A Trial of Darbepoetin Alfa in Type 2 Diabetes and Chronic Kidney
advertisement

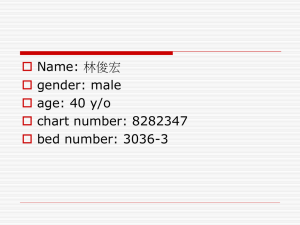
A Trial of Darbepoetin Alfa in Type 2 Diabetes and Chronic Kidney Disease: Trial to Reduce Cardiovascular Events with Aranesp Therapy (TREAT) Study Pfeffer M, Burdmann E, Chen C, et al. N Engl J Med 2009;361:2019-32. Reviewed by: Gardy Mak Purpose Background Primary Endpoints Secondary Endpoints Study Design Study Population Exclusion Criteria To determine if darbepoetin alfa reduces the risk of cardiovascular and end-stage renal disease in patients with DMII, CKD, and anemia Type II diabetes is one of the leading causes of chronic kidney disease Chronic kidney disease has many complications including cardiovascular disease and anemia Anemia in chronic renal failure o Decreased erythropoietin synthesis in the kidneys o Erythropoietin is responsible for RBC development and maturation from precursors in the bone marrow o Majority of this hormone is produced in the kidneys Red blood cell transfusions o Iron overload o Volume overload o Infection Recombinant human erythropoietin: Erythropoiesis-stimulating agents (ESAs) o Increase Hgb levels o Eliminates need for continuous transfusion o Common SE: hypertension, edema, fatigue, hypotension, and headache o Epoetin alfa (Epogen, Procrit) o Darbepoetin alfa (Aranesp) Type II diabetes, CKD, and anemia can all individually increase the risk of cardiovascular and end-stage renal disease Composite outcome of death or cardiovascular event (nonfatal MI, CHF, stroke, or hospitalization for MI) Composite outcome of death or end-stage renal disease Time to death Death from cardiovascular causes Rate of decline in the estimated GFR Changes in patient-reported outcomes at week 25 o FACT-Fatigue score o 36-Item Short-Form General Health Survey questionnaire Randomized Double-blind Placebo-controlled 623 sites in 24 countries Event driven Median follow-up duration of 29.1 months DMII CKD (eGFR of 20-60 ml/min/1.73 m2) not on dialysis Anemia (Hgb ≤ 11.0 g/dL) Transferrin saturation of 15% or more Uncontrolled hypertension Previous kidney transplantation or scheduled kidney transplant Current IV antibiotics, chemotherapy, radiation Cancer HIV Active bleeding Hematologic disease Pregnancy History of cardiovascular event, seizure or major history Treatment (N = 4038) Statistical Analysis Patient Population Results ESA in the last 12 weeks prior to randomization Darbepoetin alfa group: N = 2012 o 12 different strengths o Point-of-care device to select dose using computer algorithm o Adjust dose to maintain Hgb at ~13.0 g/dL Placebo group: N = 2026 o Matching pre-filled syringes o Rescue darbepoetin alfa if Hbg < 9.0 g/dL o Return to placebo once ≥ 9.0 g/dL Hgb levels and vital signs measured every 2 weeks during titration period then monthly Event driven, 1203 cardiovascular composite events required to provide 80% statistical power to detect a 20% risk reduction o Two-sided type I error of 0.048 Primary and secondary outcomes o Intention-to-treat analysis Hazard ratios with 95% confidence intervals o Cox proportional-hazards model Patient reported outcomes o Last-observation-carried forward method o T-tests Baseline characteristics were similar between groups o Age, history of CAD, stroke, peripheral arterial disease, MI, Hgb level, and cardiovascular disease medications History of heart failure more predominant in the placebo group than darbepoetin alfa group (35.2% and 31.5% respectively, unadjusted P = 0.01) Hemoglobin levels from baseline and end of treatment were measured o Darbepoetin alfa: Median Hgb 12.5 g/dL (interquartile range, 12.0 to 12.8) o Placebo: Median Hgb 10.6 g/dL (interquartile range, 