Stem Cell Transplant & Leukemia Fact Sheet
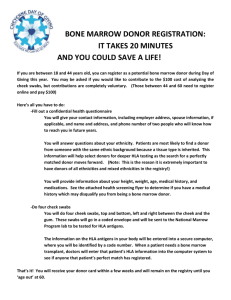
advertisement

JUST THE FACTS... LEUKEMIA Leukemia is a malignant cancer affecting the bone marrow and blood. All leukemias develop from a cell in the bone marrow, which undergoes a genetic change causing it to grow and multiply out of control. These leukemia cells eventually crowd out normal cells in the marrow. According to the Canadian Cancer Society, an estimated 4,200 Canadians were diagnosed with leukemia in 2007. Within five years, nearly 2,000 of those people will die of their illness. There are several types of leukemia. These can be divided into categories: myelogenous or lymphocytic (based on the type of blood cell affected); acute or chronic (based on the speed of progression of the disease). Acute leukemias develop rapidly and tend to grow aggressively, thus treatment is generally much more urgent than for chronic leukemias. The most common type of acute leukemia affecting adults is acute myelogenous leukemia (AML), of which there are several subtypes. The most common adult leukemia overall is chronic lymphocytic leukemia (CLL). Other common types include acute lymphocytic leukemia (ALL) and chronic myelogenous leukemia (CML). According to the Canadian Cancer Society, there were 957 new cases of AML in Canada in 2004 (versus 307 cases of ALL, 397 cases of CML, and 1786 cases of CLL). The prognosis for patients with AML depends on many factors, including the age of the patient, the subtype of AML, the specific genetic changes in the cancer cells, and the response of the disease to initial treatment. Treatment of AML is individualized for each patient, and can involve one or more of: (a) chemotherapy, (b) radiation therapy, and (c) stem cell transplantation. Stem cells in the bone marrow are cells that can generate all types of mature blood cells: red cells (which carry oxygen to the body), white cells (which help to fight infections), and platelets (which are involved in blood clotting). In many patients with AML, especially if initial chemotherapy is not effective, stem cell transplant may be the only way to cure the disease. _____ STEM CELL TRANSPLANT In order to perform a bone marrow transplant, a suitable donor must be found. (Note that gender is not important: men can donate stem cells to women and vice versa) All cells in the body carry special markers on their surface that tell the body that they belong to itself, and are not "foreign" and therefore not rejected. Those markers found on bloodforming stem cells are called "human leukocyte antigens" (HLA). We all have 6 pairs of major classes of HLA markers on our cells. Each person inherits one of each pair from each parent. There are dozens of variations of each of these markers, and therefore millions of potential combinations of all six. This is why it can be difficult to find a perfect match for a patient in need of transplant. Three pairs of markers (HLA-A, -B, and -DR) are initially screened and recorded in the database. If a match is found based on these, the others markers are tested more closely. Because we inherit half of our HLA markers from our mother and half from our father, each brother and sister who has the same parents has a 25% chance of matching. It is unlikely that extended family members will match. However, parents and/or children may also be tested to confirm HLA typing and to make sure no possible donors are overlooked. A close HLA match improves the chances for a successful transplant. Close matching: (a) promotes engraftment (when the donated cells start to grow and make new blood cells); and (b) reduces the risk of a post-transplant complication called graft-versus-host disease (GVHD). GVHD occurs when the immune cells from the donated marrow (the graft) attack the recipient's cells (the host). About 70% of patients who need a transplant do NOT have a suitable donor in their family. If there is no related donor, doctors will search national and international bone marrow donor registries for potential matched unrelated donors. Bone Marrow Donors Worldwide (BMDW) is a collective database of 59 stem cell donor registries from 43 countries (including Canada), and 40 cord blood banks from 25 countries; 12,441,390 potential donors and cord blood units were available as of August 26, 2008. A very small registry in India (Asian Indian Donor Marrow Registry) also participates in this program, but has only about one thousand registrants so far. _____ HOW TO REGISTER TO DONATE The process of registering to becoming a potential donor in Canada is free, simple, and completely non-invasive. In Canada, Canadian Blood Services (CBS) operates "OneMatch" (www.onematch.ca), the national database of stem cell donors. Much of the following information about registration and donation is taken from their website. Anyone between the ages of 17 and 50 who is in good general health can join. To register, visit www.onematch.ca and fill out the online registration form. If joining online is not possible, call 1-888-2-DONATE (1-888-236-6283) to have a registration package mailed to you. After receiving general registration information, OneMatch will contact you to ask further questions and to discuss the donation process. You will then be mailed a kit containing four swabs; simply use them to swab four areas inside your mouth (between your cheeks and gums), and mail the swabs back to CBS in the pre-paid envelope. Detailed instructions are included with the swab package. OneMatch will use the skin cells on the swabs to genetically test for your HLA types. These test results will be entered into the national database, and