Helpful Information - 25 Percent ME Group
advertisement

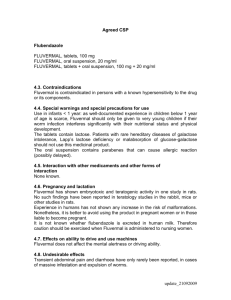
USEFUL INFORMATION A Cautionary Tale I've been bedridden with ME for 14 years, ill for longer. Among the many symptoms to surface has been intermittent chest pain which, having spoken to other ME sufferers, I assumed was yet another on the long list of things we have to put up with! I've also been getting more and more exhausted in recent months. I put this down to worsening of the illness and to my age (I'm 68). In March of this year, the chest pains became more frequent and more severe, so I reluctantly rang my GP and he immediately sent for an ambulance. Things happened so quickly after that, it hardly registered! I'd had a small heart attack and was still getting chest pain, in spite of being given maximum medication. 24 hours after being admitted to hospital I was rushed to Harefield hospital where I had an immediate angiogram. This revealed that I had 4 blocked arteries, and 5 days later I had an emergency bypass operation. I'm writing this just to say to other ME sufferers, please don't assume that every symptom you get can be attributed to ME/CFS – particularly chest pain. It's 3 months since my surgery and I'm doing well. I still have ME, of course, but as I recover from the operation, I find I am much less fatigued, can walk for 100 steps or more several times a day, and can converse more easily. I hope this will be useful to those of you experiencing strange symptoms. Christine (So glad you received the surgery so quickly and that you are making good progress – the Ed) Helped By Nimodipine/Nimotop I AM NO LONGER HOUSEBOUND since I have been taking Nimodipine/Nimotop. When I heard of a Scottish doctor who took the drug and was able to resume her practice, I began to find out more. In M.E. research, brain scans have shown poor blood flow in the brain, and it is proposed that there is an abnormality in the ion channels of the cell membranes. Nimodipine is a calcium channel blocker that increases blood flow to the brain and is used in Europe to treat cognitive impairment. Nimodipine is used to treat M.E. in Canada and the USA. It increases mental clarity, reduces pain and fatigue, and improves exercise tolerance. One side-effect may be low blood pressure or a drop of pressure upon standing, so regular monitoring is advised. My GP allows me to do this at home with a blood pressure cuff from Argos. Begin treatment with 1/2 of a 30mg tablet each morning. Improvement may be seen after four days. If there is no improvement, gradually increase the dose every two weeks up to four tablets a day, spaced evenly morning, noon, and evening. After improvement is seen, step-down the dosage to see if it can be maintained. Nimodipine is not licensed for the treatment of M.E. in the U.K. but a doctor may give a private prescription for it. A private prescription for 20 30mg tablets costs the patient about £12; 56 costs £26; 100 costs £46. The best prices I have found are from Boots Pharmacy Direct. Contact them on 0845-121-9040 or www.boots.com. Before I took Nimodipine I was largely housebound with M.E., needing a nap every day to repair mental and physical fatigue and muscle pain. I saw sudden improvement when I reached 1 1/2 tablets a day. I felt even better on 2 tablets a day, but lost the benefit when I decreased the dose. I am now taking 2 1/2 tablets day and my health is no longer incredibly fragile. I still need to balance my activities and have recovery time if I over-step the new limits, but I can go out multiple times in the week and walk further distances. On my best days I would say my condition is 1/3 to 1/2 of "normal". I have references on the research and doctor's recommendations, so please feel free to contact me, enclosing an SAE. I wish you could all benefit as I have, but I know that people with M.E. have very individual responses to potential treatments. (We recommend you contact your GP before trying any treatment—The Ed) Hospital Travel Costs This is to help with the cost of your fares or petrol when you go into hospital for NHS treatment and when you come out of hospital; it also helps with the cost of your fares and petrol when you go to and from hospital as an outpatient for NHS treatment. You can get it if you get Income Support or Income Based Jobseeker’s Allowance. If you don’t you may be able to get help with travel costs through the NHS Low Income Scheme. If you need someone to travel with you, you may also be able to get help with the cost of their fares.