Betty has trouble breathing… - NC-NET
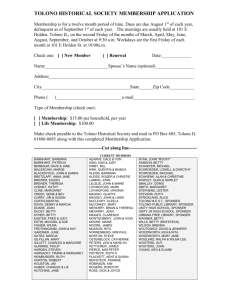
advertisement

Concept: Ethics NUR 212 Respiratory Issues (Acute respiratory Failure) As you are reading this case study, please highlight all of the ‘issues’ you identify. Afterwards please identify which 3 issues you believe to be the most important and provide rationale as to why. Betty has trouble breathing… Betty is a 64 year old woman with a history of COPD, CAD, and HTN. She developed shortness of breath and her breathing had become increasing more labored and shallow over the course of a few hours. Despite oxygen administration by mask (non-rebreather), her oxygen saturation continued to fall and presently 84% with a respiratory rate of 42/m. Her lungs are very dim to auscultation and you question whether she is moving any air at all despite her rapid respiratory rate. Respiratory therapy attempts to assist her respiratory system with CPAP but she does not improve. ABG’s were drawn and the values were: pH 7.58, PaO2 76, PCO2 29, HCO3 28, Sat 81%. She adamantly tells the nursing staff that she DOES NOT want to be put on a ventilator even though it is the only measure that has the possibility saving her life. Betty’s family practice MD (finally) shows up and is updated by the nursing staff regarding what is currently going on with the patient and her wishes of not being ventilated. He goes in & talks with the patient…Steve, one of the nurses on the unit, overhears him tell Betty that she will “only have to be on the ventilator overnight…to give her lungs a chance to rest”. Betty then reluctantly agrees to be placed on the ventilator. Steve talked to his co-worker Anna about the situation and they decide that they need to clarify with the physician to make sure that he understands that in her condition the possibility of her getting extubated in the morning is highly unlikely. They question the ethics behind doing this when earlier she adamantly refused this treatment. The physician thanks Steve and Anna for their concern, tells them that in his opinion Betty was not mentally clear enough to make life and death decisions about her care and then calls the ER to see if the MD can come up to intubate Betty. Although Steve and Anna voice their perception that Betty is cognitively able to make decisions, they know that no matter what they do Betty is about to be intubated and go in to get things ready. While in the room they again ask Betty if she is okay with her decision. Since both had worked in nursing for several years, her response didn’t surprise either one of them…she said, “My doctor promised me it would only be overnight and I believe him, He is doing everything he can for me. Why would he do anything that isn’t in my best interest?” Through an unspoken agreement, they both decide that to try to talk to her again would be in vain and possibly cause a problem with her physician so they keep their thoughts to themselves. Developed by Carol Thorn, RN, MS May use with permission for the purposes of nursing education If questions/comments, please contact Carol Thorn at cathorn1123@aol.com Steve and Anna talk to Betty’s daughter, Debbie, when she comes to visit a few hours later. She is so glad that the doctor “talked her mother into being put on the breathing machine” and she is going to do everything to keep her on it until her mother can breathe on her own again. Steve is very forthright with Debbie, telling her that with all of her previous medical problems, Betty may never be able to breathe on her own again and that Betty was adamant prior to the intubation about only wanting to be on the ‘machine’ overnight. Debbie just pats Steve’s hand, thanks him for his opinion but tells him in no uncertain terms that she will now decide when her mother comes off the machine. In the three weeks following her intubation for acute respiratory failure, Betty’s respiratory status improves, but only slightly, despite setbacks that occurred. Daily chest x-rays began by showing scattered infiltrates…she then developed ventilator acquired pneumonia (VAP) which progressed to Acute Respiratory Distress Syndrome (ARDS). Despite improvement in her respiratory status, all attempts to wean her off of the ventilator have failed. ABG’s done during weaning trials show mild acid-base imbalances as well as poor oxygenation. Her respiratory rates increase into the 30’s and she needs to be placed back on the ventilator after approximately 20-30 minutes. Despite Betty’s objections, the daughter signed the consent for a tracheotomy (as the last ditch effort to help remove her from the ventilator). That procedure is scheduled day after tomorrow. Betty is able to communicate with the nursing/medical staff and her daughter by writing notes and mouthing words. Over and over, she begs everyone to take her off of the machine and let her die. She acknowledges that she doesn’t want to live on the machine any longer and knows if she comes off the ventilator she will die. She doesn’t know why her daughter is making her suffer and doesn’t anyone realize what she is going through? Her notes are heartbreaking and soon the nursing staff members caring for her absolutely believe that they are torturing her each and every day she remains on the ventilator. When her physician is confronted by the nursing staff (with Betty’s notes in hand) he responds by saying that while he empathizes with Betty and the nursing staff’s discomfort, if he extubates Betty and she dies…her daughter will be alive to