CHAPTER 35
Medical Gas Therapy
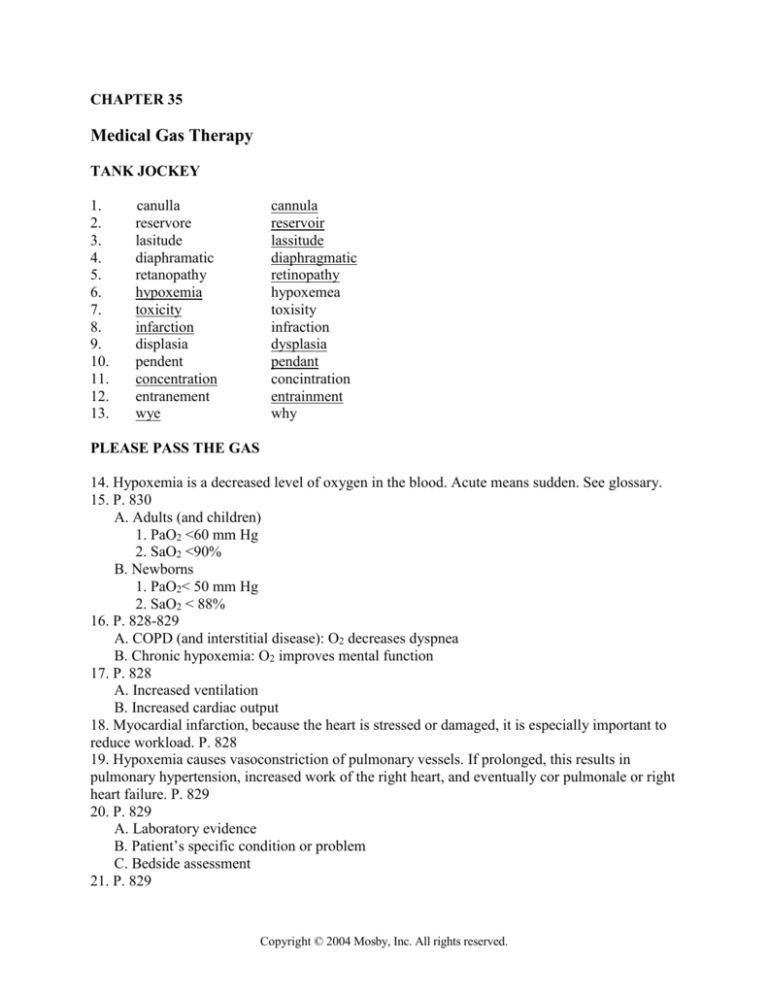
TANK JOCKEY
1.
2.
3.
4.
5.
6.
7.
8.
9.
10.
11.
12.
13.
canulla
reservore
lasitude
diaphramatic
retanopathy
hypoxemia
toxicity
infarction
displasia
pendent
concentration
entranement
wye
cannula
reservoir
lassitude
diaphragmatic
retinopathy
hypoxemea
toxisity
infraction
dysplasia
pendant
concintration
entrainment
why
PLEASE PASS THE GAS
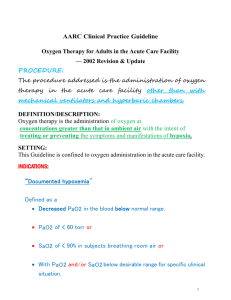
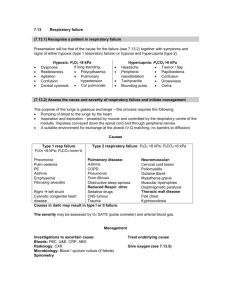
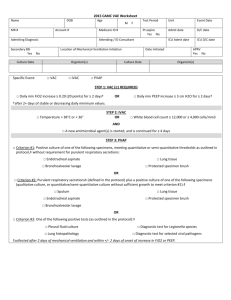
14. Hypoxemia is a decreased level of oxygen in the blood. Acute means sudden. See glossary.
15. P. 830
A. Adults (and children)
1. PaO2 <60 mm Hg
2. SaO2 <90%
B. Newborns
1. PaO2< 50 mm Hg
2. SaO2 < 88%
16. P. 828-829
A. COPD (and interstitial disease): O2 decreases dyspnea
B. Chronic hypoxemia: O2 improves mental function
17. P. 828
A. Increased ventilation
B. Increased cardiac output
18. Myocardial infarction, because the heart is stressed or damaged, it is especially important to
reduce workload. P. 828
19. Hypoxemia causes vasoconstriction of pulmonary vessels. If prolonged, this results in
pulmonary hypertension, increased work of the right heart, and eventually cor pulmonale or right
heart failure. P. 829
20. P. 829
A. Laboratory evidence
B. Patient’s specific condition or problem
C. Bedside assessment
21. P. 829
Copyright © 2004 Mosby, Inc. All rights reserved.