your information will be included when physicians search for possible donors for patients in need. You may obtain a copy of your own test results by e-mailing a request to ati@blood.ca (Access To Information Office). OneMatch conducts database searches to find a donor whose HLA markers match that of the patient in need of a stem cell transplant. In the event that you come up as a likely match, OneMatch will contact you. If you agree to proceed (you are free to decline at any point), further blood tests will be scheduled to determine the full extent of your compatibility and to test for transmissible diseases (such as HIV, hepatitis B/C, etc). Your health will be thoroughly assessed to make certain that you can safely proceed and to ensure that your health background does not pose a risk to the patient. If you are selected to donate, you will be guided through this process by a case manager. The case manager will conduct an assessment over the phone, then a transplant physician will perform a thorough physical assessment at the collection centre (the hospital where you will donate stem cells) closest to you. You will also be tested to confirm that you have no infectious diseases. Once it is determined that you are medically eligible and you agree to proceed, the patient will be notified and the elimination of his or her diseased bone marrow will begin. _____ THE DONATION PROCESS It is important to understand that donating stem cells is NOT like donating an organ (such as a kidney or liver). It is much more similar to donating blood: it involves very little pain; it is a short, minimally-invasive procedure; and there are no significant complications. Stem cells are generally collected using one of two methods: peripheral blood stem cell (PBSC) collection, and bone marrow harvest. In Canada, PBSC collection (the easier of the two methods) is now used more than 60% of the time. For a PBSC donation, a donor receives injections of a hormone called “granulocyte colony stimulating factor” (G-CSF) for a minimum of four days. These injections increase the number of stem cells found in the blood. To collect these cells, the donor is connected to an apheresis machine with a needle. Blood is drawn through a tube into a centrifuge and there the stem cells are collected and the remaining blood components are returned to the donor through another needle (see diagram below). This procedure takes 1-2 hours, is essentially painless, does not require anaesthetic, and there is no recovery time needed. Bone marrow stem cell donation is a surgical procedure performed under anaesthesia in an operating room. The collection physician will use special, hollow needles to withdraw liquid marrow from the back of your pelvic (hip) bones, not from the spine (see diagram below). Normally, about a litre of fluid is taken altogether. The procedure usually lasts from 45-90 minutes, and donors are normally discharged from the hospital the same day. You can expect to feel some soreness in the back of your hips for a few days or longer. Most donors are back to their normal routine in a few days. Your marrow is completely replaced within four to six weeks. Everyone's pain tolerance is different, but most bone marrow donors report that any discomfort they feel is easily managed with pain medication that is ordered for them if required. Many donors report very little discomfort. Stem cells are harvested on the same day as transplantation, with the intent to infuse the recipient within 24 hours of the harvest. The harvested stem cells are filtered and given to the recipient intravenously. Generally, donors are kept anonymous from the recipient until one year after transplant. At this time, identifying information can be exchanged if mutually desired. _____ MINORITY UNDER-REPRESENTATION IN THE REGISTRY While the urgent stimulus for this donor recruitment drive comes from the need of one member of our community, registering for the stem cell donor database also has the potential to save the lives of thousands of people around the world. It is especially imperative for members of the South-Asian community to register, as we are extremely under-represented within the database. In other words, although South-Asians represent a significant proportion of the general population, members of our community in need of a bone marrow transplant are much less likely to find a donor. According to the U.S. National Cancer Institute, among different ethnic groups, the probability of finding a good match is, from the highest to lowest, Japanese (99%), North American Caucasian (93%), African American and Asian (50%). Please note that even if you are not eligible to donate stem cells due to your age or health, you can still help by making a financial contribution to organizations such as Canadian Blood Services and the Canadian Cancer Society. _____ SOME INFORMATIVE WESITES Leukemia information: http://www.leukemia-lymphoma.org/all_page?item_id=7026 Canadian Cancer Society: http://www.cancer.ca/ Information about stem cells and cancer (U.S. National Cancer Institute): http://www.cancer.gov/cancertopics/understandingcancer/stemcells Canadian bone marrow donation: http://www.onematch.ca/ U.S. bone marrow donation: http://www.marrow.org/ Indian bone marrow donation: http://www.matchpia.org/ International stem cell donor database: http://www.bmdw.org/ Toronto Star article about Dr. A. Guha: http://www.thestar.com/article/486109 Vancouver Sun article about Dr. A. Guha: http://www.canada.com/vancouversun/news/westcoastnews/story.html?id=2e06ae41-99a4-436c88ac-b5b2141b152d Dr. A. Guha’s lab website: http://www.sickkids.on.ca/Guha/default.asp