litigate. Based on that comment, the next morning the nursing staff of the unit make the decision to call the Ethics Committee at the hospital to help Betty. They inform the Committee Chair about: Betty’s handwritten notes, the physician’s response to their concerns, the fact that she continually tries to pull out her endotracheal tube (ETT) so needs to be restrained rather tightly. In fact, she has actually successfully pulled out her ETT on two different occasions (rapid response was called each time to reintubate). They add that they don’t believe that someone who is cognitively aware should have her wishes ignored because the physician is afraid of litigation by the family. The Ethics Committee reviews the chart and talks to Betty. They agree that she is of sound mind and is capable of making decisions regarding her own care but they hesitate to Developed by Carol Thorn, RN, MS May use with permission for the purposes of nursing education If questions/comments, please contact Carol Thorn at cathorn1123@aol.com extubate Betty until they can talk to the daughter. Later that day, Debbie comes to the hospital (with her attorney) stating that she is ready to file suit if they extubate her mother before allowing her every opportunity to get off of the ventilator. The doctors have told her that a tracheotomy will help wean Betty from the ventilator and she demands that they wait to make the decision to remove ventilatory support until all efforts have been attempted. The Ethics Chair and Debbie are able to strike a compromise. The order to extubate will not be written until weaning attempts after the trach prove to be unsuccessful but if Betty should pull her ETT out again, the rapid response team will not be called nor will Betty be re-intubated. When the Ethics Committee and Debbie go into Betty’s room to talk to her, it was evident that Betty was not pleased with their decision. She wrote a note and told them all “to get the hell out of my room and don’t ever come back until you agree to let me die”. When Debbie tries to soothe her mother, despite being restrained Betty attempts to throws her Kleenex box at her and turns her head toward the wall. Debbie tightens the wrist restraints to the bed and leaves saying that her mother will appreciate this later. The next night, Steve and Anna are working in the unit together. In report they hear that if Betty’s wrists are untied she immediately tries to extubate herself. Betty is scheduled for a tracheotomy in the morning and that Debbie told the day shift nurses that her plan is to transfer Betty to a skilled facility in the next 2-3 days where she will be able to live with ventilator assistance. The Ethics Committee was called but they state due to the prior agreement, they cannot intervene until after the trach. When Steve and Anna go into Betty’s room, the hurt and emotion in her eyes takes them both by surprise. She tries to mouth words to them but they are unable to determine what she is trying to say. She was becoming increasingly frustrated so, even though they know better, they untied her wrists for a moment so that she can write them a note. She does not try to extubate herself…instead she writes them a note that chills them both to the core. Her note said “Why did you let this happen to me? I trusted you to help me but you let that doctor lie to me and now I live connected to a torture machine. I’ve heard all of you nurses talking out there…you all knew from the beginning that I wouldn’t get off this damn machine…why didn’t you tell me you didn’t agree with my doctor that night they put me on this thing? You just came in my room and asked me if I was ‘okay’ with my decision. Why did you say that? What was the purpose if you weren’t going to help me make a better decision? Now they are going to put a hole in my throat and I’m going to have to live on this thing in a nursing home until I get pneumonia and pray that it kills me quickly. I used to be mad at both of you but now I know that you are as sad as I am about this…well maybe not as much as I am but I know that you feel bad. Please promise me that you will never let another doctor do this to anyone ever again. Nurses are the ones that really CARE about and for the patients… people respect you so much. Stand up for your patients and earn their respect.” As Steve and Anna read the pages & pages of words that Betty was writing, tears were streaming down both of their faces. They both knew that they had failed Betty and that she was suffering every day because they did not advocate strongly enough for her in the Developed by Carol Thorn, RN, MS May use with permission for the purposes of nursing education If questions/comments, please contact Carol Thorn at cathorn1123@aol.com first place. Just like that fateful night Betty was intubated, Steve and Anna looked at each other and came to an agreement although no words were spoken. They told Betty it was time to reposition her so Steve went to get some morphine and ativan to pre-medicate her. After the medication was given, they turned Betty on her side, retied her wrists loosely and walked out of the room. A few minutes later, ventilator alarms were ringing in Betty’s room. When they reached her room, they saw that Betty had extubated herself…on her clipboard was a note…all it said was…”To my angels…thank you for caring… goodbye”. Developed by Carol Thorn, RN, MS May use with permission for the purposes of nursing education If questions/comments, please contact Carol Thorn at cathorn1123@aol.com