Medical Pharmacology Drug List
advertisement
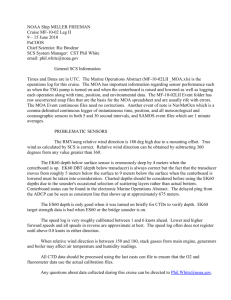
Bennie Berkvens Renal module Pharmacology 2009-2010 Medical Pharmacology Drug List for Renal/Male Reproductive Module 2009 Keeton says “two exam questions about immunosuppressive drugs will test your knowledge of their MOA” For each drug, know the: 1. mechanism of action (MOA) 2. pharmacological effects 3. therapeutic uses 4. toxicity (a.k.a., adverse effects side effects, untoward effects) Immunosuppressive Drugs –(use page 317 as a guide) “once the waiter found out I took immunosuppressive drugs my meal was COMPPT) Cyclosporine (p.323) Moa: Binds cytoplasmic protein (cyclophilin)—this complex inhibits enzymatic action of calcineurin (calmodulin dependent derine/threonine phosphatase) in Helper T-cell no dephosphorylation of NFATC no transcription of the genes for IL-2 and IL-2 receptors, TNF-b, and IFN-gBlocks helper T-cell activation, prevents clonal expansion of T-cells and B-cells, and prevents activation of CTLs (cellular immunity). Uses: primarily suppresses cellular immunity. B cells are still activated by IL-6 (direct Ag stimulation). Organ transplantation, GVHD, Autoimmune disease (RA, MG, psoriasis, DM type 1) S/E: no myelosuppression. Nephrotoxic, hepatotoxic, ↑ viral infections, gingival hyperplasia, neurotoxicity, nausea, vomiting, hirsutism, diarrhea, abd cramping, anorexia, degraded by CYP450. OKT-3 (muromonab-CD3) Moa: Monoclonal Anitbodies directed against CD-3 complex of helper T-cells (Th0) which lies directly next to Ag recognition complex of the T cell blocks binding of foreign Ag presented by the APC no activation of helper T cellsno IL-2 production blocks fxn of CTL. T-cells become inactive and are removed from the RES. Blocks direct activation of helper T, B, and plasma cells by f-MHC. Uses: prophylaxis of early rejection, primary tx for organ rejection, rejection crisis, depletion of T cells from marrow prior to transplant S/E: Cytokine release syndrome, Pulmonary edema, Nephrotoxicity, Neurologic complications, Viral infections, Neoplasms. Mycophenolate Moa: potent inhibitor of the enzyme inosine monophosphate dehydrogenase which is critical in de novo synthesis of the purine Guanine by B and T lymphocytes (these cells have no alternative pathway, HGPRT, for purine biosythesis) suppress lymph proliferation and Ab synthesis by B-cells. Prevents leukocyte recruitment by inhibiting glycosylation of lymph glycoproteins involved in cell adhesion. Uses: renal, cardiac, hepatic transplants. Oral drug for prevention of acute and chronic rejection of renal allografts esp in pts who cannot tolerate cyclosporine or tacrolimus. S/E: sepsis (CMV), diarrhea, leukopenia, GI hemorrhage Prednisone (p. 317) Moa: converted to prednisolone by 11-B-hydroxysteroid dehydrogenase. Causes a leukopenia (↓ T& B lymphs, monocytes, eos, and basophils. ↑ Neutrophils (release from marrow). Interfere w/ APC (macrophage/monocyte/langerhans/dendritic & B cells) fxnblock expression of IL-1 prevents activation of Helper T-cells blocking IL-2 release no activation of TH1 and TH2 cellsno release of IL-4 or IL-6 (from APC)no activation of CTLs or B cells. Block of IL-2 also causes block in expression of TNF-b (↓ expression of adhesion molecules in graft endothelium) and IFN-G (↓ f-MHC II expression in graft). Uses: suppression of both Cellular and Humoral immunity. Use in organ transplantation (rejection crisis), and