Respiratory failure
advertisement

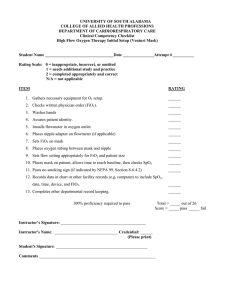
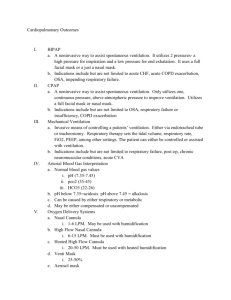
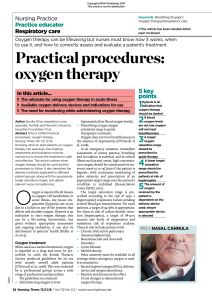
7.13 Respiratory failure (7.13.1) Recognise a patient in respiratory failure Presentation will be that of the cause for the failure (see 7.13.2) together with symptoms and signs of either hypoxia (type 1 respiratory failure) or hypoxia and hypercapnia (type 2). Hypoxia: PaO2 <8 kPa If long standing: Dyspnoea Polycythaemia Restlessness Pulmonary Agitation hypertension Confusion Central cyanosis Cor pulmonale Hypercapnia: PaCO2 >6 kPa Headache Tremor / flap Peripheral Papilloedema vasodilatation Confusion Tachycardia Drowsiness Bounding pulse Coma (7.13.2) Assess the cause and severity of respiratory failure and initiate management The purpose of the lungs is gaseous exchange – this process requires the following: Pumping of blood to the lungs by the heart Inspiration and expiration – powered by muscle and controlled by the respiratory centre of the medulla. Impulses conveyed down the spinal cord and through peripheral nerves. A suitable environment for exchange at the alveoli (V:Q matching, no barriers to diffusion) Causes Type 1 resp failure PaO2 <8 kPa; PaCO2 norm/ Type 2 respiratory failure: PaO2 <8 kPa; PaCO2 >6 kPa Pneumonia Pulm oedema PE Asthma Emphysema Fibrosing alveolitis Pulmonary disease: Asthma COPD Pneumonia Pulm fibrosis Obstructive sleep apnoea Reduced Respir. drive Right left shunt Sedative drugs Cyanotic congenital heart CNS tumour disease Trauma Causes in italic may result in type I or II failure. Neuromuscular: Cervical cord lesion Poliomyelitis Gullaine Barré Myasthenia gravis Muscular dystrophies Diaphragmatic paralysis Thoracic wall disease Flail chest Kyphoscoliosis The severity may be assessed by O2 SATS (pulse oximeter) and arterial blood gas. Management Investigations to ascertain cause: Bloods: FBC, U&E, CRP, ABG Radiology: CXR Microbiology: Blood / sputum culture (if febrile) Spirometry Treat underlying cause Give oxygen (see 7.13.5) (7.13.3) Interpret arterial blood gas results An arterial blood gas sample is taken usually from radial artery at wrist or brachial artery in cubital fossa. Sample is kept in ice and must be processed within 30 minutes. Normal values are: pH: pCO2: pO2: [HCO3-]: Base excess: 7.35 – 7.45 4.7 – 6.0 kPa >10.6 kPa 22-25 mmol/L (standardised bicarbonate) +/- 2 mmol/L Base excess is the amount of acid (if negative) or alkali (if positive) that would be needed to bring the pH to 7.4. It is therefore negative in acidosis and positive in alkalosis If the problem is respiratory then pH and pCO2 change in the opposite directions (mnemonic ROD) Respiratory acidosis: pH, pCO2 Respiratory alkalosis: pH, pCO2 If the problem is metabolic then pH and [HCO3-] change in the same direction. Metabolic acidosis: pH, [HCO3-] Metabolic alkalosis: pH, [HCO3-] It is also important to look at the FiO2 value – this is a value input by the user of the blood gas machine. It is the concentration of O2 the patient was receiving at the time the sample was taken (e.g. .21 in normal air) Background box: useful facts about ABGs The blood gas syringe and needle – what is special about them: The syringe and needle come in a package together – the syringe contains vacuum and heparin (in a small rectangular piece of paper) – it will draw blood into itself with the heparin preventing clotting. Allens test can be performed before taking an ABG from the radial artery – it ensures patency of the collateral supply from the ulnar artery: Press hard upon the patients radial and ulnar arteries and get the patient to make