Cardiac Pharmacology Update
advertisement

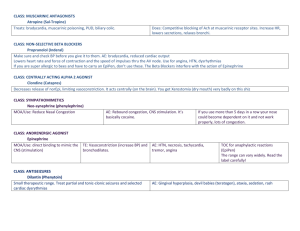
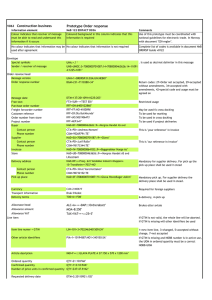
Common Cardiac Medications by Class › Examples › Mechanism of Action (MOA) › Side Effects Common Interactions Questions Examples: › Enalapril (Vasotec), Lisinopril (Prinivil/Zestril), Captopril (Capoten), Benazepril (Lotensin), Fosinopril (Monopril), Quinapril (Accupril), Ramipril (Altace) MOA: › suppresses the renin-angiotensin-aldosterone system; prevention of the conversion of Angiotensin I (AT I) to Angiotensin II (AT II, which is a vasoconstrictor) Vasodilation (↓ afterload, ↓ BP); Prevents cardiac remodeling after MI (prevent development heart failure); Renal protective in DM Side Effects: › ↓BP, ↑ K+, Cough, Angioedema, ↑ SCr & BUN, neutropenia, hepatotoxicity; teratogenic Examples: › Candesartan (Atacand), Irbesartan (Avapro), Losartan (Cozaar), Olmesartan (Benicar), Telmisartan (Micardis), Valsartan (Diovan) MOA: › blocks Angtiotensin II, a vasoconstrictor, at the receptor sites, effect similar to ACE I › Vasodilation (↓ afterload, ↓ BP); Prevents cardiac remodeling after MI (prevent development heart failure); Renal protective in DM Side Effects: › ↓BP, ↑ K+, ↑ SCr & BUN, teratogenic › Same as ACE-I, except w/o cough Examples: › Selective BB Metoprolol (Lopressor/Toprol XL), Atenolol (Tenormin), Betaxolol (Corgard), Bisoprolol (Zebeta), Nebivolol (Bystolic) › Non-Selective BB Propranolol (Inderal), Labetalol (Trandate), Carvedilol (Coreg), Nadolol (Corgard) MOA: ↓HR, ↓BP, and ↓ force of contraction › Selective BB block the beta1 adrenergic receptors of the heart—blocking of catecholemines › Non-Selective BB blocks both beta1 receptors (heart) and beta2 receptors (bronchial and vasculature sites) Side Effects: › bradycardia, hypotension, masks symptoms of hypoglycemia, fatigue, lethargy, wheezing/dyspnea nightmares, insomnia, impotence Non-Selective BB: Bronchospasm and vasoconstriction Use w/ caution in asthma, COPD, PVD, DM Examples: › Non-Dihydropyridines—Verapamil (Calan/Covera/Verelan/Isoptin), Diltiazem (Cardizem/Tiazac/Diltia/Cartia/Diltzac/Dilacor); › Dihydropyridines—Amlodipine (Norvasc), Felodipine (Plendil), Isradipine (DynaCirc), Nicardipine (Cardene), Nifedipine (Procardia/Adalat), Nisoldipine (Sular) MOA: ↓ HR, ↓ Contractility, vasodilation › inhibits influx Ca+ into cardiac and vascular smooth muscle cells Side Effects: › ↓ HR, ↓BP, edema, angioedema, gingival hyperplasia, HA, flushing, dizziness › Constipation (verapamil), CHF exacerbation (verapamil/diltiazem), drug interactions (verapamil/diltiazem) MOA: › Increases force of heart contractions, ↓ HR Side Effects: › Manifestations of Toxicity: Anorexia, N/V/D, visual changes, arrhythmias (PVCs), bradycardia › Increased Risk of Toxicity: Renal impairment, low K+/Mg+, elderly, hypothyroid; Drug interactions • Examples: Loop— Furosemide (Lasix), Bumetanide (Bumex), Torsemide (Demedex), Ethacryinic Acid Thiazide— Hydrochlorothiazide (HCTZ), Chlorthiazide (Diuril), Chlorthalidone, Metolazone (Zaroxolyn) Potassium Sparing— Amiloride, Triamterene; Aldosterone Antagonists— Spironolatone (Aldactone), Eplerenone (Inspra) • MOA: eliminates extracellular fluid Loop: inhibits Cl- reabsorption in loop of Henle Thiazide: inhibits