8 mg 4 mg qd or 2 mg bid May increase to 4 mg bid or 8 mg qd after 12 weeks 8mg daily Pioglitazone (Actos) 15 mg,30 mg, 45 mg 15 mg qd may increase by 15 mg qd every 3 months based on HgA1c response 45 mg daily monotherapy 30 mg daily combination therapy Contraindications: Hepatic dysfunction: Do not use if ALT > 2.5 the upper limits of normal. Type I diabetes Cautions: NYHA class III/IV heart failure; may cause fluid retention Anemia; may worsen blood counts May adversely effect lipids LDL cholesterol (rosiglitazone only) May cause resumption of ovulation in premenopausal anovulatory women Monitoring: LFTs: baseline and then q 2 months for 1 year then periodically. Fluid retention Menstrual irregularities Other oral agents Alpha-glucosidase Inhibitors Acarbose (Precose) 25 mg, 50 mg, 100 mg Miglitol (Glyset) 25 mg, 50 mg and 100 mg 25 mg tid with first bite of meals May start at 25 mg qd if GI distress noted Increase dose to 50 mg tid with meals after 4-8 weeks if necessary. Some may benefit from further increasing the dosage to 100 mg tid if tolerated. 100 mg tid with meals for patient > 60 kg. 50 mg tid with meals for pts 60 kg. 100 mg tid Contraindications: Liver dysfunction: may ALT/AST (Acarbose only) Bowel disorders: inflammatory bowel disease, colonic ulcer, partial obstruction, chronic intestinal problems Renal dysfunction: Do not use if ClCr < 25 ml/min Monitoring: GI intolerance: Abdominal pain, diarrhea, flatulence S/Sx hypoglycemia Should be taken with the first bite of each meal for maximum effectiveness Combination products Glipizide and Metformin (Metaglip) Rosiglitazone and Metformin (Avandamet) Gylburide and Metformin (Glucovance) In general, these products offer little benefit over the individual agents and may actually be of higher cost to the patient. May consider in patients that have been stable for sometime and may have compliance issues with multiple tablets. Would verify insurance coverage or change in patient expense first. Appendix A Insulin Recommendations for Type 2 Diabetes Mellitus Review of Insulin Preparations Type of Insulin Rapid Acting Lispro (Humalog) Aspart (NovoLog) Short Acting Regular (Humulin R/Novolin R) Intermediate Acting Isophane insulin – NPH (Humulin N/ Novolin N) Insulin Zinc – Lente (Humulin L/Novolin L) Long Acting Insulin Zinc Extended – Ultralente (Humulin U) Glargine (Lantus) Premixed Humulin 70/30 (70% NPH/30% Regular) Humulin 50/50 (50% NPH/50% Regular Humalog Mix 75/25 (75% NPL/25% Lispro) Onset of Action Peak Effective Duration Special Considerations 5-15 min 30-90 min 5 hrs Patient should skip dose if meal is going to be missed. 30-60 min 2-3 hrs 5-8 hrs 2-4 hrs 4-10 hrs 10-16 hrs 2-4 hrs 4-12 hrs 12-18 hrs 6-10 hrs 10-16 hrs 18-24 hrs 2-4 hrs no peak 20-24 hrs 30-60 min Mixed as above Mixed as above Mixed as above 10-16 hrs Mixed as above 10-16 hrs 30-60 min 5-15 min 10-16 hrs 10-16 hrs NPL – insulin lispro protamine NovoLog Mix 70/30 (70% NP/30% aspart) 5-15 min NP-protamine aspart May use in patients who need long acting insulin, but are unwilling/unable to give multiple injections as this product can be mixed with other insulins. Cannot mix with other insulins in same syringe or use same syringe. Premixed insulins may be suitable for patients who are unwilling/unable to mix insulin or give multiple injections. Patients must adhere to constant diet and not skip meals. It should be recognized it may be difficult to achieve tight blood glucose control. General guidelines for adjusting insulin doses Patients need to be properly educated on injection technique and insulin dose adjustments. Adjustments in basal insulin dosage should be made only if the increase in blood glucose pattern is not caused by a temporary change in diet, exercise, stress, illness or other medications. These components should be stable before alteration of basal insulin. Short-term adjustments in short or rapid acting insulin may be made to cover this temporary change. Dose adjustment should be made in 1-2 unit increments unless patient has demonstrated little change in blood glucose, then may change at 3-4 unit increments. Also, increments of 3-4 units may be used in patients with blood glucose readings > 200 mg/dl. It should be understood that the degree of insulin