2
A. Carbon monoxide poisoning
B. Cyanide poisoning
C. Shock
D. Trauma
E. Acute myocardial infarction
F. Postoperative patients
22. P. 829 Table 35-1
System
Mild
A. Respiratory
Tachypnea
Dyspnea
B. Cardiovascular
Tachycardia
Mild hypertension
C. Neurologic
Restlessness
Disorientation
Severe
Tachypnea
Dyspnea
Tachycardia then bradycardia
Hypertension then hypotension
Somnolence
Confusion
WHAT COULD GO WRONG?
Toxic Talk
23. P. 831
A. Lungs
B. CNS
24. P. 831
A. PO2
B. Exposure time
25. P. 831 Table 35-2
Tracheobronchitis and substernal chest pain develop during the first 12 hours. Next, vital
capacity and lung compliance begin to decrease (12-30 hours). A state similar to
bronchopneumonia develops. The alveoli and capillaries are damaged, resulting in interstitial
edema. Type I cells are destroyed. In the end stages hyaline membranes form, then pulmonary
fibrosis and hypertension develop.
26. High FIO2 causes O2 toxicity, which causes shunting, which results in lower PO2 levels,
which require higher FIO2 levels for treatment. P.831 Figure 35-2
27. Limit exposure to 100% oxygen to less than 24 hours whenever possible. High FIO2 levels
are acceptable if the concentration can be lowered to 70% within 2 days, and 50% within 5 days.
P. 832
28. Never. P. 832
I feel depressed...
29. Patients who are breathing from their hypoxic drive. P. 832
30. P. 832
A. Suppression of peripheral receptor drive to breathe increased CO2
B. Worsening V/Q increases CO2
31. Never. P. 832 (Sounds like we’re in never never land!)
RFL or ROP, it’s all the same to me!
Copyright © 2004 Mosby, Inc. All rights reserved.
3
32. Oxygen causes retinal vasoconstriction and vascular necrosis. New blood vessels form and
cause hemorrhages and scarring which leads to retinal detachment and blindness. P. 832
33. Premature infants and neonates up to 1 month. P. 832
34. Maintain PO2 levels less than 80 mm Hg. Minimize other factors such as acidosis. P. 832
Absorbing Information
35. FIO2 levels above 0.50 cause atelectasis by washing nitrogen out of poorly ventilated units
and depleting nitrogen from tissues. The oxygen is then used up physiologically and the alveoli
collapse. P. 832
36. Patients with low tidal volumes due to sedation, surgical pain, or CNS dysfunction.
P. 832
37. Use lower FIO2 levels. Encourage deep breathing. (not in text)
OXYGEN DELIVERY SYSTEMS
38. P. 833
Category
A. Low-flow 2
B. Reservoir 3
C. High-flow 1
Description
1. Always exceeds patient’s inspiratory needs
2. Provides some of patient’s inspiratory needs
3. May meet needs if no leaks occur
LOW-FLOW
39. Well tolerated, simple, easy to use, low-cost, disposable, all ages. P. 836
40. When flows are greater than 4 L/min (also with infants and children). P. 836
41. 2 L/min P. 836
Experiment
Questions
Discuss these answers with your instructor if you perform the exercises.
42. Lowers O2 usage and cost.
43. Many variables affect the FIO2 delivered by all low-flow systems including mouth breathing,
respiratory rate, tidal volume, inspiratory flowrates, minute ventilation, etc. P. 834 Table 35-3
44. Assess the actual response to the oxygen-physical assessment and pulse oximetry or ABGs.
45. A. Advantages: lower O2 usage and cost, increased mobility, less discomfort
B. Disadvantages: unattractive, cumbersome, affected by pattern, poor compliance
46. The home.
RESERVOIR
47. Table 35-3 P. 834
Mask
A. Simple
B. Partial
C. Non
FIO2 range (%)
35-50
35-60
55-70
Advantage
Cheap, easy
Moderate FIO2
High FIO2
Copyright © 2004 Mosby, Inc. All rights reserved.
Disadvantage
Comfort, vomitus
See simple mask
Suffocation hazard
4
48. Valves. Particularly between the bag and the mask. P. 839
49. The bag does not fully deflate on inspiration. P. 840
50. P. 841 Table 35-6
Problem
Solution
A. Confused patient removes mask
Restrain patient
B. Humidifier pop-off activated
Find obstruction, omit humidifier
C. Mask causes claustrophobia
Use another device
D. Bag collapses on inspiration
Increase flow
E. Bag fully inflated on inspiration
Correct leak, fix/replace mask
Experiment
Questions
Discuss these questions with your instructor if you perform the exercises.