reabsorption of Na+ and water, vasodilation Potassium Sparing: inhibits K+ channels Aldosterone Antagonists: block aldosterone Loop: ↓K+, ↓Na+, ↓Ca+, ↓Mg+; Ototoxicity, Photosensitivity, Dehydration Thiazide: ↓K+, ↓Na+, ↓Mg+; Hyperglycemia, ↑ Lipids, ↑Ca+, dehydration Triamterene/Amiloride: ↑ K+, GI upset, photosensitivity Spironolactone, etc.: ↑ K+, Gynecomastia, drowsiness, GI upset Examples: Hydralazine, Minoxidil MOA: › Relaxation smooth muscle, lowering pressure needed to push blood through vessels Side Effects: › Hydralazine: Headache, drug fever, peripheral neuropathy, hepatitis, skin reactions › Minoxidil: Hair growth, fluid overload, use with BB to prevent reflex tachycardia Examples: › Nitroglycerin, Isosorbide Mononitrate (ISMO, Monoket, Imdur), Isosorbide Dinitrate (Isordil) MOA: › Relaxation of smooth muscle, lowering pressure needed to push blood through vessels Side Effects: › Headache, flushing, hypotension, syncope, cyanosis (blue) may indicate methemiglobinemia Examples › Alpha-1 Receptor Blocker—Doxazosin, Prazosin, Terazosin › Centrally Acting Agents—Clonidine, Methyldopa, Guanabenz, Guanfacine MOA › Alpha-1 Receptor Blocker Peripheral relaxation of smooth muscle causing vasodilation › Centrally Acting Agents Stimulates alpha-2 adrenergic receptors in brain causing a peripheral reduction in sympathetic tone—↓ HR, ↓CO, ↓ peripheral resistance Side Effects › Dizziness, drowsiness, syncope/hypotension, depression, dry mouth, rebound HTN Examples › Aspirin, Clopidrogel (Plavix), Prasugrel (Effient), Dipyridimole, Ticlodipine (Ticlid) MOA › Inhibits platelet aggregation and clot formation Side Effects › Bleeding › GI upset, thrombocytopenia Heparin, Enoxaparin (Lovenox), Dalteparin (Fragmin) MOA—disruption of clotting cascade (antithrombin III) Side Effects—bleeding, thrombocytopenia Warfain (Coumadin) MOA—disruption of vitamin K dependent clotting factors Side Effects—bleeding, skin necrosis Statins (Atorvastatin, Fluvastatin, Lovastatin, Pravastatin, Rosuvastatin, Simvastatin) › MOA: blocks cholesterol synthesis and increases catabolism › Side Effects: HA, GI upset, elev LFT’s, myopathy, rhabdomyolysis; › **New FDA Warning not to exceed 40mg/day Simvastatin unless previously stable on dose without side effects. Do not increase patients beyond 40mg. Fibric Acid Analogs (Gemfibrozil, Fenofibrate) › MOA: Decreases VLDL synthesis; increases VLDL/Triglyceride removal › Side Effects: elev LFT’s, myopathy, GI upset, diarrhea, cholelithiasis, rash/itching Cholesterol Absorption Inhibitor (Ezetimibe) › Side Effects: headache, angioedema Omega 3 Fatty Acids (Lovaza) › Side Effects: halitosis, GI upset, weight gain, prolonged bleeding time Niacin › Side Effects: flushing, itching, GI upset, hyperglycemia, elev LFT’s, elevated uric acid, myopathy w/ high dose statins/fibrates Bile Acid Sequestrants › Side Effects: GI upset, bloating, constipation, drug interactions (decreases absorption) Class Ia Anti-Arrhythmic Agents Depresses pacemaker rate, conduction and excitability › Quinidine Side Effects: syncope, TdP, ↓ BP, n/v/d, HA, dizziness, tinitis, fever, thrombocytopenia › Procainamide Side Effects: hypotension, TdP, SLE, n/v/d, fever, rash, hepatitis, agranulocytosis, HA, mood changes Class Ib—Lidocaine