9.9-11.3, P<0.001) Red-cell transfusions o Darbepoetin alfa: 297 patients (14.8%) o Placebo: 496 patients (24.5%) [hazard ratio 0.56, 95% CI, 0.49 to 0.65, P<0.001] Primary Outcomes Endpoint Darbepoetin Alfa (N=2012) Cardiovascular 632 (31.4) composite endpoint Stroke 101 (5.0) Renal composite endpoint ESRD Placebo (N=2026) Hazard Ratio (95% CI) P Value NNH 602 (29.7) 1.05 (0.941.17) 0.41 59 53 (2.6) 1.92 (1.3802.68) 1.06 (0.951.19) 1.02 (0.871.18) <0.001 42 0.29 53 0.83 200 652 (32.4) 618 (30.5) 338 (16.8) 330 (16.3) Secondary Outcomes FACT-Fatigue score o Only assessed patients with both baseline and week-25 scores o Darbepoetin alfa: 963 of 1762 patients (54.7%) had an increase of 3 or more points o Placebo: 875 of 1769 patients (49.5%) o P=0.002 o NNT=20 Conclusion Short-Form General Health Survey o No significant difference between groups Darbepoetin alfa significantly increased Hgb levels and had clinical benefits in improving fatigue score compared to placebo Fewer transfusions required in the darbepoetin alfa group than the placebo group However, darbepoetin alfa did not demonstrate significant effect in reducing cardiovascular events and the time to end stage renal disease in comparison to placebo Instead, there is an increase in one of the cardiovascular components when Hgb target is 13 g/dL o Higher incidence of stroke in the darbepoeitin alfa group (5% vs 2.6% in the placebo group) Pts with DMII, CKD and anemia not on dialysis are not likely to benefit from ESAs at a Hgb of 13 g/dL Long-term study Randomization Blinding Multinational, multicenter Large sample size Higher Hgb target than current recommended goal of 10 to 12 g/dL (FDA, 2007 update) and 11 to 12 g/dL (National Kidney Foundation Dialysis Outcomes Quality Initiative) in patients treated with darbepoetin alfa o Uncertain whether the Hgb level or ESA use is causing the increase stroke incidences Baseline imbalances Baseline Hgb was 10.4 and 10.5 in darbepoetin alfa and placebo group, respectively Rate of darbepoetin alfa adjustment not specified Funded by Amgen, a company that manufactures Aranesp Correction of Hemoglobin and Outcomes in Renal Insufficency (CHOIR) study o Similar patient population o Discontinued prematurely due to increase cardiovascular events in the higher Hgb group Current guidelines recommend darbepoetin alfa use in patients with anemia and CKD o FDA indication: patients with CRF not on dialysis should have a Hgb less than 10 g/dL prior to starting treatment Studies show that ESAs might increase mortality and disease progression in patients with certain cancers and anemia o June 2008 European Medicines Agency recommended blood transfusions over ESAS in cancer patients on chemotherapy and expected to live reasonably long o FDA mandated changes to ESA indications: ESAs are not indicated in patients on myelosuppressive agents if cure is the expected outcome Strengths Limitations Clinical Relevance NEPHRODIAB2: ongoing clinical trial comparing target Hgbs level in patients with DMII, CKD, and anemia Schrier, Stanley et al. Role of erythopoiesis-stimulating agents in the treatment of anemia in patients with cancer. UpToDate. Jan 2010. http://www.uptodate.com.proxy.westernu.edu/online/content/topic.do?topicKey=genl_onc/14286&selectedTitle=1~150&source=search_resu lt#H14 Berns, Jeffrey. Anemia of chronic kidney disease: Target hemoglobin/hematocrit for patients treated with erythropoietic agents. UpToDate. Feb 2010. http://www.uptodate.com.proxy.westernu.edu/online/content/topic.do?topicKey=dialysis/36521&source=see_link#H10 Pham, David. PHRM 6202 Pharmacy Practice II: Anemia Lecture. Sept 2008. Darbepoetin. Lexicomp. http://online.lexi.com.proxy.westernu.edu/crlsql/servlet/crlonline