smaller doses for maintenance immunosuppression. Also, use in autoimmune diseases. S/E: Do NOT cause bone marrow suppression. Hirsutism, acne, PREDNISONE (Pg. 322) Prednisolone Moa: SAME AS PREDNISONE Uses: S/E: Tacrolimus Moa: binds FKBP in T-helper cellsthis complex inhibits calcineurininhibits production of IL-2, IL-2 receptors, TNF-b and IFN-g Uses: 100X more potent then cyclosporine. prevention of acute rejection, allows withdrawal of tx w/ corticosteroids, rescue therapy when OKT-3 is ineffective. S/E: same as cyclosporine Androgen receptor antagonists –Androgens are my Best Friend (BF) Bicalutamide Moa: Competitively block testosterone receptorsloss of feedback inhibition of LH secretion↑ plasma LH and testosterone. Uses: TX of prostatic carcinoma in combination w/ GnRH analog. S/E: Less hepatic toxicity then Flutamide and can be takes once a day. Flutamide Moa: Competitively block testosterone receptors loss of feedback inhibition of LH secretion↑ plasma LH and testosterone. Uses: 1 Bennie Berkvens Renal module Pharmacology 2009-2010 GnRH receptor agonists “for patients with prostatic carcinoma who are takinf GnRH receptor angonists Life’s Good (LG)” Leuprolide Moa: Initial stimulation of LSH and LH release in males and femalesinitial ↑ in plasma testosteroneif given continually in nonpulsatile fashion pituitary GnRH receptors become desensitized (downregulated) ↓ secretion of LH plasma testosterone ↓ to about 10% of normal w/In 2 wks. Uses: 3-4mo depot prep for IM injection. Prostatic carcinoma along w/ androgen receptor antagonist to prevent initial flare up of tumor activity caused by initial ↑ testosterone. TX of endometriosis and uterine fibroid tumors. TX of central precocious puberty S/E: Hot flushes and sweating, Edema, gynecomastia, ↓ libido. Goserelin Moa: Same as Leuprolide Uses: 3mo IM inplant S/E: same as leuprolide Tx of BPH- “if you have BPH, taking OSIN is a pain in the asteride” α1adrenoreceptors are abundant in the SM of the prostate, prostatic capsule, prostatic urethra and bladder neck. Blockade of these receptors causes a reversible relaxation of SM resulting in ↓ urethral resistance to flow. (70% are α-1A subtype) Doxazosin Moa: T1/2 of 22hr. alpha-adrenoreceptor blocker Uses: can be used to TX hypertension and BPH in the same patient! S/E: dizziness, postural hypotension (block of vascular α1 adrenoreceptors), somnolence, asthenia, nasal congestion, peripheral edema, impotence (failure to ejaculate, ↓ volume, retrograde ejaculation). Tamsulosin Moa: selective α-1A adrenoreceptor antagonist. Uses: BPH S/E: less dizziness and orthostatic hypotension then doxazosin. Selectivity for α-1A ↑ incidence of ejaculatory dysfunction. Finasteride (Five-a) Moa: 5α-reductase exists in 2 molecular forms (type 1-liver and skin, and type 2-prostate). Finasteride inhibits TYPE 2. inhibition of 5αreductase prevents DHT formation from testosterone (p. 333). Causes plasma DHT to fall 70% and plasma testosterone to ↑ 10%. It also causes DHT concentration in the prostate gland to ↓ by 70%. Plasma LH is not changed. Inhibition of 5α-reductase prevents hairloss Uses: BPH. ↓ size of prostate. (the larger the prostate the greater the response). ↓ need for TURP. Male pattern baldness S/E: impotence, ↓ libido, 5mg Suppresses Prostate specific Antigen (PSA) by up to 50% (so now require periodic rectal exams), 1mg does not suppress PSA. Dutasteride Moa: Inhibits BOTH type 1 and 2 forms of 