a fist, hold for a few seconds then relax – the palm will go white. If the grip on the ulnar artery is released and the palm goes red again then the collateral supply is Ok and you may proceed to take blood from the radial artery. ABG results are printed on thermal paper – this fades with time. Always write the results down and do not simply attach them to the notes. (7.13.4) Use and interpret results from a pulse oximeter The pulse oximeter allows non-invasive measurement of peripheral O2 saturation (‘sats’) by way of a probe attached to fingertip or earlobe. Results <90% require attention; <80% is clearly abnormal and action is required unless this is normal for the patient (e.g. COPD). In children, any result below 96% requires urgent action (oxygen). Results from a pulse oximeter must be treated with caution – the following can result in erroneous readings: Cold peripheries (poor perfusion) Skin pigmentation Take an ABG when indicated Excess light CO poisoning (cherry red colour) Methaemaglobnaemia Nail varnish (7.13.5) Prescribe oxygen and oxygen delivery systems appropriately Oxygen is a drug – it must be prescribed. Use the normal cardex – there is often a dedicated ‘medical gas’ section on page 1. If not write as a normal drug and ring around all the time slots to indicate continuous supply. Do not prescribe PRN – it is unlikely to be given. Hypoxia kills faster than hypercapnia and CO2 retainers are rare (even in those with COPD) – if in doubt start O2 at 40% and move from there. If ABG shows >1.5 kPa increase in PaCO2, consider a respiratory stimulant (e.g. doxapram 1.5 – 4 mg / min IV) or assisted ventilation (e.g. NIPPV – non-invasive positive pressure ventilation). Oxygen delivery systems are divided into fixed and variable delivery systems: A fixed performance device utilises the HAFOE principle (High Air Flow with Oxygen Enrichment). O2 (A) flows into a jet (B) to entrain air through apertures (C) in the venturi barrel (D). The resultant air/oxygen mixture containing the prescribed O 2 concentration flows into the face piece (E) for patient breathing. Surplus gas leaves the mask through the holes (F) to flush out expired CO2. When oxygen flow is increased, more air is entrained, to maintain a constant oxygen concentration. This means that the exact FiO2 is known and does not vary. One example of this type of mask is the Venturi Mask in which the colour of the mask’s aperture reflects the FiO 2 achieved (24%: blue; 28%: white; 35%: yellow; 40%: red; 60%: green). The flow rate of oxygen to be used with each colour is printed on the Venturi barrel. Changing the FiO2 means a new mask is needed. This is a Hudson mask – a commonly used type of variable flow delivery system. The advantage of this system is that the FiO2 can be varied simply by changing the flow rate of O2. The disadvantage is that the exact FiO2 varies with the patient’s breathing pattern and cannot be exactly known. The last commonly used delivery system is nasal cannulae (right) – these too are a variable system – they may be used with up to 4L of oxygen and are not likely to achieve FiO2 greater than 28%. They are useful for patients who are normally on low levels of home oxygen treatment. So what system should I use? Well but slightly low SATs Nasal cannulae Long term home oxygen Hudson mask if required FiO2 <50% (approx 50% with 15L / min flow) Asthma / LVF / pneumonia Add a reservoir bag if required FiO2 >50-70% (at 15 L / min flow) COPD Venturi mask More detail is available from: http://www.studentbmj.com/issues/04/02/education/56.php Nasal Cannulae Venturi Mask Hudson Mask Hudson mask + reservoir bag