HIGH-FLOW
51. P. 842
Factor
Increased size
Decreased size
A. Jet
1. FIO2
Increased FIO2
Decreased FIO2
2. Flow
Decreased flow
Increased total flow
B. Port
1. FIO2
Decreased FIO2
Increased FIO2
2. Flow
Increased flow
Decreased total flow
52. P. 843 Table 35-7
A. 100%
0:1
B. 60%
1:1
C. 40%
3:1
D. 35%
5:1
E. 30%
8:1
F. 24%
25:1
53. Venti-mask or Venturi mask. P. 844
54. Allows excess flow and patient exhalation to escape. P. 844
55. Little or no effect. P. 844
56. 35% or less. P. 844
57. Increase the input flow. P. 844
58. The small jets limit the oxygen flowrates through the device. P. 845
59. P. 845 Figure 35-16
Patient
Aerosol appliance
A. Tracheostomy tube
T-piece or tracheostomy collar
B. Endotracheal tube
T-piece
C. Intact upper airway
Face tent, aerosol mask
60. P. 845
Observe the mist on the expiratory side when the patient inhales. Calculate the flow delivered by
the device. Measure the patient’s minute ventilation and multiply by 3. Compare the two values.
Copyright © 2004 Mosby, Inc. All rights reserved.
5
61. P. 847
A. Aerosol: Gas injection nebulizer
B. Dry: Downs flow generator
62. Downstream resistance increases the FIO2 and decreases total flow delivered. P. 845-6
Experiment
Questions
Discuss if you have the students do these experiments.
MATHEMAGIC
63. P. 843
A. Step 1—Compute the ratio
Formula: 100% %O2 ÷ %O2 21
Calculation: 100 60 ÷ 60 21
Reduce answer to get ratio: 40 ÷ 39 = 1:1
B. Step 2—Add the parts: 1+1 = 2
C. Step 3—Multiply the sum of the parts by the O2 flow rate: 10 2 = 20 L/min
BLENDERS
64. P. 849 Box 35-3
A. Confirm appropriate air and oxygen inlet pressure
B. Test alarms by disconnecting each gas source
C. Analyze at 100%, 21% and one other setting
PUT THAT CHILD IN A BOX!
65. Frequent opening and closing causes wide swings in the FIO2. P. 849
66. 40%-50% P. 849
67. It only covers the head and leaves the body free for nursing care. P. 849
68. 7 L/min to prevent accumulation of CO2. P. 849
69. May generate harmful noise levels. P. 849
70. Increases oxygen consumption and may cause apnea. P. 850
71. Oxygen hood. P. 850
72. Helps maintain a neutral thermal environment. P. 850
HBO
73. P. 853
Chamber
A. Monoplace
B. Multiplace
74. P. 855 Box 35-6
Acute
O2 Delivery
Cylinder is filled
Patient wears mask
Patient
One only
Up to 12
Chronic
Copyright © 2004 Mosby, Inc. All rights reserved.
Staff
Outside
Inside
6
A. Decompression sickness
Enhanced wound healing
B. Air or gas embolism
Refractory
osteomyelitis
C. Carbon monoxide poisoning
Radiation necrosis
75. History of unconsciousness, presence of neuropsychiatric abnormalities, cardiac instability,
carboxyhemoglobin 25% in adults (lower in kids and pregnant women). P. 855 Box 35-7
WHAT ELSE COULD THERE BE?
76. P. 855,858
Gas
A. NO
Indications
ARDS
Persistent pulmonary hypertension of the newborn
B. Helium
Acute airway obstruction of various causes
Postextubation stridor in pediatric settings (and croup)
77. Oxygen. Usually 80% helium, 20% oxygen. P. 858
78. Low density. P. 858
79. Nonrebreathing mask. P. 858
CASE STUDIES
Case 1
80. Borderline saturation for a cardiac patient, but meets minimum criteria. Tachycardia may
indicate cardiac dysfunction and definitely indicates increased cardiovascular work.
81. In spite of the SPO2, the patient should be placed on oxygen. The AHA recommends 4 L via
nasal cannula.
Case 2
82. Increased respiratory rate and tidal volume.
83. Increased rate, volume, and minute ventilation decrease the delivered FIO2.
84. Pulse oximeter and clinical signs.
Case 3
85. The system is not delivering enough flow to meet the patient’s needs. The FIO2 will not be
delivered.
86. A reservoir on the expiratory side.
87. Use two nebulizers in tandem.
88. 1:1
89. 24 L/min.
BOARD EXAM BROADSIDE
90. D. inadequate preoxygenation
91. D. Reduce the flow to 2 L/M and obtain an ABG
92. B. Oxygen hood
93. C. Increase the flow to the mask
Copyright © 2004 Mosby, Inc. All rights reserved.
7
94. D. Nonrebreathing mask
95. D. 18L
96. B. 32 L/M
97. C. Increased flowrate
98. B. 2L/M
FOOD FOR THOUGHT
99. The device only delivers about 70% oxygen at best. Many clinicians believe that a patient is
receiving the maximum amount of oxygen when they are not. A better system when 100% is
needed is a nonrebreathing reservoir circuit.
100. The AEM produces dry gas without the mist that might produce bronchospasm.
Copyright © 2004 Mosby, Inc. All rights reserved.