resistance varies in patients with Type 2 Diabetes and thus the response to 1 unit of insulin may vary between patients. Insulin adjustments should focus on stabilization of fasting and pre-prandial blood glucose with basal insulin first, and then focus on post-prandial blood sugar adjustment. Target one component to adjust at a time focusing on the highest blood glucose reading. If all readings are elevated > 200mg/dl consider making alterations to all components and focusing on fasting readings. Adjust: Morning short or rapid acting insulin Morning basal insulin or prelunch short or rapid acting insulin Predinner short or rapid acting Predinner or bedtime basal insulin Based on: Prelunch blood glucose Predinner blood glucose Bedtime blood glucose Morning (fasting) blood glucose Initiation of Basal Insulin Patient will need to SMBG 2-4 times daily 2. Start bedtime basal insulin dose of 10 units Glargine or NPH insulin Recommend to use glargine insulin as first line if blood glucose above goal for entire day and NPH insulin if FBS high with good control of daytime blood glucose readings 3. Adjustment of basal insulin Assess fasting blood glucose every 3-4 days Increase basal insulin 1-2 units every 3-4 days until FBG goal of < 120mg/dl met or hypoglycemia occurs (appropriate patients may be instructed to do this) May need to increase in increments of 2-4 units for FBG > 200mg/dl 4. Oral medication considerations Secretagogues - Do not need to discontinue at this time as blood glucose lowering effect may remain on post-prandial readings. If post prandial blood glucose consistently elevated once FBG is at goal may discontinue as patient may not be having benefit; assuming patient following proper meal planning. Insulin Sensitizers – Continue as benefit to increasing receptor sensitivity to insulin. Initiation of Bolus (Short-acting/Rapid Acting) Insulin On oral and/or basal insulin regimen 1. Patient should have stable dose of basal insulin with acceptable fasting blood glucose readings. 2. Initiate rapid acting (lispro or aspart) or regular insulin prior to each meal. The rapid acting insulins are preferable for patients that want more flexibility with timing of meals. Amount of insulin based on post-prandial blood glucose as well as estimation of amount of carbohydrates consumed with each meal. 3. Alternatively, a combination 70/30 product may be initiated for patients that are hesitant to move to four injections a day or have difficulty drawing from multiple vials. The patient needs to have a stable diet and consistent timing of meals to reduce the possibility of hypoglycemia. Combination insulin is to be given 30 minutes before breakfast and dinner. For patients on basal insulin, divide the dose in thirds and give 2/3 in before breakfast and 1/3 before dinner. 4. See general guidelines above for recommendations of insulin dose adjustments. Initiation of Basal and Bolus Insulin For patients not on oral anti-diabetic medications 1. Starting dose of insulin based on total daily dose of 0.2 to 0.5 units per kg as a starting range. 2. Once adequate spacing of meals is established, give 2/3 of total daily insulin dose at breakfast and 1/3 before dinner; with 2/3 of each dose basal insulin and 1/3 bolus insulin. Some people may require the total daily insulin dose to be given 50% in AM and 50% in PM. 3. Dosage adjustments should be made every 4-7 days based on fasting blood glucose first (See general guidelines above for recommendations of insulin dose adjustments.) Conversion of NPH or Ultralente to Glargine Initiate Glargine dose at 70-80% of NPH or Ultralente dose. Glargine insulin cannot be mixed with rapid or short acting insulins and a separate syringe must also be used for administration. Additional Bolus Insulin Patients may add 1 unit of rapid or short acting insulin for every 30-50 points over 150 mg/dl to their current bolus insulin dose. Carbohydrate Counting Patients may be taught carbohydrate counting and coverage with bolus insulin. In general 1 unit of insulin will cover 10-15 grams of carbohydrate. Patients with Type 2 DM may require 1 unit of insulin for 5 grams of carbohydrate. (Refer to Certified Diabetes Educator, Dietitian or Pharmacy Diabetes Consult Service.) Deanne Hall, PharmD 09/18/03