5α-reductase forms. Uses: same as Finasteride S/E: reduces serum PSA by 40% Tx voiding dysfunction “all dentists (DDS) take voiding dysfunction drugs” Solifenacin Moa: selective M3 muscarinic receptor antagonist (M3 receptors found on the detrusor muscle of the bladder, as well as in the salivary glands. Uses: TX of urge incontinence (uninhibited contractions of the urinary bladder that overcome the sphincter). Can be given postprostatectomy to prevent bladder spasms. S/E: ↑ Q-Tc, few CNS effects, minimal dry mouth. Darifenacin Moa: selective M3 muscarinic receptor antagonist. Uses: S/E: no CNS or CV effects and no increase in Q-Tc. Minimal dry mouth. Desmopressin (DDAVP) Moa: synthetic analog of AVP (ADH) w/ duration of 6-20hr. selective for V2 receptor found in principle cells of the late distal tubule and collecting duct. ↓ Normal production or urine. Uses: TX of voiding dysfunction, nocturnal enuresis in children. Can be given as Nasal spray before bed. S/E: Nasal spray can cause allergic rhinitis or nasal congestion from URI slow absorption. Tx of erectile dysfunction “ ED drugs should be sold in VATS” Vardenafil Moa: onset 60 min, acts 4-5Hr MOA same as sildenafil Uses: ED S/E: same as sildenafil Alprostadil Moa: PGE1-receptor agonistrelaxation of SM of corpus cavernosa and relaxation of penile SMerection in 5 min (subsides 60-90 min). Uses: used for patients nor responding to sildenafil. S/E: Tadalafil Moa: onset 30-45 min, acts 24Hr. MOA same as sildenafil Uses: ED 2 Bennie Berkvens Renal module Pharmacology 2009-2010 S/E: same as sildenafil Sildenafil Moa: onset 30-60 min, acts 4-5Hr PDEase5 inhibitorprevents CGMP degradationCGMP is now converted to CGMP protein kinaseact of MLC phosphataseprevents MLC phosphorylationrelaxation of vascular SM↑ blood flow erection Uses: ED S/E: smurf vision and impaired blue-green color discrimination (partial blockade of PDEase6 in cones of the retina), ↓ BF to the optic nerveoptic neuropathy, headache and flushing. Severe hypotension when used w/ a nitrate or α-blockers. Diuretic drugs acetazolamide Moa: Proximal Tubule inhibits 80-90% Carbonic anhydrase in PT inhibts 35% HCO3 reab in PT and EDTprevents reab of Na and waterurine becomes alkaline. Loop cannot compensate for loss of Na reab DT [Na] and [HCO3] are highthis causes ↑ K secretion in LDT/CD. CL excretion falls. Uses: glaucoma, altitude sickness, alkalinization of urine to ↑ loss of acidic drug in drug intoxication. S/E: Hyperchloremic metabolic acidosis due to loss of HCO3 and impaired H secretion. When body loses HCO3, CL is retained. Mannitol Moa: TAL ↓Na reab. Freely filtered, not reabsorbed. ↑ RBF and GFR. ↑ urine flow and prevents reab of water in TDL of loop ↓ [NaCl] in TAL (relative to water content)↓ Na reab in TAL. Overall ↑ in urinary excretion of Na, K,Mg, Ca, Cl, HCO3, PO4. salt/water loss directly related to amount of mannitol excreted in urine. (B/c ↑ in urine flow rate, mannitol should be given w/ IV fluid) Uses: prevent complete renal failure in ARF patients, ↓ intraocular pressure in glaucoma, ↓ intracranial pressure if intracranial bleeding is not involved, prevent renal toxicity of cisplatin, Ampho-B, cyclosporine, Myoglobin. S/E: overexpansion of plasma volumeCHF and pulmonary edema. Headache, nausea, hyponatremia. Furosemide Moa: TAL ↓Na reab. Filtered and secreted into PT. Activity not effected by acidosis or alkalosis, effective orally or parenterally, rapid diuresis of