Depresses abnormal cardiac activity, shortens action potential duration, prolongs diastole (extending time for recovery) Side Effects: Hypotension, parasthesias, nausea, tremor, syncope, hearing disturbances, slurred speech, seizures Class Ic—Propafenone Similar to Quinidine, weak BB Side Effects: metalic taste, proarrhythmias Class II—Beta-Blockers Class III › Amiodarone Broad spectrum of activity: lengthens action potential, weak CCB, non-competitive BB, alpha-receptor blocker Effects: vasodilatation, bradycardia, heart block, TdP, pulmonary fibrosis, corneal deposits, visual disturbances, sun sensitivity, skin discoloration, constipation, hepatic dysfunction, ataxia, HA, tremor, drug interactions • Class III, cont. › Dronedarone Similar to amiodarone Effects: bradycardia, TdP, GI upset, weakness, rash, liver injury, hepatic failure; new agent › Sotolol Non-selective BB, prolongs action potential Side Effects: fatigue, bradycardia, dizziness, dyspnea, proarrhythmias Class IV—CCBs (Verapamil/Diltiazem) › Drugs affecting Absorption Antibiotics alter GI Flora, affecting Warfarin › Drugs affecting Protein Binding › Drugs affecting Metabolism Increases Metabolism of Medication Rifampin ↑ warfarin metabolism, decreasing INR Decreases Metabolism of Medication Amiodarone inhibits hepatic enzymes from metabolizing key medications › Drugs affecting Excretion Amiodarone decreases digoxin clearance Cialis/Viagra/Levitra potentiate Nitrates/Vasodilators = Hypotension! › Important to know if patients are taking these medications Warfarin—Everything! › “the biggies” Amiodarone Sulfamethoxazole (Septra/Bactrim) Metronidazole (Flagyl) Quinolones (Cipro, etc) Rifampin Medications Effect on PT/INR Mechanism Estrogens, Vitamin K ↓ Methimazole, Propylthiouracil Barbituates, carbamazepine, chronic ETOH, dicloxacillin, nafcillin, rifampin, phenytoin ↓ Increased synthesis of clotting factors Reduced catabolism of clotting factors ↓ Increased warfarin metabolism cholestyramine, colestipol, sucralfate azathioprine, cyclophosphamide, cyclosporine, mesalamine ↓ Reduced warfarin absorption ↓ thyroid hormones ↑ cetotetan, vitamin E ↑ Broad spectrum antibiotics acute ETOH, allopurinol, amiodarone, azithromycin, ciprofloxacin, erythromycin, clarithromycin, fluconazole, fluorouracil, fluoxetine, ketoconazole, metronidazole, omeprazole, phenytoin, sulfamethoxazole, propafenone acetaminophen, androgens, vitamin C, clofibrate, corticosteroids, gemfibrozil, statins ↑ Unexplained Increased catabolism of clotting factors Decreased synthesis of clotting factors Impaired Vitamin K production by GI flora ↑ Decreased warfarin metabolism ↑ Unexplained aspirin, clopidrogel, NSAIDs, SSRIs, ticlodipine 0 Increased bleeding risk NSAIDs & ACE-I › Can reduce the antihypertensive effect of ACE-I or cause/worsen renal failure Digoxin & Amiodarone › May need less digoxin if on chronic amiodarone Drugs prolonging QT interval › Can cause arrhythmia when combined with other drugs prolonging QT interval Anti-arrhythmic medications known to prolong QT Interval › Amiodarone › Dofetilide › Procainamide › Quinidine Other medications with potential to prolong QT Interval › Droperidol › Erythromycin › Clarithromycin › Haloperidol › Methadone › Ziprasidone › Many others… ????