short duration, Effective if GFR<25ml/min. Inhibit NA/K/2Cl co-transport in loop↓ reab of NaCl. Distal tubule unable to resorb all extra NaClmassive diuresis. Na/K/Cl symporter blocked in the macula densa ↑GFR due to tuboglomerular feedback block, ↑ vasodilatory prostaglandins, ↑ renin secretion (causes secondary hyperaldosteronism). ↑ Ca, Mg, K, Na, Cl, HCO3, PO4 excretion. Uses: Acute pulmonary edema, edema in cardiac, hepatic, and renal disease. b/c of ↑ GFR and RBF they are useful in TX of CRF and nephrotic syndrome. Also TX hypercalcemia. S/E: hypokalemia-hypochloremic metabolic alkalosis. hypoMg cardiac dysrrhythmias, hyperuricemia gouty arthritis, Orthostatic Hypotension, dilutional hyponatremia, Tinnitis. Hyperglycemia (Furosemide only), Azotemia and coma in renal and hepatic disease. Bumetanide Moa: TAL ↓Na reab Same as Furosemide Uses: same as Furosemide S/E: same as Furosemide ethacrynic acid Moa: TAL ↓Na reab Uses: same as furosemide S/E: same as Furosemide but ↑ risk for tinnitus and hearing loss Hydrochlorothiazide Moa: EDT inhibit NaCl reab in DT. Rapid onset, long duration. Only 5-6% of filtered Na is excreted, GFR consistently reduced, Ineffective if GFR <25 ml/min (except for Metolaxone). At larger doses Thiazides inhibit carbonic anhydrase in PT↑ urinary pH. Do not allow dilute urine production (urine is hypertonic). Enhanced urate reab in PT. ↓ excretion of Ca. ↑ Mg, K, Na, Cl, K, HCO3 excretion. Contraction of ECF volume causes renin secretionsecondary hyperaldosteronism. Uses: first line for HTN. tx edema due to CHF, renal failure, hepatic cirrhosis, premenstrual wt gain, estrogen therapy. TX hypercalcinuria in pts w/ renal calculi. Also ↓ urine output in patients that have Diabetes Insipidus (nephrogenic) b/c ↓ plasma volume ↑ solute/water reab in PTless volume to CD. S/E: secondary hyperaldosteronism, Hypokalemia, HypoMg, Hyperuricemia, dilutional hyponatremia, hyperglycemia (due to block in insulin secretion), azotemia and coma in severe renal and hepatic disease (hypokalemia stim renal prod of ammonia) Metolazone Moa: EDT ↓NaCl reab same as HCTZ Uses: same as HCTZ. Use w/ loop diuretic when PT is reab too much Na massive Na excretion. S/E: Same as HCTZ Spironolactone Moa: LDT/CD K-sparing ↓Na reab. Block aldosterone receptors in the DT (so diuretic activity requires the presence of aldosterone). Weak diuretic (only 2-3%of filtered Na is excreted). ↑ excretion of Na, Cl, HCO3. ↓ excretion of K. very long duration of action. Uses: lessen hypokalemia caused by thiazide (used together). Refractory edema, primary hyperaldosteronism, cirrhosis and nephrotic syndrome, Heart failure (↓ LV wall thickness). S/E: hyperkalemia (do not use w/ oral K), gynecomastia, azoospermia in males and menstrual irregularity and hirsutism in females due to partial agonistic effects at androgen, estrogen, and progesterone receptors. Amiloride Moa: LDT/CD K-sparing ↓Na reab by blocking Na channels on luminal (apical) memb of principal cells in DT and CD. Weak diuretics (2-3% Na excreted). Inhibit secretion of H ion (does not involve CA). ↑ excretion of water, Na, Cl, HCO3 and ↓ excretion of K and H. Uses: use w/ thiazide to ↑ Na loss and to ↓ hypokalemia. Use in CF inhalation of amiloride slows mucus accumulation. S/E: hyperkalemia Triamterene Moa: LDT/CD K-sparing ↓Na reab same as Amiloride Uses: Same as Amiloride S/E: Same as Amiloride 3 Bennie Berkvens Renal module Pharmacology 2009-2010 4